J Korean Neurosurg Soc.
2017 Sep;60(5):518-526. 10.3340/jkns.2016.1212.006.
Intra-arterial and Intravenous Tirofiban Infusion for Thromboembolism during Endovascular Coil Embolization of Cerebral Aneurysm
- Affiliations
-
- 1Department of Neuroradiology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea.
- 2Department of Neurosurgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. tgkim@chamc.co.kr
- 3Department of Neurosurgery, Seoul Medical Center, Seoul, Korea.
- KMID: 2457958
- DOI: http://doi.org/10.3340/jkns.2016.1212.006
Abstract
OBJECTIVE
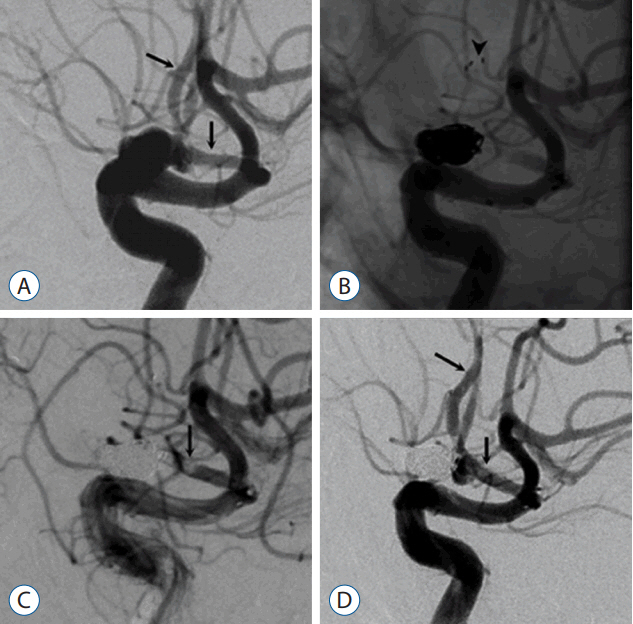
Thromboembolism is the one of the most serious complications that can occur during endovascular coil embolization of cerebral aneurysm. We report on the effectiveness and safety of intra-arterial/intravenous (IA/IV) glycoprotein IIb/IIIa inhibitor (tirofiban) infusion for treating thromboembolism during endovascular coil embolization of cerebral aneurysm.
METHODS
We performed a retrospective analysis of 242 patients with ruptured or unruptured cerebral aneurysms (n=264) who underwent endovascular coil embolization from January 2011 to June 2014. Thromboembolism occurred in 20 patients (7.4%), including 14 cases of ruptured aneurysms and 6 cases of unruptured aneurysms. The most common site of aneurysms was the anterior communicating artery (n=8), followed by middle cerebral artery (n=6). When we found an enlarged thromboembolism during coil embolization, we tried to dissolve it using tirofiban administered via IA and IV loading (5 μg/kg, respectively) for 3-5 minutes followed by IV maintenance (0.08 μg/kg/min) for approximately 4-24 hours.
RESULTS
In 4 of 5 patients with total vessel occlusion, the vessel was recanalized to Thrombolysis in Cerebral Infarction Perfusion Scale (TICI) grade 3, and in 1 patient to TICI grade 2a. In 2 patients with partial vessel occlusion and 13 patients with minimal occlusion, the vessel recanalized to TICI grade 3. Irrelevant intracerebral hemorrhage was noted in 1 patient (5%), and thromboemboli-related cerebral infarction developed in 5 patients (25%), of which only 1 (5%) was symptomatic.
CONCLUSION
IA/IV infusion and IV maintenance with tirofiban appear to be an effective rescue treatment for thromboembolism during endovascular coil embolization in patients with ruptured or unruptured cerebral aneurysms.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Stent-Assisted Coil Embolization Using Only a Glycoprotein IIb/IIIa Inhibitor (Tirofiban) for Ruptured Wide-Necked Aneurysm Repair
Sang Hyub Lee, In Sung Park, Ja Myoung Lee, Kwangho Lee, Hyun Park, Chul Hee Lee
J Cerebrovasc Endovasc Neurosurg. 2018;20(1):14-23. doi: 10.7461/jcen.2018.20.1.14.
Reference
-
References
1. Bizzarri F, Scolletta S, Tucci E, Lucidi M, Davoli G, Toscano T, et al. Perioperative use of tirofiban hydrochloride (Aggrastat) does not increase surgical bleeding after emergency or urgent coronary artery bypass grafting. J Thorac Cardiovasc Surg. 122:1181–1185. 2001.
Article2. Brinjikji W, McDonald JS, Kallmes DF, Cloft HJ. Rescue treatment of thromboembolic complications during endovascular treatment of cerebral aneurysms. Stroke. 44:1343–1347. 2013.
Article3. Brinjikji W, Morales-Valero SF, Murad MH, Cloft HJ, Kallmes DF. Rescue treatment of thromboembolic complications during endovascular treatment of cerebral aneurysms: a meta-analysis. AJNR Am J Neuroradiol. 36:121–125. 2015.
Article4. Bruening R, Mueller-Schunk S, Morhard D, Seelos KC, Brueckmann H, Schmid-Elsaesser R, et al. Intraprocedural thrombus formation during coil placement in ruptured intracranial aneurysms: treatment with systemic application of the glycoprotein IIb/IIIa antagonist tirofiban. AJNR Am J Neuroradiol. 27:1326–1331. 2006.5. Cho YD, Lee JY, Seo JH, Kang HS, Kim JE, Jung KH, et al. Intra-arterial tirofiban infusion for thromboembolic complication during coil embolization of ruptured intracranial aneurysms. Eur J Radiol. 81:2833–2838. 2012.
