Healthc Inform Res.
2019 Jul;25(3):230-235. 10.4258/hir.2019.25.3.230.
Internet of Things Applied in Healthcare Based on Open Hardware with Low-Energy Consumption
- Affiliations
-
- 1TIGUM Research Group, Universidad Militar Nueva Granada, Bogota, Colombia. leonardo.ramirez@unimilitar.edu.co
- 2GINT Research Group, Universidad de Santiago de Chile, Santiago, Chile.
- KMID: 2457475
- DOI: http://doi.org/10.4258/hir.2019.25.3.230
Abstract
OBJECTIVES
The Internet of Things (IoT) and its applications are growing simultaneously. These applications need new intelligent devices along heterogeneous networking. Which makes them costly to implement indeed. Platforms and open devices designed for open-source hardware are possible solutions. This research was conducted under an IoT design, implementation, and assessment model for the remote monitoring of pulse oximetry via oxygen partial saturation (SpO2) and heart rate (HR) with low-energy consumption.
METHODS
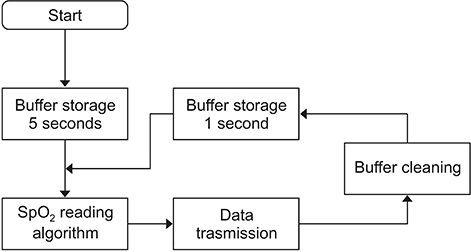
This study focused on the development of SpO2 and HR measurements that will allow the monitoring and estimation in real time of the user's state and health related to the established parameters. Measurements were acquired and recorded using a remote web server that recorded the acquired variables for further processing. The statistical analysis data allows comparison of the registered data measured with theoretical models.
RESULTS
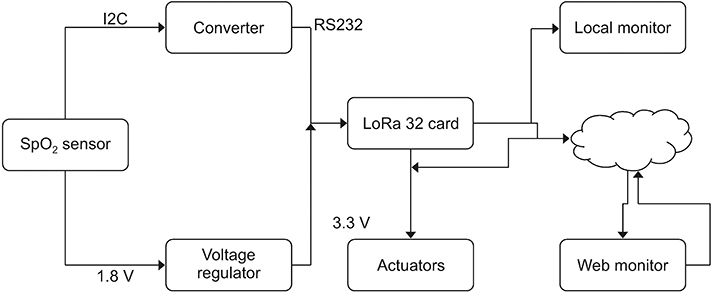
The IoT model was developed use Bluetooth low-energy devices, which comply with low-cost and open-hardware solutions operated via "˜HTTP requests' for data transmission and reception from a cloud server to an edge device. Network performance assessment was conducted to guarantee the availability and integrity of the acquired values and signals. The system measured SpO2 and HR variables. The most significant result was to achieve energy consumption 20% lower than that of devices in the market.
CONCLUSIONS
In summary, the acquired data validation based on the IoT model had a transmission error of 0.001% which proves its applicability in healthcare.
MeSH Terms
Figure
Cited by 1 articles
-
Real-Time Monitoring System to Manage Mental Healthcare Emergency Unit
Samy Housbane, Adil Khoubila, Khaoula Ajbal, Mohamed Agoub, Omar Battas, Mohamed Bennani Othmani
Healthc Inform Res. 2020;26(4):344-350. doi: 10.4258/hir.2020.26.4.344.
Reference
-
1. Son LP, Thu NT, Kien NT. Design an IoT wrist-device for SpO2 measurement. In : Proceedings of 2017 International Conference on Advanced Technologies for Communications (ATC); 2017 Oct 18–20; Quy Nhon, Vietnam. p. 144–149.2. Lee I, Lee K. The Internet of Things (IoT): applications, investments, and challenges for enterprises. Bus Horiz. 2015; 58(4):431–440.
Article3. Vogler M. Efficient IoT application delivery and management in smart city environments [dissertation]. Wien, Austria: Technische Universitat Wien;2016.4. Valdivieso Caraguay AL, Benito Peral A, Barona Lopez LI, Garcia Villalba LJ. SDN: evolution and opportunities in the development IoT applications. Int J Distrib Sens Netw. 2014; 10(5):735142.
Article5. Ma HD. Internet of Things: objectives and scientific challenges. J Comp Sci Technol. 2011; 26(6):919–924.
Article6. Atzori L, Iera A, Morabito G. Understanding the Internet of Things: definition, potentials, and societal role of a fast evolving paradigm. Ad Hoc Netw. 2017; 56:122–140.
Article7. Chiang M, Zhang T. Fog and IoT: an overview of research opportunities. IEEE Internet Things J. 2016; 3(6):854–864.
