Neurointervention.
2019 Sep;14(2):107-115. 10.5469/neuroint.2019.00108.
Clinical Impact of Intracerebral Hemorrhage after Hyperacute Extracranial Stenting in Patients with Ischemic Stroke
- Affiliations
-
- 1Department of Neurology, Ajou University School of Medicine, Ajou University Medical Center, Suwon, Korea. jinsoo22@gmail.com
- 2Department of Radiology, Ajou University School of Medicine, Ajou University Medical Center, Suwon, Korea.
- 3Department of Neurosurgery, School of Medicine, Kyungpook National University, Daegu, Korea.
- 4Department of Radiology, School of Medicine, Kyungpook National University, Daegu, Korea.
- 5Department of Neurology, School of Medicine, Kyungpook National University, Daegu, Korea.
- 6Department of Neurology, Keimyung University Dongsan Medical Center, Daegu, Korea.
- 7Department of Neurosurgery, Keimyung University Dongsan Medical Center, Daegu, Korea.
- KMID: 2458490
- DOI: http://doi.org/10.5469/neuroint.2019.00108
Abstract
- PURPOSE
Emergent intracranial occlusions causing acute ischemic stroke are often related to extracranial atherosclerotic stenosis. This study aimed to investigate the association between post-procedure intracerebral hemorrhage (ICH) and emergent extracranial artery stenting and assess their effects on clinical outcomes in patients with acute ischemic stroke.
MATERIALS AND METHODS
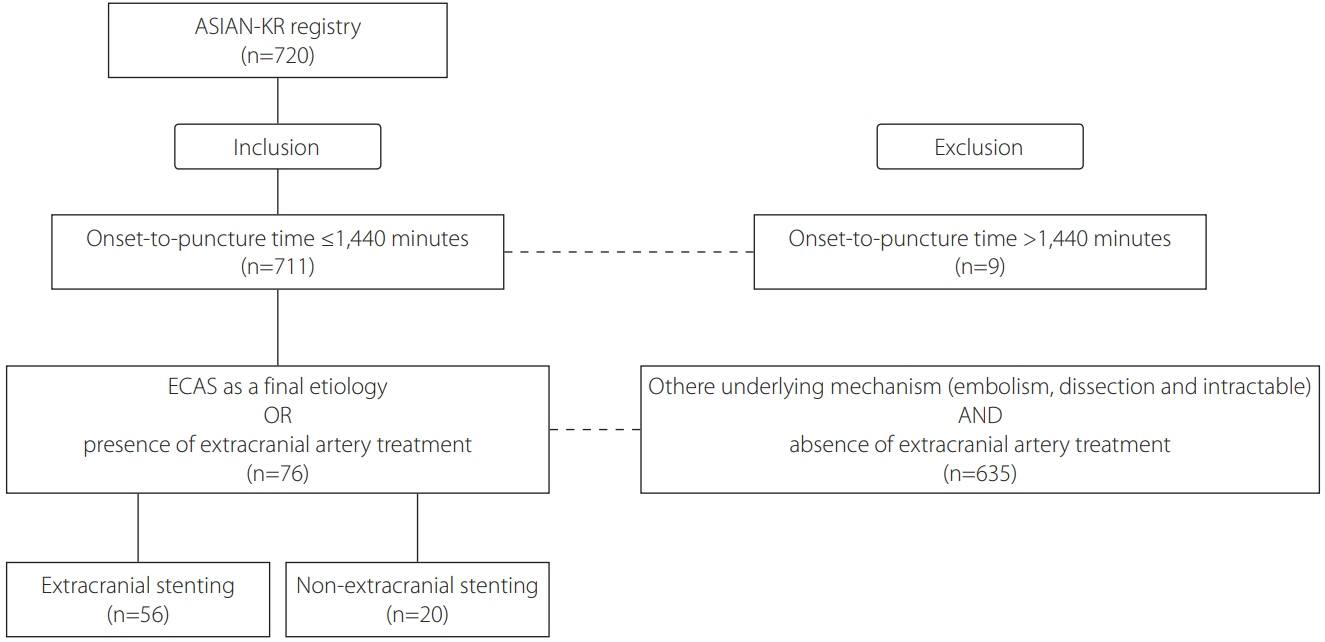
We retrospectively analyzed patients undergoing hyperacute endovascular treatment for cervicocephalic vascular occlusion in three Korean hospitals between January 2011 and February 2016. Patients who had extracranial artery involvement and were treated from 24 hours of symptom onset to puncture were included in this study, and they were divided into the extracranial stenting (ES) and non-ES groups. Any type of petechial hemorrhages and parenchymal hematoma was defined as ICH for the current study.
