Korean J Radiol.
2016 Oct;17(5):657-663. 10.3348/kjr.2016.17.5.657.
Superior Cervical Sympathetic Ganglion: Normal Imaging Appearance on 3T-MRI
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea. jeonghlee@amc.seoul.kr
- 2Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea.
- 3Department of Anatomy and Cell Biology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea.
- 4Department of Radiology, Catholic Kwandong University International St. Mary's Hospital, Catholic Kwandong University College of Medicine, Incheon 22711, Korea.
- 5Department of Radiology, Busan Paik Hospital, Inje University College of Medicine, Busan 47392, Korea.
- KMID: 2458057
- DOI: http://doi.org/10.3348/kjr.2016.17.5.657
Abstract
OBJECTIVE
To identify superior cervical sympathetic ganglion (SCSG) and describe their characteristic MR appearance using 3T-MRI.
MATERIALS AND METHODS
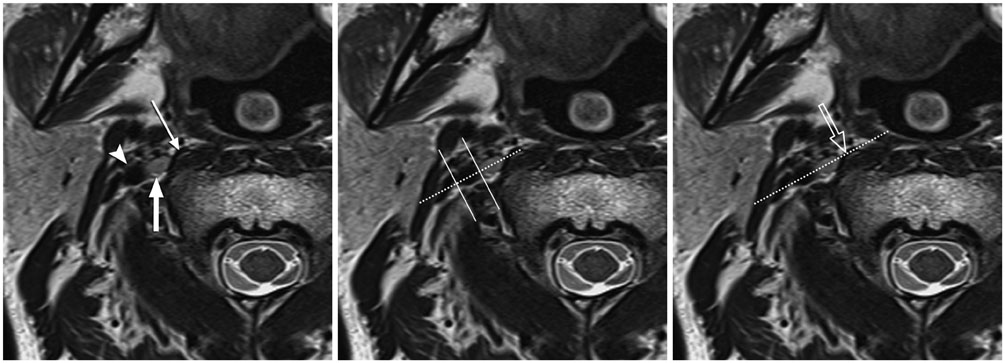
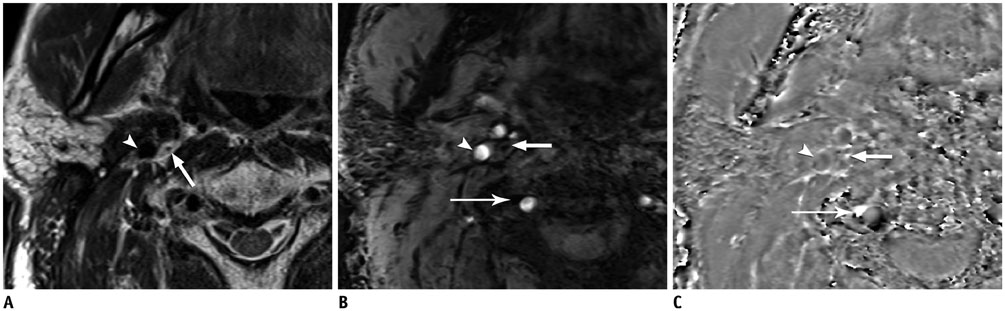
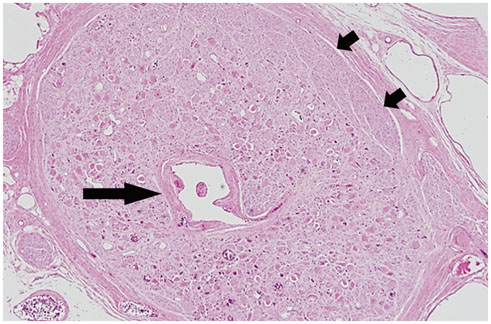
In this prospective study, we recruited 53 consecutive patients without history of head and neck irradiation. Using anatomic location based on literature review, both sides of the neck were evaluated to identify SCSGs in consensus. SCSGs were divided into definite (medial to internal carotid artery [ICA] and lateral to longus capitis muscle [LCM]) and probable SCSGs based on relative location to ICA and LCM. Two readers evaluated signal characteristics including intraganglionic hypointensity of all SCSGs and relative location of probable SCSGs. Interrater and intrarater agreements were quantified using unweighted kappa.
RESULTS
Ninety-one neck sites in 53 patients were evaluated after exclusion of 15 neck sites with pathology. Definite SCSGs were identified at 66 (73%) sites, and probable SCSGs were found in 25 (27%). Probable SCSGs were located anterior to LCM in 16 (18%), lateral to ICA in 6 (7%), and posterior to ICA in 3 (3%). Intraganglionic hypointensity was identified in 82 (90%) on contrast-enhanced fat-suppressed T1-weighted images. There was no statistical difference in the relative location between definite and probable SCSGs of the right and left sides with intragnalionic hypointensity on difference pulse sequences. Interrater and intrarater agreements on the location and intraganglionic hypointensity were excellent (κ-value, 0.749-1.000).
