Neurointervention.
2019 Sep;14(2):91-98. 10.5469/neuroint.2019.00150.
Current Status of Clinical Diagnosis and Genetic Analysis of Hereditary Hemorrhagic Telangiectasia in South Korea: Multicenter Case Series and a Systematic Review
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dcsuh@amc.seoul.kr
- 2Department of Laboraory Medicines, Asan Medical Center, University of Ulsan, Seoul, Korea.
- 3Department of Laboraory Medicines, Samsung Medical Center, Seoul, Korea.
- 4Department of Radiology, Severance Stroke Center, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2458488
- DOI: http://doi.org/10.5469/neuroint.2019.00150
Abstract
- PURPOSE
Hereditary hemorrhagic telangiectasia (HHT), a rare genetic vascular disorder, has been rarely reported in South Korea. We investigated the current prevalence and presenting patterns of genetically confirmed HHT in South Korea.
MATERIALS AND METHODS
We defined HHT patients as those with proven mutations on known HHT-related genes (ENG, ACVRL1, SMAD4, and GDF2) or those fulfilling 3 or 4 of the Curaçao criteria. A computerized systematic search was performed in PubMed and KoreaMed using the following search term: ("hereditary hemorrhagic telangiectasia" AND "Korea") OR ("Osler-Weber-Rendu" AND "Korea"). We also collected government health insurance data. HHT genetic testing results were collected from three tertiary hospitals in which the genetic tests were performed. We integrated patient data by analyzing each case to obtain the prevalence and presenting pattern of HHT in South Korea.
RESULTS
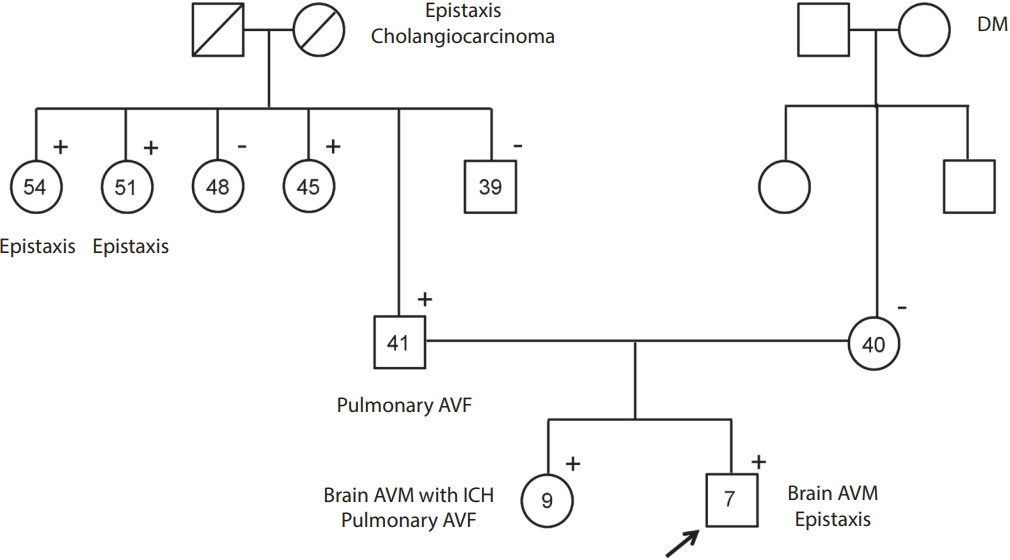
We extracted 90 cases from 52 relevant articles from PubMed and KoreaMed. An additional 22 cases were identified from the three Korean tertiary hospitals after excluding seven cases that overlapped with those in the published articles. Finally, 112 HHT patients were identified (41 males and 71 females, aged 4-82 years [mean±standard deviation, 45.3±20.6 years]). The prevalence of HHT in South Korea is about 1 in 500,000, with an almost equal prevalence among men and women. Forty-nine patients underwent genetic testing, of whom 28 had HHT1 (ENG mutation) and 19 had HHT2 (ACVRL1 mutation); the other two patients were negative for ENG, ACVRL1, and SMAD4 mutations.
CONCLUSION
The prevalence of HHT is underestimated in Korea. The rate of phenotypic presentation seems to be similar to that found worldwide. Korean health insurance coverage is limited to representative genetic analysis to detect ENG and ACVRL1 mutations. Further genetic analyses to detect HHT3, HHT4, and other forms of HHT should be implemented.
Keyword
MeSH Terms
Figure
Reference
-
1. Shovlin CL. Hereditary haemorrhagic telangiectasia: pathophysiology, diagnosis and treatment. Blood Rev. 2010; 24:203–219.
Article2. Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, et al. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet. 2000; 91:66–67.
Article3. McDonald J, Wooderchak-Donahue W, VanSant Webb C, Whitehead K, Stevenson DA, Bayrak-Toydemir P. Hereditary hemorrhagic telangiectasia: genetics and molecular diagnostics in a new era. Front Genet. 2015; 6:1.
Article4. University of Utah. ARUP Scientific Resource for Research and Education: ENG Database. http://arup.utah.edu/database/ENG/ENG_display.php. Accessed January 27, 2019.5. University of Utah. ARUP Scientific Resource for Research and Education: ACVRL1 Database. http://arup.utah.edu/database/ACVRL1/ACVRL1_display.php. Accessed January 27, 2019.6. Health Insurance Review & Assessment Service. Healthcare Bigdata Hub. http://opendata.hira.or.kr/home.do. Accessed January 28, 2019.7. Pau H, Carney AS, Murty GE. Hereditary haemorrhagic telangiectasia (Osler-Weber-Rendu syndrome): otorhinolaryngological manifestations. Clin Otolaryngol Allied Sci. 2001; 26:93–98.