Article8. Kelly SD, Suryadevara NK, Mukhopadhyay SC. Towards the implementation of IoT for environmental condition monitoring in homes. IEEE Sens J. 2013; 13(10):3846–3853.
Article9. Al-Fuqaha A, Guizani M, Mohammadi M, Aledhari M, Ayyash M. Internet of Things: a survey on enabling technologies, protocols, and applications. IEEE Commun Surv Tutor. 2015; 17(4):2347–2376.
Article10. Wang J, Li D. Adaptive computing optimization in software-defined network-based industrial Internet of Things with fog computing. Sensors (Basel). 2018; 18(8):2509.
Article11. Ibarra-Lancheros KS, Puerto-Leguizamon G, Suarez-Fajardo C. Quality of service evaluation based on network slicing for software-defined 5G systems. TecnoLogicas. 2018; 21(43):27–41.
Article12. Sundararaman LV, Edwards RR, Ross EL, Jamison RN. Integration of mobile health technology in the treatment of chronic pain: a critical review. Reg Anesth Pain Med. 2017; 42(4):488–498.
Article13. Severinghaus JW. Takuo Aoyagi: discovery of pulse oximetry. Anesth Analg. 2007; 105:6 Suppl. S1–S4.
Article14. Aarrestad S, Qvarfort M, Kleiven AL, Tollefsen E, Skjonsberg OH, Janssens JP. Diagnostic accuracy of simple tools in monitoring patients with chronic hypoventilation treated with non-invasive ventilation; a prospective cross-sectional study. Respir Med. 2018; 144:30–35.
Article15. Song S, Jiang F, Hao L, Xu L, Yi X, Li G, et al. Use of bi-level pulsed frequency-division excitation for improving blood oxygen saturation precision. Measurement. 2018; 129:523–529.
Article16. O'Leary RJ Jr, Landon M, Benumof JL. Buccal pulse oximeter is more accurate than finger pulse oximeter in measuring oxygen saturation. Anesth Analg. 1992; 75(4):495–498.17. Arruza J, Alzate R. Esfuerzo percibido y frecuencia cardiaca: El control de la intensidad de los esfuerzos en el entrenamiento de judo. Revista de Psicologia del Deporte. 2007; 5(2):29–40.18. Mendonca F, Mostafa SS, Morgado-Dias F, Navarro-Mesa JL, Julia-Serda G, Ravelo-Garcia AG. A portable wireless device based on oximetry for sleep apnea detection. Computing. 2018; 100(11):1203–1219.
Article19. Laborde M. Medida de la Saturacion de Oxigeno por Medio Optico [Internet]. Montevideo, Uruguay: Universidad de la Republica;2004. cited at 2019 Jun 30. Available from: http://www.nib.fmed.edu.uy/laborde.pdf.20. Muncharaz AB, Andres EB, Valero RR, Font SM, Tuson RC, Campos RA. Relationship between pulse oximetry and determination of arterial oxygen saturation. Influence of vasoactive drugs on the SattcO2-SatO2 correlation. Med Intensiva. 2001; 25(9):333–339.21. Chan C, Inskip JA, Kirkham AR, Ansermino JM, Dumont G, Li LC, et al. A smartphone oximeter with a fingertip probe for use during exercise training: usability, validity and reliability in individuals with chronic lung disease and healthy controls. Physiotherapy. 2018; 10. 26. [Epub]. DOI: 10.1016/j.physio.2018.07.015.
Article22. Gong G, Guo Y, Sun X, Wang X, Yin Y, Feng DD. Study of an oxygen supply and oxygen saturation monitoring system for radiation therapy associated with the active breathing coordinator. Sci Rep. 2018; 8(1):1254.
Article23. Jones GA, Ray S, Ramnarayan P, Peters MJ. Error without trials: Safe SpO(2) threshold levels may not be derivable from SpO(2)-PaO(2) relationships. J Crit Care. 2017; 40:283–284.
Article24. Al Rajeh AM, Hurst JR. Monitoring of physiological parameters to predict exacerbations of chronic obstructive pulmonary disease (COPD): a systematic review. J Clin Med. 2016; 5(12):108.
Article25. Kim JA. Book Review: The Internet of Healthy Things. Healthc Inform Res. 2016; 22(3):250.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Internet of Things: An Overview and its Applications in Aviation
- Book Review: The Internet of Healthy Things
- Usage of the Internet of Things in Medical Institutions and its Implications
- Wearable Devices in Medical Internet of Things: Scientific Research and Commercially Available Devices
- Action Research on Development and Application of Internet of Things Services in Hospital