J Korean Ophthalmol Soc.
2019 Aug;60(8):808-815. 10.3341/jkos.2019.60.8.808.
Choroidal Neovascularization in a Patient with Best Disease
- Affiliations
-
- 1Department of Ophthalmology, Kyungpook National University School of Medicin, Daegu, Korea. Jps11@hanmail.net
- KMID: 2455466
- DOI: http://doi.org/10.3341/jkos.2019.60.8.808
Abstract
- PURPOSE
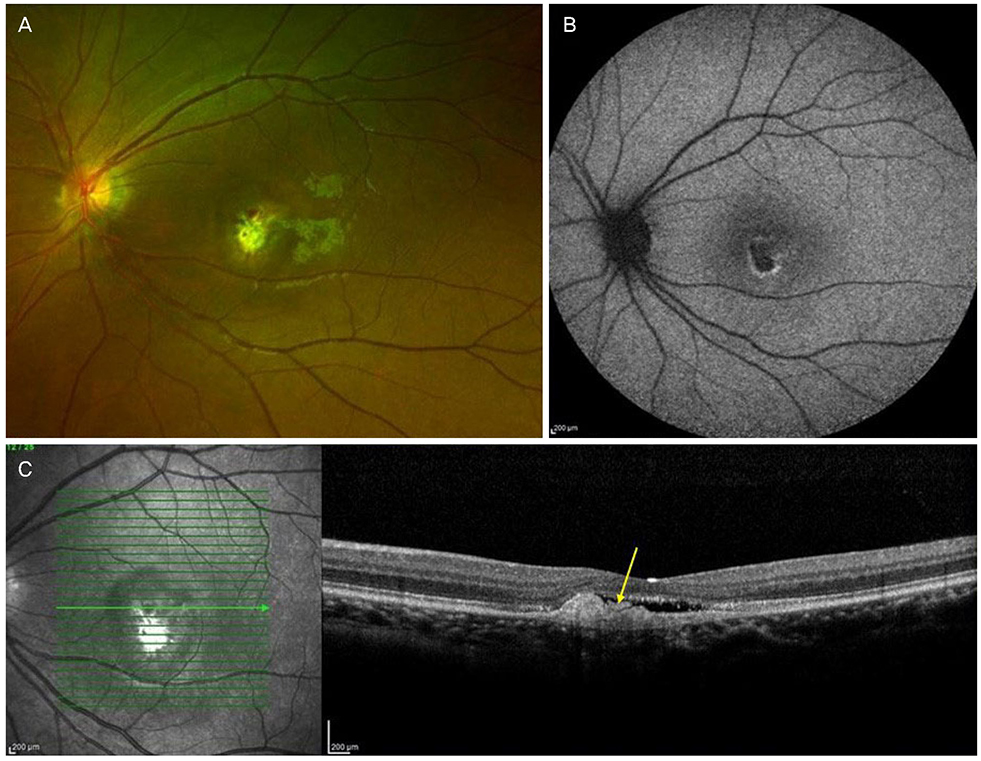
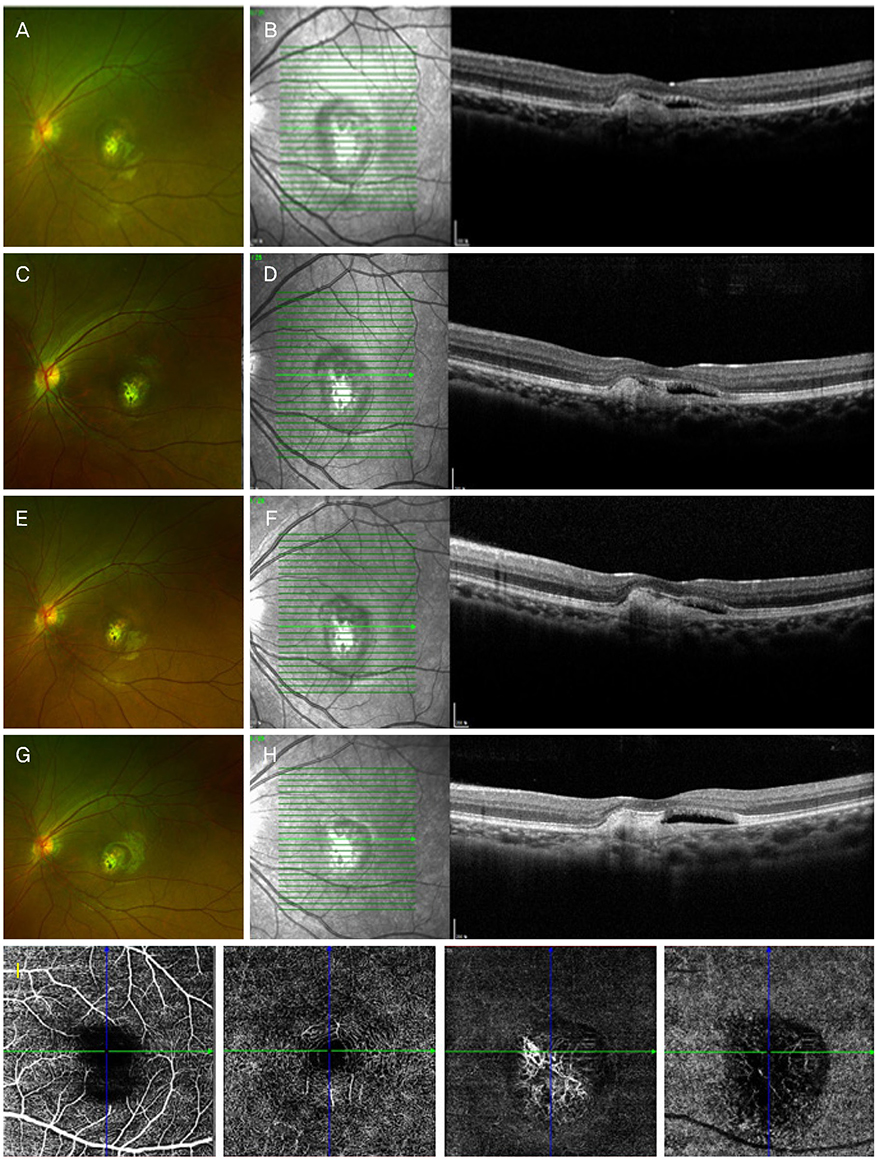
To report a case of choroidal neovascularization in a Best disease patient treated with intravitreal bevacizumab injection and followed up with optical coherence tomography angiography (OCTA).
CASE SUMMARY
A 20-year-old female visited our clinic with decreased visual acuity of the left eye for 6 months. On optical coherence tomography (OCT), subretinal fluid and hyperreflective subretinal clumps were observed in the macula of the right eye. Subretinal hemorrhage and subretinal fluid were observed in the left eye. Choroidal neovascularization in the left eye was observed using OCTA, fluorescein angiography, and indocyanine green angiography. A full-field electroretinogram was normal in both eyes, but an electrooculogram revealed that the Arden ratio was 1.564 in the right eye and 1.081 in the left eye. Intravitreal bevacizumab injection was performed in the left eye. At 6 months after the intravitreal injection, the best-corrected visual acuity of the left eye had recovered to 20/20. OCT revealed that subretinal fluid reduced and choroidal neovascularization was stable. After 12 months, visual acuity of the left eye was maintained at 20/20, but OCTA revealed that choroidal neovascularization had increased.
CONCLUSIONS
Choroidal neovascularization associated with Best disease can improve by intravitreal bevacizumab injection, and the changes in choroidal neovascularization can be followed using OCTA.
