Neonatal Med.
2019 Aug;26(3):138-146. 10.5385/nm.2019.26.3.138.
Evaluation of Newborn Infants with Prenatally Diagnosed Congenital Pulmonary Airway Malformation: A Single-Center Experience
- Affiliations
-
- 1Division of Neonatology, Department of Pediatrics, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Division of Neonatology, Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. kipark@yuhs.ac
- KMID: 2457181
- DOI: http://doi.org/10.5385/nm.2019.26.3.138
Abstract
- PURPOSE
Congenital pulmonary airway malformation (CPAM)"”a rare developmental anomaly"”affects the lower respiratory tract in newborns. By comparing the reliability of diagnostic tools and identifying predictive factors for symptoms, we provide comprehensive clinical data for the proper management of CPAM.
METHODS
We reviewed the medical records of 66 patients with prenatally diagnosed CPAM delivered at Severance Children's Hospital between January 2005 and July 2017.
RESULTS
We enrolled 33 boys and 33 girls. Their mean gestational age and birth weight were 38.8 weeks and 3,050 g, respectively. Prenatal ultrasonography and postnatal radiography, lung ultrasonography, and chest computed tomography (CT) showed inconsistent findings. Chest CT showed superior sensitivity (100%) and positive predictive value (90%). Among the 66 patients, 59 had postnatally confirmed CPAM, three had pulmonary sequestration, one had cystic teratoma, and one had a normal lung. Of the 59 patients with CPAM, 21 (35%; mean age, 23.4 months) underwent surgery, including 15 who underwent video-assisted thoracoscopy. Twenty-five and 12 patients exhibited respiratory symptoms at birth and during infancy, respectively. Apgar scores and mediastinal shift on radiography were significantly associated with respiratory symptoms at birth. However, none of the factors could predict respiratory symptoms during infancy.
CONCLUSION
Radiography or ultrasonography combined with chest CT can confirm an unclear or inconsistent lesion. Apgar scores and mediastinal shift on radiography can predict respiratory symptoms at birth. However, symptoms during infancy are not associated with prenatal and postnatal factors. Chest CT combined with periodic symptom monitoring is important for diagnosing and managing patients with prenatally diagnosed CPAM and to guide appropriate timing of surgery.
Keyword
MeSH Terms
-
Birth Weight
Bronchopulmonary Sequestration
Cystic Adenomatoid Malformation of Lung, Congenital
Female
Gestational Age
Humans
Infant, Newborn*
Lung
Medical Records
Parturition
Radiography
Respiratory System
Teratoma
Thoracic Surgery, Video-Assisted
Thoracoscopy
Thorax
Tomography, X-Ray Computed
Ultrasonography
Ultrasonography, Prenatal
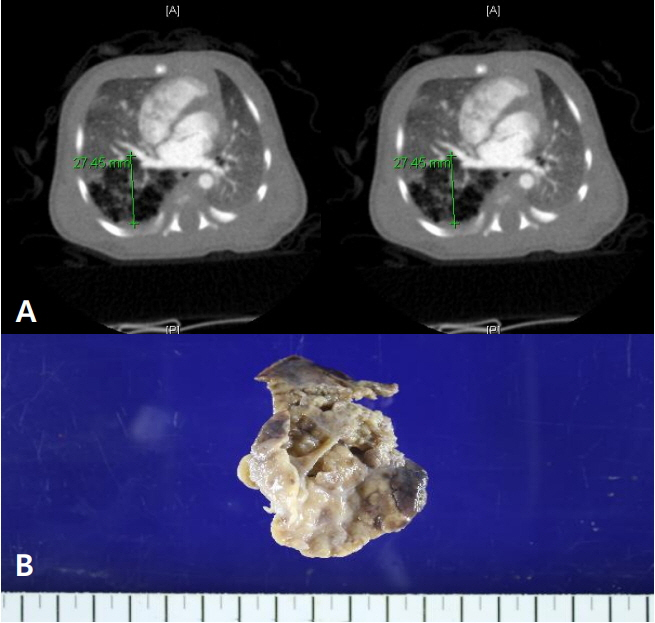
Figure
Reference
-
1. Kulwa E, Tharakan T, Baxi L. Congenital cystic adenomatoid malformation in the fetus: a hypothesis of its development. Fetal Diagn Ther. 2005; 20:472–4.2. Laje P, Liechty KW. Postnatal management and outcome of prenatally diagnosed lung lesions. Prenat Diagn. 2008; 28:612–8.3. Suh YE, Kim HK, Choi YS, Lee BS, Kim KS, Won HS, et al. Neonatal characteristic of congenital cystic adenomatoid malformation of the lung requiring early operation and preoperative intervention. Neonatal Med. 2013; 20:81–9.4. Stanton M. The argument for a non-operative approach to asymptomatic lung lesions. Semin Pediatr Surg. 2015; 24:183–6.5. Stocker JT, Madewell JE, Drake RM. Congenital cystic adenomatoid malformation of the lung. Classification and morphologic spectrum. Hum Pathol. 1977; 8:155–71.6. Xia B, Yu G, Liu C, Hong C, Tang J. Surgical treatment of congenital cystic adenomatoid malformation: a retrospective study of single tertiary center experience. J Matern Fetal Neonatal Med. 2017; 30:416–9.7. Leblanc C, Baron M, Desselas E, Phan MH, Rybak A, Thouvenin G, et al. Congenital pulmonary airway malformations: stateof-the-art review for pediatrician's use. Eur J Pediatr. 2017; 176:1559–71.8. Turan O, Hirfanoglu IM, Beken S, Biri A, Efeturk T, Atalay Y. Prenatally detected congenital cystic adenomatoid malformation and postnatally diagnosed trisomy 13: case report and review of the literature. Turk J Pediatr. 