Anesth Pain Med.
2019 Jul;14(3):364-369. 10.17085/apm.2019.14.3.364.
The effect of gender and age on postoperative pain in laparoscopic cholecystectomy: a prospective observational study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Dong-A University College of Medicine, Busan, Korea. Parksy@dau.ac.kr
- KMID: 2454824
- DOI: http://doi.org/10.17085/apm.2019.14.3.364
Abstract
- BACKGROUND
Gender and age are known factors that affect postoperative pain. The purpose of this study was to investigate the effect of gender and age on postoperative pain and analgesic consumptions after laparoscopic cholecystectomy.
METHODS
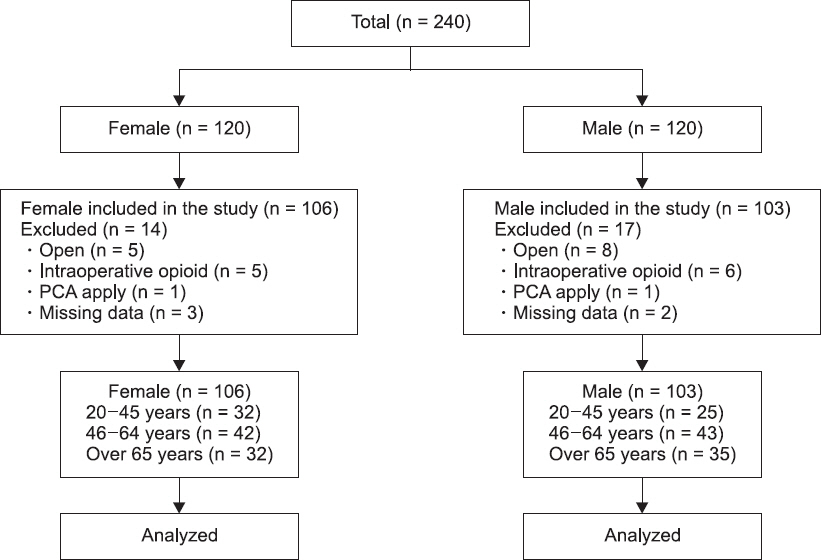
We studied 240 adult patients (120 female patients and 120 male patients) who underwent elective 3-port laparoscopic cholecystectomy under general anesthesia. The numerical rating scale (NRS) scores were assessed before surgery, when the patient arrived in the recovery room, and at 8, 16, and 24 h after surgery. Analgesic consumptions in the recovery room and at 24 h postoperatively were evaluated. We compared the NRS scores and quantity of analgesics between the gender groups and the age groups (20-45, 46-64, and ≥ 65 years old).
RESULTS
Compared to male patients, female patients had higher NRS scores (6 [5, 7] vs. 5 [4, 6]; P = 0.001) and required a higher dose of fentanyl (0.94 ± 0.47 µg/kg vs. 0.79 ± 0.41 µg/kg; P = 0.011) in the recovery room. The younger female patients (20-45 and 46-64 years old) required a higher dose of fentanyl than those older than 65 years of age in the recovery room.
CONCLUSIONS
Female patients exhibit higher NRS scores and greater consumptions of analgesics than male patients immediately postoperatively. Younger female patients require more analgesics than elderly patients in the recovery room.
