J Korean Soc Radiol.
2019 May;80(3):477-489. 10.3348/jksr.2019.80.3.477.
Effectiveness and Influencing Factors of Percutaneous Transluminal Angioplasty for Stenosis of Transposed Brachiobasilic Arteriovenous Fistula
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Seoul Hospital, Seoul, Korea. intervention.kim@gmail.com
- 2Department of Radiology, Soonchunhyang University Gumi Hospital, Gumi, Korea.
- 3Department of Radiology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 4Department of Radiology, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- KMID: 2454027
- DOI: http://doi.org/10.3348/jksr.2019.80.3.477
Abstract
- PURPOSE
To evaluate effectiveness of percutaneous transluminal angioplasty (PTA) for transposed brachiobasilic arteriovenous fistula (tBBAVF), and to analyze the factors influencing patency after PTA.
MATERIALS AND METHODS
In 101 patients who underwent operation for tBBAVF from January 2006 to February 2008, we identified 42 patients undergoing PTA. We conducted a retrospective analysis of sequential PTAs in these patients from 2006 to 2017.
RESULTS
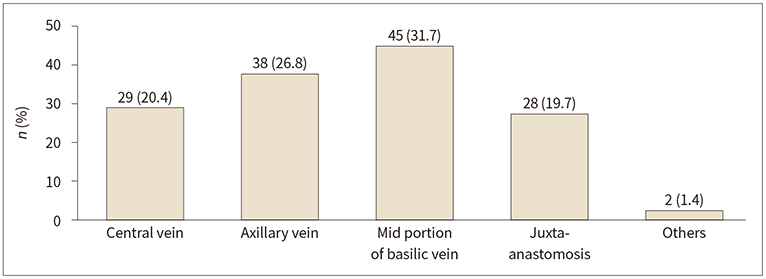
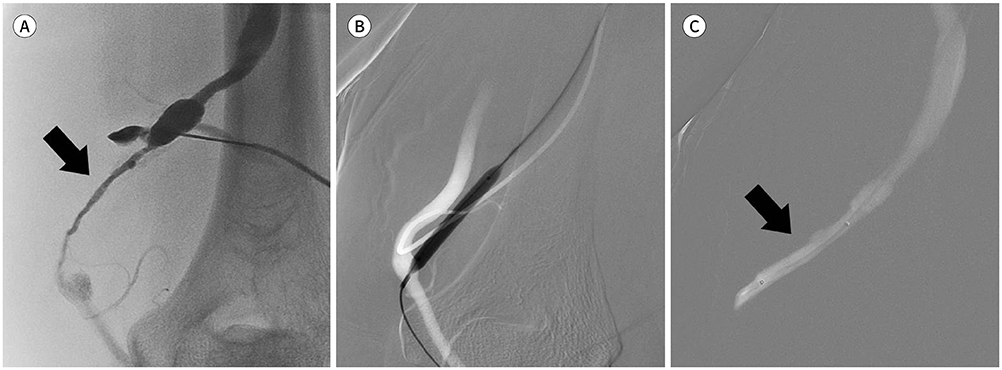
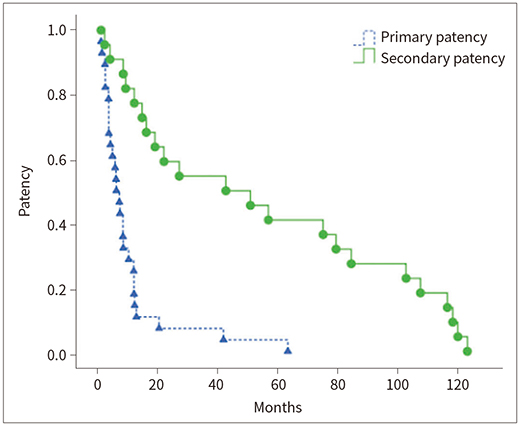
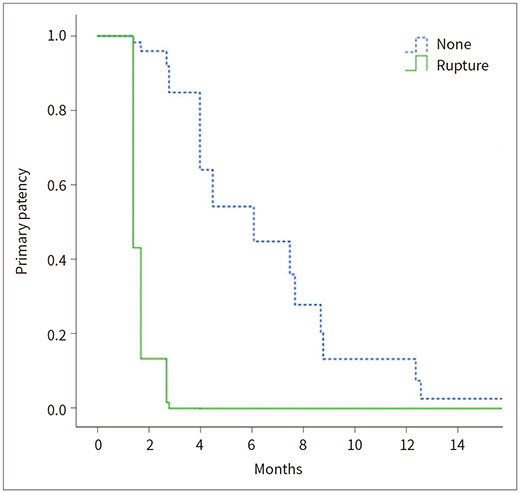
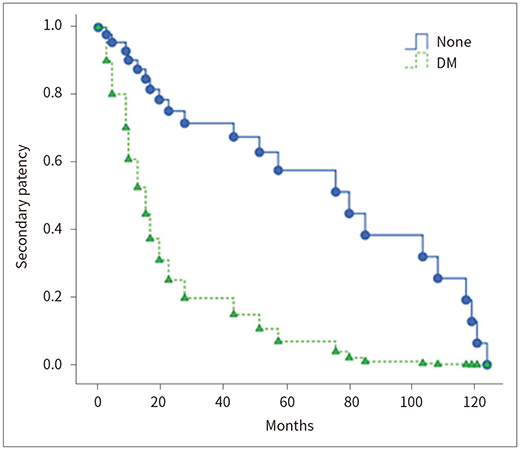
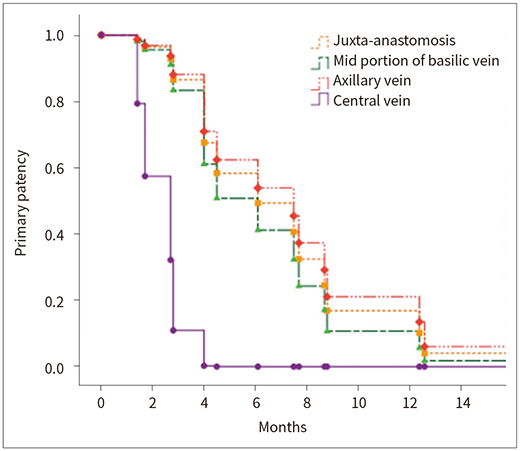