RESULTS
In total, 76 patients were included in this study. Among them, 56 patients underwent ES, and 20 patients did not. Baseline characteristics, risk factors, laboratory data, treatment methods, successful reperfusion rates, and baseline stenotic degrees of extracranial internal carotid artery did not differ between these two groups. However, atrial fibrillation was more frequent in patients without than with ES (P=0.002), and post-procedure ICH was more frequent in patients with than without ES (P=0.035). Logistic regression models revealed that ES was independently associated with post-procedure ICH (odds ratio [OR], 7.807; 95% confidence interval [CI], 1.213-50.248; P=0.031), and ICH was independently associated with poor clinical outcomes (OR, 0.202; 95% CI, 0.054-0.759; P=0.018); however, ES itself was not associated with clinical outcomes (OR, 0.530; 95% CI, 0.117-2.395; P=0.409). Notably, ICH and ES had interaction for predicting good outcomes (P=0.041).
CONCLUSION
Post-procedure ICH was associated with ES and poor clinical outcomes. Therefore, ES should be cautiously considered in patients with hyperacute stroke.
MeSH Terms
Figure
Cited by 1 articles
-
Factors Contributing to an Efficacious Endovascular Treatment for Acute Ischemic Stroke in Asian Population
Jin Soo Lee, Yang-Ha Hwang, Sung-Il Sohn
Neurointervention. 2021;16(2):91-110. doi: 10.5469/neuroint.2020.00339.
Reference
-
1. Grau AJ, Weimar C, Buggle F, Heinrich A, Goertler M, Neumaier S, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German stroke data bank. Stroke. 2001; 32:2559–2566.
Article2. Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J, et al. Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006; 37:2301–2305.3. Jovin TG, Gupta R, Uchino K, Jungreis CA, Wechsler LR, Hammer MD, et al. Emergent stenting of extracranial internal carotid artery occlusion in acute stroke has a high revascularization rate. Stroke. 2005; 36:2426–2430.
Article4. Papanagiotou P, Roth C, Walter S, Behnke S, Grunwald IQ, Viera J, et al. Carotid artery stenting in acute stroke. J Am Coll Cardiol. 2011; 58:2363–2369.
Article5. Yoon W, Kim BM, Kim DJ, Kim DI, Kim SK. Outcomes and prognostic factors after emergent carotid artery stenting for hyperacute stroke within 6 hours of symptom onset. Neurosurgery. 2015; 76:321–329.
Article6. Grigoryan M, Haussen DC, Hassan AE, Lima A, Grossberg J, Rebello LC, et al. Endovascular treatment of acute ischemic stroke due to tandem occlusions: large multicenter series and systematic review. Cerebrovasc Dis. 2016; 41:306–312.
Article7. Maurer C, Joachimski F, Berlis A. Two in one: endovascular treatment of acute tandem occlusions in the anterior circulation. Clin Neuroradiol. 2015; 25:397–402.
Article8. Cohen JE, Gomori JM, Rajz G, Itshayek E, Eichel R, Leker RR. Extracranial carotid artery stenting followed by intracranial stentbased thrombectomy for acute tandem occlusive disease. J Neurointerv Surg. 2015; 7:412–417.
Article9. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e99.