Article6. Cognard C, Weill A, Castaings L, Rey A, Moret J. Intracranial berry aneurysms: angiographic and clinical results after endovascular treatment. Radiology. 206:499–510. 1998.
Article7. Cronqvist M, Pierot L, Boulin A, Cognard C, Castaings L, Moret J. Local intraarterial fibrinolysis of thromboemboli occurring during endovascular treatment of intracerebral aneurysm: a comparison of anatomic results and clinical outcome. AJNR Am J Neuroradiol. 19:157–165. 1998.8. Debrun GM, Aletich VA, Kehrli P, Misra M, Ausman JI, Charbel F. Selection of cerebral aneurysms for treatment using Guglielmi detachable coils: the preliminary University of Illinois at Chicago experience. Neurosurgery. 43:1281–1295. discussion 1296–1287. 1998.
Article9. Eskridge JM, Song JK. Endovascular embolization of 150 basilar tip aneurysms with Guglielmi detachable coils: results of the Food and Drug Administration multicenter clinical trial. J Neurosurg. 89:81–86. 1998.
Article10. Fiorella D, Albuquerque FC, Han P, McDougall CG. Strategies for the management of intraprocedural thromboembolic complications with abciximab (ReoPro). Neurosurgery. 54:1089–1097. discussion 1097–1098. 2004.
Article11. Fiorella D, Thiabolt L, Albuquerque FC, Deshmukh VR, McDougall CG, Rasmussen PA. Antiplatelet therapy in neuroendovascular therapeutics. Neurosurg Clin N Am. 16:517–540. vi2005.
Article12. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 34:e109–e137. 2003.
Article13. Jeon JS, Sheen SH, Hwang G, Kang SH, Heo DH, Cho YJ. Intraarterial tirofiban thrombolysis for thromboembolisms during coil embolization for ruptured intracranial aneurysms. J Cerebrovasc Endovasc Neurosurg. 14:5–10. 2012.
Article14. Jeong HW, Jin SC. Intra-arterial infusion of a glycoprotein IIb/IIIa antagonist for the treatment of thromboembolism during coil embolization of intracranial aneurysm: a comparison of abciximab and tirofiban. AJNR Am J Neuroradiol. 34:1621–1625. 2013.
Article15. Kang HS, Kwon BJ, Roh HG, Yoon SW, Chang HW, Kim JE, et al. Intra-arterial tirofiban infusion for thromboembolism during endovascular treatment of intracranial aneurysms. Neurosurgery. 63:230–237. discussion 237–238. 2008.
Article16. Koebbe CJ, Horowitz MB, Levy EI, Dutton K, Jungries CC, Purdy PD. Intraarterial thrombolysis for thromboemboli associated with endovascular aneurysm coiling. Report of five cases Interv Neuroradiol. 8:151–158. 2002.
Article17. Marmur JD, Poludasu S, Agarwal A, Manjappa N, Cavusoglu E. High-dose tirofiban administered as bolus-only during percutaneous coronary intervention. J Invasive Cardiol. 20:53–58. 2008.18. Mounayer C, Piotin M, Baldi S, Spelle L, Moret J. Intraarterial administration of abciximab for thromboembolic events occurring during aneurysm coil placement. AJNR Am J Neuroradiol. 24:2039–2043. 2003.19. Park JH, Kim JE, Sheen SH, Jung CK, Kwon BJ, Kwon OK, et al. Intraarterial abciximab for treatment of thromboembolism during coil embolization of intracranial aneurysms: outcome and fatal hemorrhagic complications. J Neurosurg. 108:450–457. 2008.
Article20. Pelz DM, Lownie SP, Fox AJ. Thromboembolic events associated with the treatment of cerebral aneurysms with Guglielmi detachable coils. AJNR Am J Neuroradiol. 19:1541–1547. 1998.21. Ries T, Siemonsen S, Grzyska U, Zeumer H, Fiehler J. Abciximab is a safe rescue therapy in thromboembolic events complicating cerebral aneurysm coil embolization: single center experience in 42 cases and review of the literature. Stroke. 40:1750–1757. 2009.
Article22. Song JK, Niimi Y, Fernandez PM, Brisman JL, Buciuc R, Kupersmith MJ, et al. Thrombus formation during intracranial aneurysm coil placement: treatment with intra-arterial abciximab. AJNR Am J Neuroradiol. 25:1147–1153. 2004.23. Velat GJ, Burry MV, Eskioglu E, Dettorre RR, Firment CS, Mericle RA. The use of abciximab in the treatment of acute cerebral thromboembolic events during neuroendovascular procedures. Surg Neurol. 65:352–358. discussion 358–359. 2006.
Article24. Viñuela F, Duckwiler G, Mawad M. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg. 86:475–482. 1997.
Article25. Workman MJ, Cloft HJ, Tong FC, Dion JE, Jensen ME, Marx WF, et al. Thrombus formation at the neck of cerebral aneurysms during treatment with Guglielmi detachable coils. AJNR Am J Neuroradiol. 23:1568–1576. 2002.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraarterial Tirofiban Thrombolysis for Thromboembolisms During Coil Embolization for Ruptured Intracranial Aneurysms
- Recent Trends in the Treatment of Cerebral Aneurysms: Comparison between Endovascular Coil Embolization and Surgical Clipping
- Surgical Removal of Coil and Clipping of Aneurysm after Failure of Intraaneurysmal Coil Embolization: Case Report
- Intra-arterial Thrombolysis for Central Retinal Artery Occlusion after the Coil Embolization of Paraclinoid Aneurysm
- Delayed Symptomatic Thromboembolism After Unruptured Middle Cerebral Artery Aneurysm Embolization