A total of 100 PTAs were performed. The technical success rate was 93% and the clinical success was 100%. Only ruptures occurred in 12% as minor complications. Primary patency rate was 61%, 29%, 7%, and secondary patency was 91%, 82%, 59% at 6, 12, and 24 months, respectively. Primary patency rate was lower in tBBAVF with rupture (p = 0.024). Secondary patency rate was significantly lower in the diabetes (p = 0.002).
CONCLUSION
Repetitive PTAs in tBBAVF are acceptable due to excellent secondary patency. Primary patency of tBBAVF is low in patients with rupture. Diabetes itself has a significant effect on secondary patency.
MeSH Terms
Figure
Reference
-
1. III. NKF-K/DOQI clinical practice guidelines for vascular access: update 2000. Am J Kidney Dis. 2001; 37:S137–S181.2. Dagher F, Gelber R, Ramos E, Sadler J. The use of basilic vein and brachial artery as an A-V fistula for long term hemodialysis. J Surg Res. 1976; 20:373–376.
Article3. Oliver MJ, McCann RL, Indridason OS, Butterly DW, Schwab SJ. Comparison of transposed brachiobasilic fistulas to upper arm grafts and brachiocephalic fistulas. Kidney Int. 2001; 60:1532–1539.
Article4. Weale AR, Bevis P, Neary WD, Lear PA, Mitchell DC. A comparison between transposed brachiobasilic arteriovenous fistulas and prosthetic brachioaxillary access grafts for vascular access for hemodialysis. J Vasc Surg. 2007; 46:997–1004.
