Ann Rehabil Med.
2019 Aug;43(4):458-464. 10.5535/arm.2019.43.4.458.
Risk Assessment of Injury to Palmar Cutaneous Branch of the Median Nerve Using High-Resolution Ultrasound
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Korea University Guro Hospital, Seoul, Korea. rehab46@korea.ac.kr
- KMID: 2457754
- DOI: http://doi.org/10.5535/arm.2019.43.4.458
Abstract
OBJECTIVE
To evaluate the relationship between the palmar cutaneous branch of median nerve (PCBMN) and surrounding anatomical structures by using high-resolution ultrasound (HRUS) to assess the risk of PCBMN injury.
METHODS
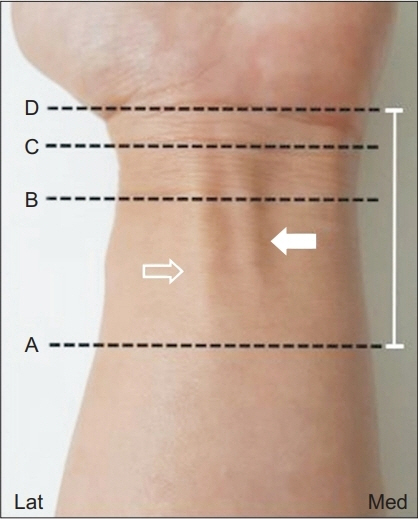
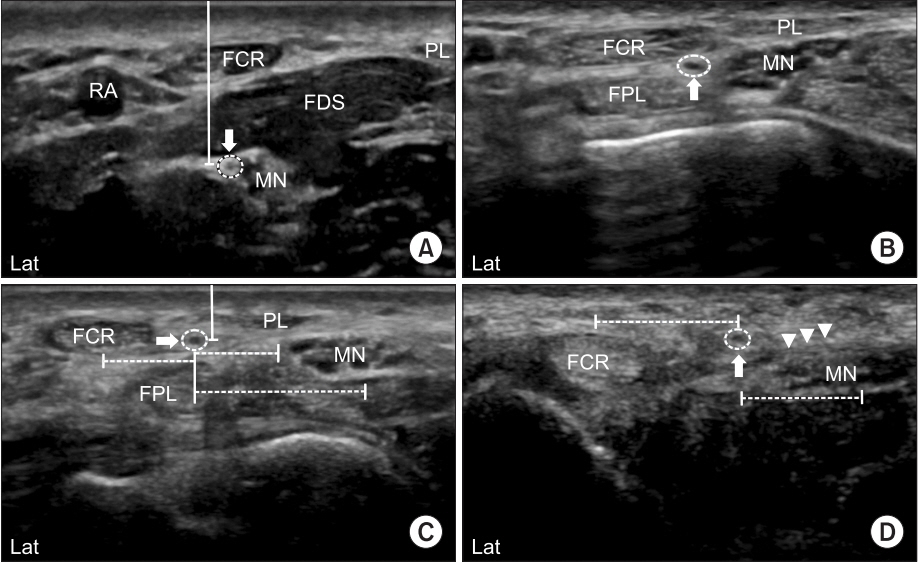
The PCBMN course and the characteristics of bilateral distal forearms and wrists of 30 healthy volunteers were identified. The distance between PCBMN and other anatomical structures at three different levels along its course were measured using HRUS. Moreover, the depth of PCBMN from skin and its cross-sectional area (CSA) were measured.
RESULTS
HRUS showed the PCBMN in all subjects. PCBMN branched off from the radial aspect of the median nerve (MN) at 4.69±0.89 cm proximal to the bistyloid line (BSL) and extended radially toward the flexor carpi radialis (FCR) tendon. PCBMN was within the ulnar edge of FCR tendon sheath, and became more superficial and perforated the antebrachial fascia between the FCR tendon laterally and the palmaris longus (PL) tendon medially. PCBMN was located at 4.08±0.72 mm on the ulnar aspect of the FCR tendon and 4.78±0.36 mm radially on the PL tendon at BSL. At the distal wrist crease level, the PCBMN was located at 5.68±0.58 mm on the ulnar side of the FCR tendon. The PCBMN depth from skin at BSL and its branching point was 1.92±0.41 and 7.95±0.79 mm, respectively. The PCBMN CSA was 0.26±0.15 mm² at BSL.
CONCLUSION
HRUS can be used to identify PCBMN and its relationship with other anatomical structures. Our data can be used to predict PCBMN location, and prevent complications associated with invasive procedures involving the wrist.
MeSH Terms
Figure
Cited by 1 articles
-
Is Palmar Cutaneous Branch of the Median Nerve More Swollen in Carpal Tunnel Syndrome?
Ha Mok Jeong, Young Ha Jeong, Joon Shik Yoon
Ann Rehabil Med. 2021;45(4):325-330. doi: 10.5535/arm.21101.
