Prog Med Phys.
2019 Sep;30(3):65-73. 10.14316/pmp.2019.30.3.65.
Dosimetric Effects of Intrafractional Organ Motion in Field-in-Field Technique for Whole-Breast Irradiation
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. sg.ju@samsung.com, doho.choi@samsung.com
- 2Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2459445
- DOI: http://doi.org/10.14316/pmp.2019.30.3.65
Abstract
- PURPOSE
We evaluated the motion-induced dosimetric effects on the field-in-field (FIF) technique for whole-breast irradiation (WBI) using actual patient organ motion data obtained from cine electronic portal imaging device (cine EPID) images during treatment.
MATERIALS AND METHODS
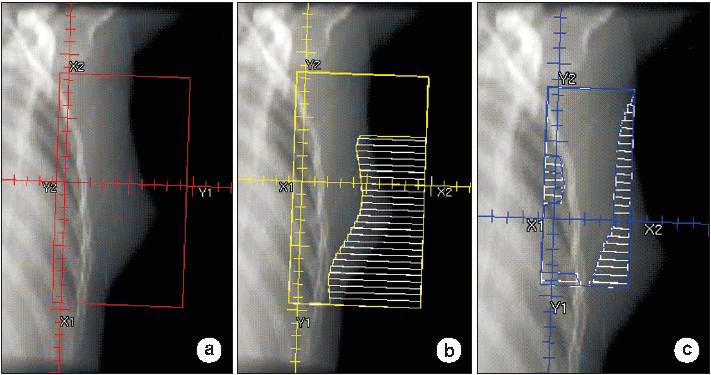
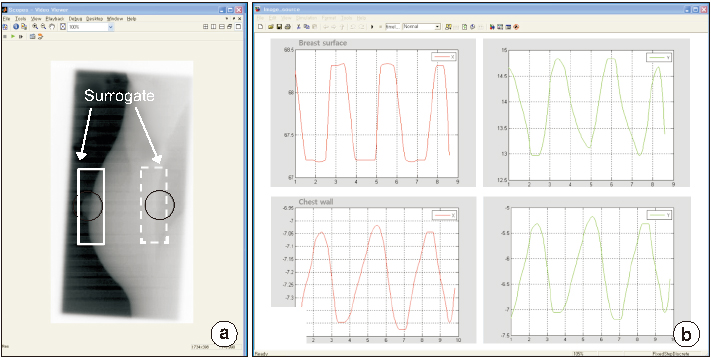
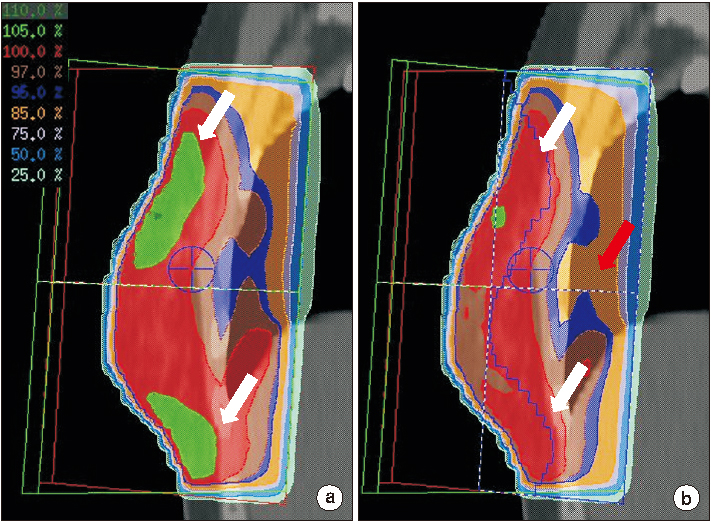
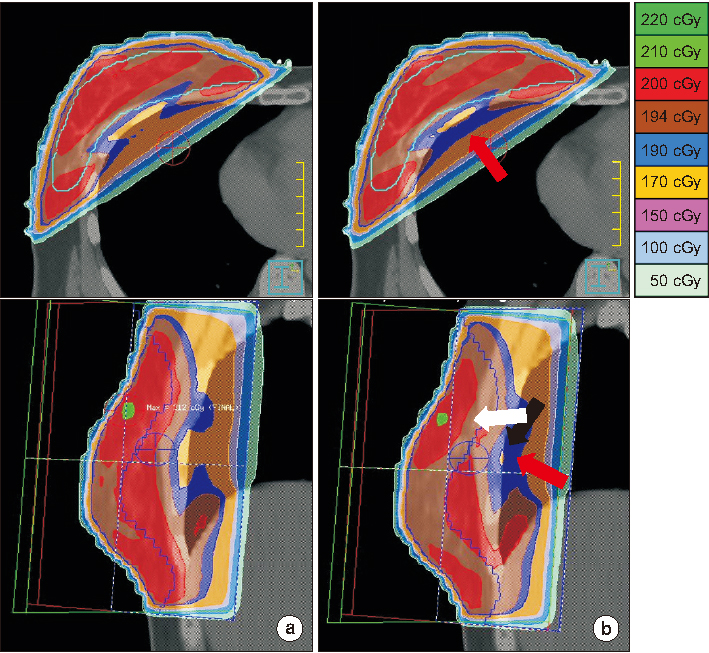
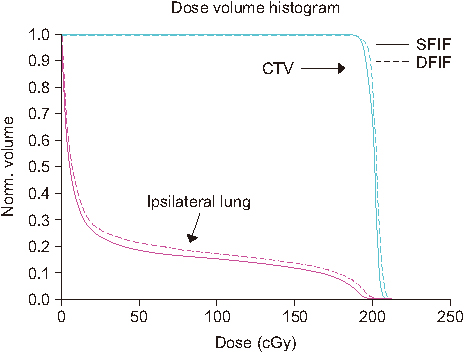
Ten breast cancer patients who received WBI after breast-conserving surgery were selected. The static FIF (SFIF) plan involved the application of two parallel opposing tangential and boost FIFs. To obtain the amplitude of the internal organ motion during treatment, cine EPID images were acquired five times for each patient. The outside contour of the breast (OCB) and chest wall (CW) contour were tracked using in-house motion analysis software. Intrafractional organ motion was analyzed. The dynamic FIF (DFIF) reflecting intrafractional organ motion incorporated into the SFIF plan was calculated and compared with the SFIF in terms of the dose homogeneity index (DHI(90/10)) for the target and Vâ‚‚â‚€ for the ipsilateral lung.
RESULTS
The average motion amplitudes along the X and Y directions were 1.84±1.09 mm and 0.69±0.50 mm for OCB and 1.88±1.07 mm and 1.66±1.49 mm for CW, respectively. The maximum motion amplitudes along the X and Y directions were 5.53 and 2.08 mm for OCB and 5.22 and 6.79 mm for CW, respectively. Significant differences in DHI(90/10) values were observed between SFIF and DFIF (0.94 vs 0.95, P<0.05) in statistical analysis. The average Vâ‚‚â‚€ for the lung in the DFIF was slightly higher than that of the SFIF in statistical analysis (19.21 vs 19.00, P<0.05).
CONCLUSION
