Korean J Ophthalmol.
2019 Oct;33(5):399-405. 10.3341/kjo.2019.0049.
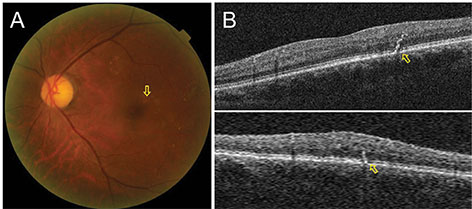
New Method of Quantitative Analysis of Hard Exudate Using Optical Coherence Tomography: Application in Diabetic Macular Edema
- Affiliations
-
- 1Department of Ophthalmology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. H00398@paik.ac.kr
- 2Department of Ophthalmology, Hallym University Kangnam Sacred Hospital, Seoul, Korea.
- KMID: 2459520
- DOI: http://doi.org/10.3341/kjo.2019.0049
Abstract
- PURPOSE
In the present study, the volume of hard exudates (HEs) was quantitatively measured using optical coherence tomography (OCT) and the agreement and correlation with area of HEs in fundus photography were analyzed.
METHODS
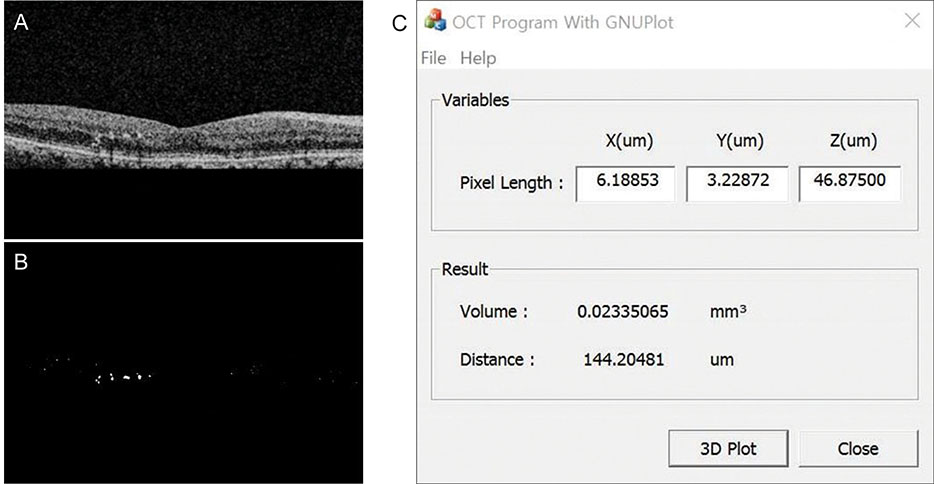
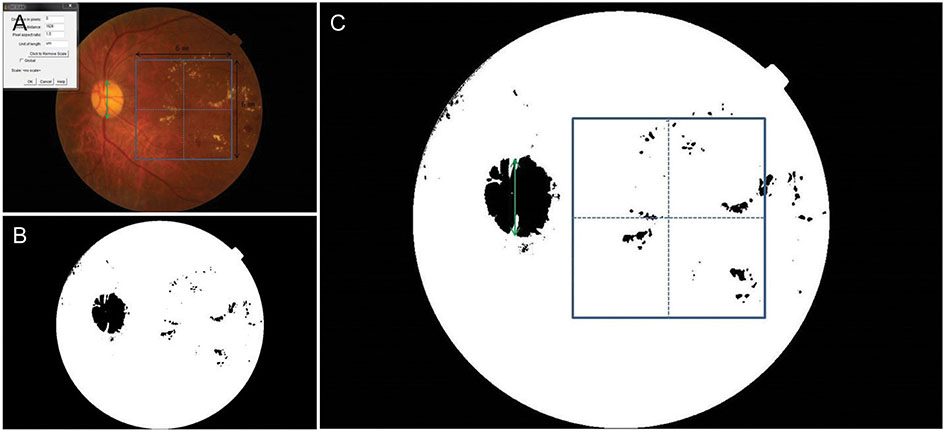
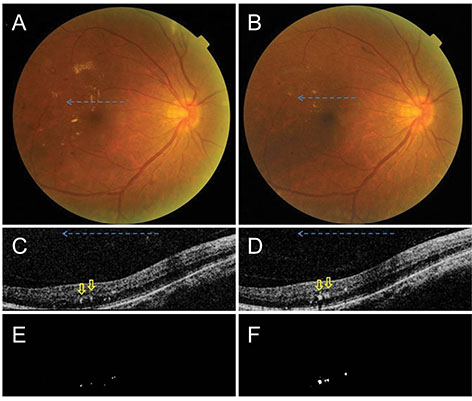
The medical records of patients with diabetic macular edema who underwent focal laser treatment and were followed up more than 3 months were retrospectively evaluated. An automated customized program designed for measuring HE volume was used. The HEs in each OCT B-scan binary image were measured using 512 × 128 pixels, 6 mm × 6 mm OCT cube scans. The volume was measured by summing the segmented HEs in each 128 B-scan image. The area was measured in 6 mm x 6 mm fundus photography. The volume and area were measured before and 3 months after the treatment. The agreement of increase and decrease in HEs, and the correlation of volume and area of HEs were analyzed.