CONCLUSION
3T-MRI identified definite SCSGs at 73% of neck sites and varied location of the remaining SCSGs. Intraganglionic hypointensity was a characteristic feature of SCSGs.
Keyword
Figure
Reference
-
1. Wisco JJ, Stark ME, Safir I, Rahman S. A heat map of superior cervical ganglion location relative to the common carotid artery bifurcation. Anesth Analg. 2012; 114:462–465.2. Elias M. Cervical sympathetic and stellate ganglion blocks. Pain Physician. 2000; 3:294–304.3. Tubbs RS, Salter G, Wellons JC 3rd, Oakes WJ. Blood supply of the human cervical sympathetic chain and ganglia. Eur J Morphol. 2002; 40:283–288.4. Siegenthaler A, Haug M, Eichenberger U, Suter MR, Moriggl B. Block of the superior cervical ganglion, description of a novel ultrasound-guided technique in human cadavers. Pain Med. 2013; 14:646–649.5. Som PM, Curtin HD. Head and neck imaging. 5th ed. St. Louis: Mosby;2011.6. Civelek E, Karasu A, Cansever T, Hepgul K, Kiris T, Sabanci A, et al. Surgical anatomy of the cervical sympathetic trunk during anterolateral approach to cervical spine. Eur Spine J. 2008; 17:991–995.7. Kiray A, Arman C, Naderi S, Güvencer M, Korman E. Surgical anatomy of the cervical sympathetic trunk. Clin Anat. 2005; 18:179–185.8. Saylam CY, Ozgiray E, Orhan M, Cagli S, Zileli M. Neuroanatomy of cervical sympathetic trunk: a cadaveric study. Clin Anat. 2009; 22:324–330.9. Stark ME, Safir I, Wisco JJ. Probabilistic mapping of the cervical sympathetic trunk ganglia. Auton Neurosci. 2014; 181:79–84.10. Lee JH, Lee HK, Lee DH, Choi CG, Kim SJ, Suh DC. Neuroimaging strategies for three types of Horner syndrome with emphasis on anatomic location. AJR Am J Roentgenol. 2007; 188:W74–W81.11. Harris CL, Hamid B, Rosenquist RW, Schultz-Stubner SH. Ganglionic local opioid application (GLOA) for treatment of chronic headache and facial pain. Reg Anesth Pain Med. 2006; 31:460–462.12. Pozzilli P. BCG vaccine in insulin-dependent diabetes mellitus. IMDIAB Group. Lancet. 1997; 349:1520–1521.13. Yuen HW, Goh CH, Tan TY. Enlarged cervical sympathetic ganglion: an unusual parapharyngeal space tumour. Singapore Med J. 2006; 47:321–323.14. Ebraheim NA, Lu J, Yang H, Heck BE, Yeasting RA. Vulnerability of the sympathetic trunk during the anterior approach to the lower cervical spine. Spine (Phila Pa 1976). 2000; 25:1603–1606.15. Wu Z, Mittal S, Kish K, Yu Y, Hu J, Haacke EM. Identification of calcification with MRI using susceptibility-weighted imaging: a case study. J Magn Reson Imaging. 2009; 29:177–182.16. Ding P, Tufano RP, Campbell-Malone R, Feng W, Kim SJ, German RZ. Horner syndrome after carotid sheath surgery in a pig: anatomic study of cervical sympathetic chain. Comp Med. 2011; 61:453–456.17. Wenn CM, Newman DL. Arterial tortuosity. Australas Phys Eng Sci Med. 1990; 13:67–70.18. Sacco S, Totaro R, Baldassarre M, Carolei A. Morphological variations of the internal carotid artery: prevalence, characteristics and association with cerebrovascular disease. Int J Angiol. 2007; 16:59–61.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Enlarged Superior Cervical Sympathetic Ganglion Mimicking a Metastatic Lymph Node in the Retropharyngeal Space: A Case Report
- The Effects of Superior Cervical Ganglion Block on the Behavioral Despair in Rats
- Superior Cervical Sympathetic Ganglion Block may not Influence Early Brain Damage Induced by Permanent Focal Cerebral Ischemia in Rats
- Thoracic Sympathetic Ganglion Block for a Patient with Hyperhidrosis
- Distribution and Origin of Nitrergic Innervation of the Canine Laryngeal Ventricle