Our findings indicate that the FIF technique can form a safe and effective treatment method for WBI. Regular monitoring using cine EPID images can be effective in reducing motion-induced dosimetric errors.
Figure
Reference
-
1. International Agency for Research on Cancer (IARC) and World Health Organization (WHO). GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide 2012. Available at: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.2. Blichert-Toft M, Rose C, Andersen JA, Overgaard M, Axelsson CK, Andersen KW, et al. Danish randomized trial comparing breast conservation therapy with mastectomy: six years of life-table analysis. Danish Breast Cancer Cooperative Group. J Natl Cancer Inst Monogr. 1992; 19–25.3. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347:1233–1241.
Article4. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002; 347:1227–1232.
Article5. Fisher B, Anderson S, Redmond CK, Wolmark N, Wickerham DL, Cronin WM. Reanalysis and results after 12 years of follow-up in a randomized clinical trial comparing total mastectomy with lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1995; 333:1456–1461.
Article6. Taylor ME, Perez CA, Halverson KJ, Kuske RR, Philpott GW, Garcia DM, et al. Factors influencing cosmetic results after conservation therapy for breast cancer. Int J Radiat Oncol Biol Phys. 1995; 31:753–764.
Article7. Park W, Huh SJ, Yang JH, Nam SJ, Kim JH, Choi JY, et al. The implication of hot spots on bone scans within the irradiated field of breast cancer patients treated with mastectomy followed by radiotherapy. Ann Nucl Med. 2008; 22:685–691.
Article8. Oliver M, Chen J, Wong E, Van Dyk J, Perera F. A treatment planning study comparing whole breast radiation therapy against conformal, IMRT and tomotherapy for accelerated partial breast irradiation. Radiother Oncol. 2007; 82:317–323.
Article9. Prabhakar R, Haresh KP, Julka PK, Ganesh T, Rath GK, Joshi RC, et al. A study on contralateral breast surface dose for various tangential field techniques and the impact of set-up error on this dose. Australas Phys Eng Sci Med. 2007; 30:42–45.
Article10. Harsolia A, Kestin L, Grills I, Wallace M, Jolly S, Jones C, et al. Intensity-modulated radiotherapy results in significant decrease in clinical toxicities compared with conventional wedge-based breast radiotherapy. Int J Radiat Oncol Biol Phys. 2007; 68:1375–1380.