RESULTS
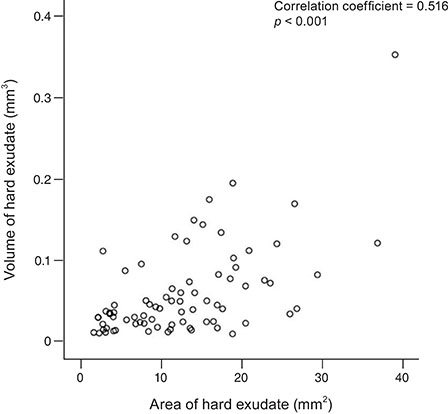
A total of 35 patients (39 eyes) were included in the study. The volume was significantly reduced from 0.07978 to 0.02565 mm³ at 3 months (p < 0.001). The area was also significantly reduced from 15.35 to 8.60 mm² at 3 months (p < 0.001). The volume was decreased in 34 eyes and increased in 5 eyes. The area was decreased in 37 eyes and increased in 2 eyes. A significant correlation between volume and area was found (p < 0.001) as well as agreement between increase and decrease in volume and area.
CONCLUSIONS
In the 3-dimensional quantitative volumetric analysis, the volume and area of HEs were correlated and the direction of increase and decrease was concordant. Considering the distribution of HEs in multiple layers of the retina, volumetric analysis could be considered a substitute for the analysis of HE area.
Keyword
MeSH Terms
Figure
Reference
-
1. Schachat AP, Wilkinson CP, Hinton DR, et al. Ryan's retina: volume 2 medical retina. 6th ed. St. Louis: Elsevier;2017. p. 1038.2. Klein R, Klein BE, Moss SE, et al. Wisconsin epidemiologic study of diabetic retinopathy. IV. Diabetic macular edema. Ophthalmology. 1984; 91:1464–1474.3. Csaky KG, Richman EA, Ferris FL 3rd. Report from the NEI/FDA Ophthalmic Clinical Trial Design and Endpoints Symposium. Invest Ophthalmol Vis Sci. 2008; 49:479–489.
Article4. Diabetic Retinopathy Clinical Research Network. Browning DJ, Glassman AR, et al. Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007; 114:525–536.
Article5. Grading diabetic retinopathy from stereoscopic color fundus photographs: an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991; 98(5 Suppl):786–806.6. Domalpally A, Ip MS, Ehrlich JS. Effects of intravitreal ranibizumab on retinal hard exudate in diabetic macular edema: findings from the RIDE and RISE phase III clinical trials. Ophthalmology. 2015; 122:779–786.7. Chew EY, Klein ML, Ferris FL 3rd, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch Ophthalmol. 1996; 114:1079–1084.8. Jeon S, Lee WK. Effect of intravitreal bevacizumab on diabetic macular edema with hard exudates. Clin Ophthalmol. 2014; 8:1479–1486.9. Shin YU, Hong EH, Lim HW, et al. Quantitative evaluation of hard exudates in diabetic macular edema after short-term intravitreal triamcinolone, dexamethasone implant or bevacizumab injections. BMC Ophthalmol. 2017; 17:182.
Article10. De Benedetto U, Sacconi R, Pierro L, et al. Optical coherence tomographic hyperreflective foci in early stages of diabetic retinopathy. Retina. 2015; 35:449–453.
Article11. Lammer J, Bolz M, Baumann B, et al. Detection and analysis of hard exudates by polarization-sensitive optical coherence tomography in patients with diabetic maculopathy. Invest Ophthalmol Vis Sci. 2014; 55:1564–1571.
Article12. Bolz M, Schmidt-Erfurth U, Deak G, et al. Optical coherence tomographic hyperreflective foci: a morphologic sign of lipid extravasation in diabetic macular edema. Ophthalmology. 2009; 116:914–920.13. Niu S, Yu C, Chen Q, et al. Multimodality analysis of hyper-reflective foci and hard exudates in patients with diabetic retinopathy. Sci Rep. 2017; 7:1568.
Article14. Framme C, Schweizer P, Imesch M, et al. Behavior of SD-OCT-detected hyperreflective foci in the retina of anti-VEGF-treated patients with diabetic macular edema. Invest Ophthalmol Vis Sci. 2012; 53:5814–5818.
Article15. Ota M, Nishijima K, Sakamoto A, et al. Optical coherence tomographic evaluation of foveal hard exudates in patients with diabetic maculopathy accompanying macular detachment. Ophthalmology. 2010; 117:1996–2002.
Article16. Lee H, Jang H, Choi YA, et al. Association between soluble CD14 in the aqueous humor and hyperreflective foci on optical coherence tomography in patients with diabetic macular edema. Invest Ophthalmol Vis Sci. 2018; 59:715–721.
Article17. Miura M, Makita S, Sugiyama S, et al. Evaluation of intraretinal migration of retinal pigment epithelial cells in age-related macular degeneration using polarimetric imaging. Sci Rep. 2017; 7:3150.
Article18. Pemp B, Deak G, Prager S, et al. Distribution of intraretinal exudates in diabetic macular edema during anti-vascular endothelial growth factor therapy observed by spectral domain optical coherence tomography and fundus photography. Retina. 2014; 34:2407–2415.
Article19. Davoudi S, Papavasileiou E, Roohipoor R, et al. Optical coherence tomography characteristics of macular edema and hard exudates and their association with lipid serum levels in type 2 diabetes. Retina. 2016; 36:1622–1629.
Article20. Sophie R, Lu N, Campochiaro PA. Predictors of functional and anatomic outcomes in patients with diabetic macular edema t reated with ranibizumab. Ophthalmology. 2015; 122:1395–1401.21. Jenkins AJ, Joglekar MV, Hardikar AA, et al. Biomarkers in diabetic retinopathy. Rev Diabet Stud. 2015; 12:159–195.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quantitative Analysis of Diabetic Macular Edema by Optical Coherence Tomography
- The Correlation between Visual Acuity and Patterns of Diabetic Macular Edema in OCT Images
- Risk Factors for Diffuse Diabetic Macular Edema as Classified by Optical Coherence Tomography
- Diurnal Variation of Macular Thickness in Diabetic Macular Edema
- Analysis of Postoperative Macular Edema in Cataract Patients with Diabetes using Optical Coherence Tomography