Article10. Kang DH, Yoon W, Kim SK, Baek BH, Lee YY, Kim YW, et al. Endovascular treatment for emergent large vessel occlusion due to severe intracranial atherosclerotic stenosis. J Neurosurg. 2019; 130:1949–1956.
Article11. Hao Y, Yang D, Wang H, Zi W, Zhang M, Geng Y, et al. Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke. Stroke. 2017; 48:1203–1209.
Article12. Lee JS, Lee SJ, Hong JM, Choi JW, Hong JH, Chang HW, et al. Temporal changes in care processes and outcomes for endovascular treatment of acute ischemic stroke: retrospective registry data from three Korean centers. Neurointervention. 2018; 13:2–12.
Article13. North American Symptomatic Carotid Endarterectomy Trial. Methods, patient characteristics, and progress. Stroke. 1991; 22:711–720.14. Tomsick T, Broderick J, Carrozella J, Khatri P, Hill M, Palesch Y, et al. Revascularization results in the Interventional Management of Stroke II trial. AJNR Am J Neuroradiol. 2008; 29:582–587.
Article15. Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, et al. Hemorrhagic transformation within 36 hours of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke. 1999; 30:2280–2284.16. Frontera JA, Claassen J, Schmidt JM, Wartenberg KE, Temes R, Connolly ES Jr, et al. Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified fisher scale. Neurosurgery. 2006; 59:21–27. ; discussion 21-27.17. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007; 38:967–973.18. Dorado L, Castaño C, Millán M, Aleu A, de la Ossa NP, Gomis M, et al. Hemorrhagic risk of emergent endovascular treatment plus stenting in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2013; 22:1326–1331.
Article19. Zhu F, Bracard S, Anxionnat R, Derelle AL, Tonnelet R, Liao L, et al. Impact of emergent cervical carotid stenting in tandem occlusion strokes treated by thrombectomy: a review of the TITAN collaboration. Front Neurol. 2019; 10:206.
Article20. Zhang L, Dai D, Li Z, Duan G, Zhang YW, Yang P, et al. Risk factors for hyperperfusion-induced intracranial hemorrhage after carotid artery stenting in patients with symptomatic severe carotid stenosis evaluation. J Neurointerv Surg. 2019; 11:474–478.
Article21. Kozar S, Jeromel M. Hyperperfusion and intracranial haemorrhage after carotid angioplasty with stenting–latest review. Signa Vitae. 2014; 9:9–14.22. Narita S, Aikawa H, Nagata S, Tsutsumi M, Nii K, Yoshida H, et al. Intraprocedural prediction of hemorrhagic cerebral hyperperfusion syndrome after carotid artery stenting. J Stroke Cerebrovasc Dis. 2013; 22:615–619.
Article23. Abou-Chebl A, Yadav JS, Reginelli JP, Bajzer C, Bhatt D, Krieger DW. Intracranial hemorrhage and hyperperfusion syndrome following carotid artery stenting: risk factors, prevention, and treatment. J Am Coll Cardiol. 2004; 43:1596–1601.24. Buhk JH, Cepek L, Knauth M. Hyperacute intracerebral hemorrhage complicating carotid stenting should be distinguished from hyperperfusion syndrome. AJNR Am J Neuroradiol. 2006; 27:1508–1513.25. Kim BM. Causes and solutions of endovascular treatment failure. J Stroke. 2017; 19:131–142.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes of Emergent Carotid Artery Stenting within 6 Hours of Symptom Onset in Patients with Acute Ischemic Stroke
- Short-term Coexisting Intracerebral Hemorrhage and Cerebral Infarctions
- Guideline for intra-arterial thrombolysis of hyperacute ischemic stroke patients: Preliminary Report
- Extracranial Carotid Disease: An Interpretation of Extracranial Carotid Artery Disease Guideline 2011
- Emergency Cervical Carotid Artery Stenting After Intravenous Thrombolysis in Patients With Hyperacute Ischemic Stroke