2011; 53:337–41.9. Kitaichi M, Yousem S. Symposium 24: non-neoplastic lung disease. Histopathology. 2002; 41(Suppl 2):424–58.10. Thakkar HS, Durell J, Chakraborty S, Tingle BL, Choi A, Fowler DJ, et al. Antenatally detected congenital pulmonary airway malformations: the Oxford experience. Eur J Pediatr Surg. 2017; 27:324–9.11. Shanmugam G, MacArthur K, Pollock JC. Congenital lung malformations: antenatal and postnatal evaluation and management. Eur J Cardiothorac Surg. 2005; 27:45–52.12. Hardee S, Tuzovic L, Silva CT, Cowles RA, Copel J, Morotti RA. Congenital cystic lung lesions: evolution from in-utero detection to pathology diagnosis. A multidisciplinary approach. Pediatr Dev Pathol. 2017; 20:403–10.13. Pacharn P, Kline-Fath B, Calvo-Garcia M, Linam LE, Rubio EI, Salisbury S, et al. Congenital lung lesions: prenatal MRI and postnatal findings. Pediatr Radiol. 2013; 43:1136–43.14. Ruchonnet-Metrailler I, Leroy-Terquem E, Stirnemann J, Cros P, Ducoin H, Hadchouel A, et al. Neonatal outcomes of prenatally diagnosed congenital pulmonary malformations. Pediatrics. 2014; 133:e1285. –91.15. Gallardo AM, Alvarez de la Rosa RM, De Luis EJF, Mendoza RL, Padilla PAI, Troyano LJ. Antenatal ultrasound diagnosis and neonatal results of the congenital cystic adenomatoid malformation of the lung. Rev Chil Pediatr. 2018; 89:224–230.16. Shamas AG, Bohara K. Congenital cystic adenomatoid malformation of the lung (CCAM), a retrospective clinical audit and literature review in a tertiary centre in Scotland over a period of 14 years. J Obstet Gynaecol. 2017; 37:19–24.17. Crombleholme TM, Coleman B, Hedrick H, Liechty K, Howell L, Flake AW, et al. Cystic adenomatoid malformation volume ratio predicts outcome in prenatally diagnosed cystic adenomatoid malformation of the lung. J Pediatr Surg. 2002; 37:331–8.18. Shirota C, Tainaka T, Nakane T, Tanaka Y, Hinoki A, Sumida W, et al. Usefulness of fetal magnetic resonance imaging for postnatal management of congenital lung cysts: prediction of probability for emergency surgery. BMC Pediatr. 2018; 18:105.19. Kantor N, Wayne C, Nasr A. Symptom development in originally asymptomatic CPAM diagnosed prenatally: a systematic review. Pediatr Surg Int. 2018; 34:613–20.20. Morini F, Zani A, Conforti A, van Heurn E, Eaton S, Puri P, et al. Erratum to: current management of congenital pulmonary airway malformations: a "European Pediatric Surgeons' Association" Survey. Eur J Pediatr Surg. 2018; 28:e1.21. Derderian SC, Coleman AM, Jeanty C, Lim FY, Shaaban AM, Farrell JA, et al. Favorable outcomes in high-risk congenital pulmonary airway malformations treated with multiple courses of maternal betamethasone. J Pediatr Surg. 2015; 50:515–8.22. Kapralik J, Wayne C, Chan E, Nasr A. Surgical versus conservative management of congenital pulmonary airway malformation in children: a systematic review and meta-analysis. J Pediatr Surg. 2016; 51:508–12.23. Polites SF, Habermann EB, Zarroug AE, Thomsen KM, Potter DD. Thoracoscopic vs open resection of congenital cystic lung disease: utilization and outcomes in 1120 children in the United States. J Pediatr Surg. 2016; 51:1101–5.24. Rothenberg SS, Middlesworth W, Kadennhe-Chiweshe A, Aspelund G, Kuenzler K, Cowles R, et al. Two decades of experience with thoracoscopic lobectomy in infants and children: standardizing techniques for advanced thoracoscopic surgery. J Laparoendosc Adv Surg Tech A. 2015; 25:423–8.25. Ghosh M, Islam N, Ghosh A, Chaudhuri PM, Saha K, Chatterjee U. Pleuropulmonary blastoma developing in a case of misinterpreted congenital pulmonary airway malformation: a case report. Fetal Pediatr Pathol. 2018; 37:377–86.26. Delacourt C, Hadchouel A, Khen Dunlop N. Shall all congenital cystic lung malformations be removed? the case in favour. Paediatr Respir Rev. 2013; 14:169–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of prenatally diagnosed extrapulmonary arteriovenous malformation associated with a complex heart defect
- An Intraabdominal Pulmonary Sequestration Containing Congenital Cystic Adenomatoid Malformation
- Case of mucinous adenocarcinoma of the lung associated with congenital pulmonary airway malformation in a neonate
- Congenital Pulmonary Lymphangiectasis
- Prenatally Diagnosed Extrapulmonary Sequestration: 2cases