Keyword
MeSH Terms
Figure
Reference
-
1. Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience:results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003; 97:534–40. DOI: 10.1213/01.ANE.0000068822.10113.9E. PMID: 12873949.2. Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain:risk factors and protective factors. Expert Rev Neurother. 2009; 9:723–44. DOI: 10.1586/ern.09.20. PMID: 19402781.3. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain:risk factors and prevention. Lancet. 2006; 367:1618–25. DOI: 10.1016/S0140-6736(06)68700-X. PMID: 16698416.4. Fletcher D, Fermanian C, Mardaye A, Aegerter P. Pain and Regional Anesthesia Committee of the French Anesthesia and Intensive Care Society (SFAR). A patient-based national survey on postoperative pain management in France reveals significant achievements and persistent challenges. Pain. 2008; 137:441–51. DOI: 10.1016/j.pain.2008.02.026. PMID: 18417292.5. Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption:a qualitative systematic review. Anesthesiology. 2009; 111:657–77. DOI: 10.1097/ALN.0b013e3181aae87a. PMID: 19672167.6. Tighe PJ, Le-Wendling LT, Patel A, Zou B, Fillingim RB. Clinically derived early postoperative pain trajectories differ by age, sex, and type of surgery. Pain. 2015; 156:609–17. DOI: 10.1097/01.j.pain.0000460352.07836.0d. PMID: 25790453. PMCID: PMC4367128.7. Zheng H, Schnabel A, Yahiaoui-Doktor M, Meissner W, Van Aken H, Zahn P, et al. Age and preoperative pain are major confounders for sex differences in postoperative pain outcome:a prospective database analysis. PLoS One. 2017; 12:e0178659. DOI: 10.1371/journal.pone.0178659. PMID: 28586373. PMCID: PMC5460859.8. Rosseland LA, Stubhaug A. Gender is a confounding factor in pain trials:women report more pain than men after arthroscopic surgery. Pain. 2004; 112:248–53. DOI: 10.1016/j.pain.2004.08.028. PMID: 15561379.9. Kang DH, Kim DS, Kim JD, Kim JW. A comparison of fentanyl and morphine for patient controlled analgesia after laparoscopic cholecystectomy. Anesth Pain Med. 2013; 8:21–5.10. Fillingim RB, Ness TJ, Glover TL, Campbell CM, Hastie BA, Price DD, et al. Morphine responses and experimental pain:sex differences in side effects and cardiovascular responses but not analgesia. J Pain. 2005; 6:116–24. DOI: 10.1016/j.jpain.2004.11.005. PMID: 15694878.11. Fillingim RB, Maixner W. Gender differences in the responses to noxious stimuli. Pain Forum. 1995; 4:209–21. DOI: 10.1016/S1082-3174(11)80022-X.12. Aubrun F, Salvi N, Coriat P, Riou B. Sex- and age-related differences in morphine requirements for postoperative pain relief. Anesthesiology. 2005; 103:156–60. DOI: 10.1097/00000542-200507000-00023. PMID: 15983468.13. Cepeda MS, Carr DB. Women experience more pain and require more morphine than men to achieve a similar degree of analgesia. Anesth Analg. 2003; 97:1464–8. DOI: 10.1213/01.ANE.0000080153.36643.83. PMID: 14570666.14. Zeidan A, Al-Temyatt S, Mowafi H, Ghattas T. Gender-related difference in postoperative pain after laparoscopic Roux-En-Y gastric bypass in morbidly obese patients. Obes Surg. 2013; 23:1880–4. DOI: 10.1007/s11695-013-0996-x. PMID: 23695438.15. Theodoraki K, Staikou C, Fassoulaki A. Postoperative pain after major bdominal surgery:is it gender related?An observational prospective study. Pain Pract. 2014; 14:613–9. DOI: 10.1111/papr.12114. PMID: 24024825.16. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997; 86:10–23. DOI: 10.1097/00000542-199701000-00004. PMID: 9009935.17. Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011; 152:2399–404. DOI: 10.1016/j.pain.2011.07.005. PMID: 21856077.18. Jensen MP, Engel JM, McKearnan KA, Hoffman AJ. Validity of pain intensity assessment in persons with cerebral palsy:a comparison of six scales. J Pain. 2003; 4:56–63. DOI: 10.1054/jpai.2003.9. PMID: 14622716.19. Buckenmaier CC 3rd, Galloway KT, Polomano RC, McDuffie M, Kwon N, Gallagher RM. Preliminary validation of the Defense and Veterans Pain Rating Scale (DVPRS) in a military population. Pain Med. 2013; 14:110–23. DOI: 10.1111/j.1526-4637.2012.01516.x. PMID: 23137169.20. Fillingim RB, Ness TJ. Sex-related hormonal influences on pain and analgesic responses. Neurosci Biobehav Rev. 2000; 24:485–501. DOI: 10.1016/S0149-7634(00)00017-8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Preoperative Dexamethasone Administration, according to Age and Gender on Postoperative Pain in Patients who Undergo Laparoscopic Choelecystectomy
- Postoperative nausea and vomiting after capsicum plaster at the P6 acupoint after laparoscopic cholecystectomy according to gender
- Effects of Preoperative Dexamethasone on Postoperative Pain after Laparoscopic Cholecystectomy
- Comparison of Laparoscopic Cholecystectomy and Minilaparotomy Cholecystectomy
- Laparoscopic Cholecystectomy in the Second Trimester of Pregnancy