Article8. Jackson SB, Villano NP, Benhammou JN, Lewis M, Pisegna JR, Padua D. Gastrointestinal Manifestations of Hereditary Hemorrhagic Telangiectasia (HHT): a systematic review of the literature. Dig Dis Sci. 2017; 62:2623–2630.
Article9. Kühnel T, Wirsching K, Wohlgemuth W, Chavan A, Evert K, Vielsmeier V. Hereditary hemorrhagic telangiectasia. Otolaryngol Clin North Am. 2018; 51:237–254.
Article10. Plauchu H, de Chadarévian JP, Bideau A, Robert JM. Age-related clinical profile of hereditary hemorrhagic telangiectasia in an epidemiologically recruited population. Am J Med Genet. 1989; 32:291–297.
Article11. Dupuis-Girod S, Cottin V, Shovlin CL. The lung in hereditary hemorrhagic telangiectasia. Respiration. 2017; 94:315–330.
Article12. UpToDate. Clinical manifestations and diagnosis of hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome). https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-hereditary-hemorrhagic-telangiectasia-osler-weber-rendu-syndrome. Accessed January 27, 2019.13. Donaldson JW, McKeever TM, Hall IP, Hubbard RB, Fogarty AW. Complications and mortality in hereditary hemorrhagic telangiectasia: a population-based study. Neurology. 2015; 84:1886–1893.
Article14. Labeyrie PE, Courthéoux P, Babin E, Bergot E, Touzé E, Pelage JP. Neurological involvement in hereditary hemorrhagic telangiectasia. J Neuroradiol. 2016; 43:236–245.
Article15. Krings T, Ozanne A, Chng SM, Alvarez H, Rodesch G, Lasjaunias PL. Neurovascular phenotypes in hereditary haemorrhagic telangiectasia patients according to age. Review of 50 consecutive patients aged 1 day-60 years. Neuroradiology. 2005; 47:711–720.16. Kim H, Nelson J, Krings T, terBrugge KG, McCulloch CE, Lawton MT, et al. Hemorrhage rates from brain arteriovenous malformation in patients with hereditary hemorrhagic telangiectasia. Stroke. 2015; 46:1362–1364.
Article17. Woodall MN, McGettigan M, Figueroa R, Gossage JR, Alleyne CH Jr. Cerebral vascular malformations in hereditary hemorrhagic telangiectasia. J Neurosurg. 2014; 120:87–92.
Article18. Palagallo GJ, McWilliams SR, Sekarski LA, Sharma A, Goyal MS, White AJ. The prevalence of malformations of cortical development in a pediatric hereditary hemorrhagic telangiectasia population. Am J Neuroradiol. 2017; 38:383–386.
Article19. Klostranec JM, Chen L, Mathur S, McDonald J, Faughnan ME, Ratjen F, et al. A theory for polymicrogyria and brain arteriovenous malformations in HHT. Neurology. 2019; 92:34–42.
Article20. Franco CA, Gerhardt H. Morph or move? How distinct endothelial cell responses to blood flow shape vascular networks. Dev Cell. 2017; 41:574–576.
Article21. Sugden WW, Siekmann AF. Endothelial cell biology of Endoglin in hereditary hemorrhagic telangiectasia. Curr Opin Hematol. 2018; 25:237–244.
Article22. David L, Mallet C, Mazerbourg S, Feige JJ, Bailly S. Identification of BMP9 and BMP10 as functional activators of the orphan activin receptor-like kinase 1 (ALK1) in endothelial cells. Blood. 2007; 109:1953–1961.
Article23. Park SO, Wankhede M, Lee YJ, Choi EJ, Fliess N, Choe SW, et al. Real-time imaging of de novo arteriovenous malformation in a mouse model of hereditary hemorrhagic telangiectasia. J Clin Invest. 2009; 119:3487–3496.
Article24. Kroon S, Snijder RJ, Faughnan ME, Mager HJ. Systematic screening in hereditary hemorrhagic telangiectasia: a review. Curr Opin Pulm Med. 2018; 24:260–268.25. McDonald J, Bayrak-Toydemir P, Pyeritz RE. Hereditary hemorrhagic telangiectasia: an overview of diagnosis, management, and pathogenesis. Genet Med. 2011; 13:607–616.
Article26. Faughnan ME, Palda VA, Garcia-Tsao G, Geisthoff UW, McDonald J, Proctor DD, et al. International guidelines for the diagnosis and management of hereditary haemorrhagic telangiectasia. J Med Genet. 2011; 48:73–87.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Genetic Mutation Analysis Can Supplement Clinically Confirmed Hereditary Hemorrhagic Telangiectasia Populations
- Hereditary Hemorrhagic Telangiectasia in a Family
- Hereditary Hemorrhagic Telangiectasia Combined with Pulmonary Arteriovenous Malformation Treated with Transcatheter Embolotherapy
- A Case of Hereditary Hemorrhagic Telangiectasia
- A Case of Hepatic Involvement in Hereditary Hemorrhagic Telangiectasia Presenting as High Output Heart Failure