Reference
-
1. Bezerra AJ, Carvalho VC, Nucci A. An anatomical study of the palmar cutaneous branch of the median nerve. Surg Radiol Anat. 1986; 8:183–8.
Article2. Chaynes P, Becue J, Vaysse P, Laude M. Relationships of the palmar cutaneous branch of the median nerve: a morphometric study. Surg Radiol Anat. 2004; 26:275–80.
Article3. Rotman MB, Donovan JP. Practical anatomy of the carpal tunnel. Hand Clin. 2002; 18:219–30.
Article4. Kuhlmann N, Tubiana R, Lisfranc R. Contribution of anatomy to the understanding of carpal tunnel compression syndromes and sequelae of decompression operations. Rev Chir Orthop Reparatrice Appar Mot. 1978; 64:59–70.5. Kamath J, Jayasheelan N, Mathews R. Compressive neuropathy of the palmar cutaneous branch of the median nerve after a malunited fracture of the distal radius. J Hand Surg Eur Vol. 2016; 41:231–2.
Article6. Carroll RE, Green DP. The significance of the palmar cutaneous nerve at the wrist. Clin Orthop Relat Res. 1972; 83:24–8.
Article7. Louis DS, Greene TL, Noellert RC. Complications of carpal tunnel surgery. J Neurosurg. 1985; 62:352–6.
Article8. Ilyas AM. Surgical approaches to the distal radius. Hand (N Y). 2011; 6:8–17.
Article9. An H, Park S, Kim HD. The influence of stimulation site on the conduction study of palmar cutaneous branch of median nerve. J Korean Acad Rehabil Med. 2002; 26:46–9.10. Imai T, Wada T, Matsumoto H. Entrapment neuropathy of the palmar cutaneous branch of the median nerve in carpal tunnel syndrome. Clin Neurophysiol. 2004; 115:2514–7.
Article11. Tagliafico A, Pugliese F, Bianchi S, Bodner G, Padua L, Rubino M, et al. High-resolution sonography of the palmar cutaneous branch of the median nerve. AJR Am J Roentgenol. 2008; 191:107–14.
Article12. Chang KV, Mezian K, Nanka O, Wu WT, Lou YM, Wang JC, et al. Ultrasound imaging for the cutaneous nerves of the extremities and relevant entrapment syndromes: from anatomy to clinical implications. J Clin Med. 2018; 7:E457.
Article13. McCann PA, Clarke D, Amirfeyz R, Bhatia R. The cadaveric anatomy of the distal radius: implications for the use of volar plates. Ann R Coll Surg Engl. 2012; 94:116–20.
Article14. Conti Mica MA, Bindra R, Moran SL. Anatomic considerations when performing the modified Henry approach for exposure of distal radius fractures. J Orthop. 2016; 14:104–7.
Article15. Hobbs RA, Magnussen PA, Tonkin MA. Palmar cutaneous branch of the median nerve. J Hand Surg Am. 1990; 15:38–43.
Article16. Gaspar MP, Sessions BA, Dudoussat BS, Kane PM. Single-incision carpal tunnel release and distal radius open reduction and internal fixation: a cadaveric study. J Wrist Surg. 2016; 5:241–6.17. Jones C, Beredjiklian P, Matzon JL, Kim N, Lutsky K. Incidence of an anomalous course of the palmar cutaneous branch of the median nerve during volar plate fixation of distal radius fractures. J Hand Surg Am. 2016; 41:841–4.
Article18. Berglund LM, Messer TM. Complications of volar plate fixation for managing distal radius fractures. J Am Acad Orthop Surg. 2009; 17:369–77.
Article19. Smith J, Wisniewski SJ, Finnoff JT, Payne JM. Sonographically guided carpal tunnel injections: the ulnar approach. J Ultrasound Med. 2008; 27:1485–90.20. Kim DH, Jang JE, Park BK. Anatomical basis of ulnar approach in carpal tunnel injection. Pain Physician. 2013; 16:E191–8.21. Cartwright MS, Walker FO. Neuromuscular ultrasound in common entrapment neuropathies. Muscle Nerve. 2013; 48:696–704.
Article22. Roche SJ, Ng CY. Absent palmar cutaneous branch of median nerve. J Hand Microsurg. 2014; 6:47–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Electrophysiological and Ultrasonographic Evaluation of Palmar Digital Nerve Injury in Distal Finger
- Is Palmar Cutaneous Branch of the Median Nerve More Swollen in Carpal Tunnel Syndrome?
- The Influence of Stimulation Site on the Conduction Study of Palmar Cutaneous Branch of Median Nerve
- Anatomical variations of the innervated radial artery superficial palmar branch flap: A series of 28 clinical cases
- Variation of the palmar cutaneous branch of the median nerve identified within the tendon sheath of the flexor carpal radialis