Article11. Kestin LL, Sharpe MB, Frazier RC, Vicini FA, Yan D, Matter RC, et al. Intensity modulation to improve dose uniformity with tangential breast radiotherapy: initial clinical experience. Int J Radiat Oncol Biol Phys. 2000; 48:1559–1568.
Article12. Haciislamoglu E, Colak F, Canyilmaz E, Dirican B, Gurdalli S, Yilmaz AH, et al. Dosimetric comparison of left-sided whole-breast irradiation with 3DCRT, forward-planned IMRT, inverse-planned IMRT, helical tomotherapy, and volumetric arc therapy. Radiother Oncol. 2011; 100:241–246.
Article13. Mihai A, Rakovitch E, Sixel K, Woo T, Cardoso M, Bell C, et al. Inverse vs. forward breast IMRT planning. Med Dosim. 2005; 30:149–154.
Article14. Onal C, Sonmez A, Arslan G, Oymak E, Kotek A, Efe E, et al. Dosimetric comparison of the field-in-field technique and tangential wedged beams for breast irradiation. Jpn J Radiol. 2012; 30:218–226.
Article15. Prabhakar R, Julka PK, Rath GK. Can field-in-field technique replace wedge filter in radiotherapy treatment planning: a comparative analysis in various treatment sites. Australas Phys Eng Sci Med. 2008; 31:317–324.
Article16. Michalski A, Atyeo J, Cox J, Rinks M. Inter- and intra-fraction motion during radiation therapy to the whole breast in the supine position: a systematic review. J Med Imaging Radiat Oncol. 2012; 56:499–509.
Article17. Jain P, Marchant T, Green M, Watkins G, Davies J, McCarthy C, et al. Inter-fraction motion and dosimetric consequences during breast intensity-modulated radiotherapy (IMRT). Radiother Oncol. 2009; 90:93–98.
Article18. Song T, Suh CO, Lee I, Jeong K, Keum K, Lee CG, et al. The effect of respiratory motion on forward intensity modulated radiotherapy for breast cancer. Technol Cancer Res Treat. 2008; 7:207–215.
Article19. Mitchell J, Formenti SC, DeWyngaert JK. Interfraction and intrafraction setup variability for prone breast radiation therapy. Int J Radiat Oncol Biol Phys. 2010; 76:1571–1577.
Article20. Kahan Z, Csenki M, Varga Z, Szil E, Cserhati A, Balogh A, et al. The risk of early and late lung sequelae after conformal radiotherapy in breast cancer patients. Int J Radiat Oncol Biol Phys. 2007; 68:673–681.21. Saliou MG, Giraud P, Simon L, Fournier-Bidoz N, Fourquet A, Dendale R, et al. Radiotherapy for breast cancer: respiratory and set-up uncertainties. Cancer Radiother. 2005; 9:414–421.22. Smith RP, Bloch P, Harris EE, McDonough J, Sarkar A, Kassaee A, et al. Analysis of interfraction and intrafraction variation during tangential breast irradiation with an electronic portal imaging device. Int J Radiat Oncol Biol Phys. 2005; 62:373–378.
Article23. Baroni G, Ferrigno G, Orecchia R, Pedotti A. Real-time opto-electronic verification of patient position in breast cancer radiotherapy. Comput Aided Surg. 2000; 5:296–306.
Article24. Richter A, Sweeney R, Baier K, Flentje M, Guckenberger M. Effect of breathing motion in radiotherapy of breast cancer: 4D dose calculation and motion tracking via EPID. Strahlenther Onkol. 2009; 185:425–430.25. Berbeco RI, Pope CJ, Jiang SB. Measurement of the interplay effect in lung IMRT treatment using EDR2 films. J Appl Clin Med Phys. 2006; 7:33–42.
Article26. Court LE, Seco J, Lu XQ, Ebe K, Mayo C, Ionascu D, et al. Use of a realistic breathing lung phantom to evaluate dose delivery errors. Med Phys. 2010; 37:5850–5857.27. Chui CS, Yorke E, Hong L. The effects of intra-fraction organ motion on the delivery of intensity-modulated field with a multileaf collimator. Med Phys. 2003; 30:1736–1746.
Article28. Cao J, Roeske JC, Chmura SJ, Salama JK, Shoushtari AN, Boyer AL, et al. Calculation and prediction of the effect of respiratory motion on whole breast radiation therapy dose distributions. Med Dosim. 2009; 34:126–132.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dosimetric Characteristics of Dynamic Wedge Techinique
- A Smart Setup for Craniospinal Irradiation
- Dosimetric Advantages of the Field-in-field Plan Compared with the Tangential Wedged Beams Plan for Whole-breast Irradiation
- Modified Five Field Technique for Primary and Postop Breast Cancer Irradiation
- A Comprehensive Dosimetric Analysis of Inverse Planned Intensity Modulated Radiation Therapy and Multistatic Fields Technique for Left Breast Radiotherapy