Keyword
MeSH Terms
Figure
Reference
-
1. Marmorstein AD, Marmorstein LY, Rayborn M, et al. Bestrophin, the product of the Best vitelliform macular dystrophy gene (VMD2), localizes to the basolateral plasma membrane of the retinal pigment epithelium. Proc Natl Acad Sci U S A. 2000; 97:12758–12763.
Article2. Deutman AF, Hoyng CB, van Lith-Verhoeven JJC. Macular dystrophies. In : Ryan SJ, Schachat AP, Wilkinson C, editors. Retina. 4th ed. Baltimore: Elsevier Mosby;2006. v. 2:chap. 63.3. Shahzad R, Siddiqui MA. Choroidal neovascularization secondary to Best vitelliform macular dystrophy detected by optical coherence tomography angiography. J AAPOS. 2017; 21:68–70.
Article4. Patel RC, Gao SS, Zhang M, et al. Optical coherence tomography angiography of choroidal neovascularization in four inherited retinal dystrophies. Retina. 2016; 36:2339–2347.
Article5. Stattin M, Ahmed D, Glittenberg C, et al. Optical coherence tomography angiography for the detection of secondary choroidal neovascularization in vitelliform macular dystrophy. Retin Cases Brief Rep. 2017; 08. 16. DOI: 10.1097/ICB.0000000000000626.
Article6. Guduru A, Gupta A, Tyagi M, et al. Optical coherence tomography angiography characterisation of Best disease and associated choroidal neovascularisation. Br J Ophthalmol. 2018; 102:444–447.
Article7. Wang XN, You QS, Li Q, et al. Findings of optical coherence tomography angiography in Best vitelliform macular dystrophy. Ophthalmic Res. 2018; 60:214–220.
Article8. Andrade RE, Farah ME, Cardillo JA, et al. Optical coherence tomography in choroidal neovascular membrane associated with Best's vitelliform dystrophy. Acta Ophthalmol Scand. 2002; 80:216–218.
Article9. Sodi A, Murro V, Caporossi O, et al. Long-term results of photodynamic therapy for choroidal neovascularization in pediatric patients with Best vitelliform macular dystrophy. Ophthalmic Genet. 2015; 36:168–174.
Article10. Leu J, Schrage NF, Degenring RF. Choroidal neovascularisation secondary to Best's disease in a 13-year-old boy treated by intravitreal bevacizumab. Graefes Arch Clin Exp Ophthalmol. 2007; 245:1723–1725.
Article11. Heidary F, Hitam WH, Ngah NF, et al. Intravitreal ranibizumab for choroidal neovascularization in Best's vitelliform macular dystrophy in a 6-year-old boy. J Pediatr Ophthalmol Strabismus. 2011; 48:e19–e22.
Article12. Ruiz-Moreno O, Calvo P, Ferrández B, Torrón C. Long-term outcomes of intravitreal ranibizumab for choroidal neovascularization secondary to Best's disease: 3-year follow-up. Acta Ophthalmol. 2012; 90:e574–e575.
Article13. Khan KN, Mahroo OA, Islam F, et al. Functional and anatomical outcomes of choroidal neovascularization complicating BEST1-related retinopathy. Retina. 2017; 37:1360–1370.
Article14. O'Gorman S, Flaherty WA, Fishman GA, Berson EL. Histopathologic findings in Best's vitelliform macular dystrophy. Arch Ophthalmol. 1988; 106:1261–1268.15. Kim HK, Rho CR, Lee WK, Kim KS. Optical coherence tomography findings in Best disease. J Korean Ophthalmol Soc. 2008; 49:845–852.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Availability of Optical Coherence Tomography in Diagnosis and Classification of Choroidal Neovascularization
- A Case of Idiopathic Choroidal Neovascularization
- Subretinal Hemorrhages in High Myopia
- Laser-Induced Choroidal Neovascularization in Central Serous Chorioretinopathy: 4 Cases
- A Case of Choroidal Neovascularization Occurring after Macular Hole Surgery