Article5. Turmel-Rodrigues L, Pengloan J, Baudin S, Testou D, Abaza M, Dahdah G, et al. Treatment of stenosis and thrombosis in haemodialysis fistulas and grafts by interventional radiology. Nephrol Dial Transplant. 2000; 15:2029–2036.6. Clark TW, Hirsch DA, Jindal KJ, Veugelers PJ, LeBlanc J. Outcome and prognostic factors of restenosis after percutaneous treatment of native hemodialysis fistulas. J Vasc Interv Radiol. 2002; 13:51–59.
Article7. Rajan DK, Bunston S, Misra S, Pinto R, Lok CE. Dysfunctional autogenous hemodialysis fistulas: outcomes after angioplasty--are there clinical predictors of patency? Radiology. 2004; 232:508–515.
Article8. Turmel-Rodrigues L, Pengloan J, Bourquelot P. Interventional radiology in hemodialysis fistulae and grafts: a multidisciplinary approach. Cardiovasc Intervent Radiol. 2002; 25:3–16.
Article9. Glass C, Porter J, Singh M, Gillespie D, Young K, Illig K. A large-scale study of the upper arm basilic transposition for hemodialysis. Ann Vasc Surg. 2010; 24:85–91.
Article10. Gilmore J. KDOQI clinical practice guidelines and clinical practice recommendations—2006 updates. Nephrol Nurs J. 2006; 33:487–488.11. Neuen BL, Gunnarsson R, Baer RA, Tosenovsky P, Green SJ, Golledge J, et al. Factors associated with patency following angioplasty of hemodialysis fistulae. J Vasc Interv Radiol. 2014; 25:1419–1426.
Article12. Maeda K, Furukawa A, Yamasaki M, Murata K. Percutaneous transluminal angioplasty for Brescia-Cimino hemodialysis fistula dysfunction: technical success rate, patency rate and factors that influence the results. Eur J Radiol. 2005; 54:426–430.
Article13. Heye S, Maleux G, Vaninbroukx J, Claes K, Kuypers D, Oyen R. Factors influencing technical success and outcome of percutaneous balloon angioplasty in de novo native hemodialysis arteriovenous fistulas. Eur J Radiol. 2012; 81:2298–2303.
Article14. Simons ME, Clark TW, Rajan DK. The woggle technique: a new method of suture closure of hemodialysis arteriovenous grafts and fistulas after percutaneous interventions. J Vasc Interv Radiol. 2001; 12:S30.15. Cohen MA, Kumpe DA, Durham JD, Zwerdlinger SC. Improved treatment of thrombosed hemodialysis access sites with thrombolysis and angioplasty. Kidney Int. 1994; 46:1375–1380.
Article16. Goo DE, Kim JH, Park ST, Chang YW, Kwon KH, Choi DL, et al. Usefulness of thromboaspiration with desilets-Hoffman sheath in thrombosed hemodialysis access graft. J Korean Radiol Soc. 2004; 51:45–53.
Article17. Turmel-Rodrigues L, Pengloan J, Rodrigue H, Brillet G, Lataste A, Pierre D, et al. Treatment of failed native arteriovenous fistulae for hemodialysis by interventional radiology. Kidney Int. 2000; 57:1124–1140.
Article18. Gray RJ, Sacks D, Martin LG, Trerotola SO;. Reporting standards for percutaneous interventions in dialysis access. J Vasc Interv Radiol. 2003; 14:S433–S442.
Article19. Jeong SM, Kim JH, Byun SS, Kang JM, Choi ST, Kim JW, et al. Effect of percutaneous transluminal angioplasty on the stenosis of autogenous radiocephalic arteriovenous fistula for hemodialysis. J Korean Soc Radiol. 2016; 74:105–113.
Article20. Trerotola SO, Kwak A, Clark TW, Mondschein JI, Patel AA, Soulen MC, et al. Prospective study of balloon inflation pressures and other technical aspects of hemodialysis access angioplasty. J Vasc Interv Radiol. 2005; 16:1613–1618.
Article21. Manninen HI, Kaukanen ET, Ikäheimo R, Karhapää P, Lahtinen T, Matsi P, et al. Brachial arterial access: endovascular treatment of failing Brescia-Cimino hemodialysis fistulas—initial success and long-term results. Radiology. 2001; 218:711–718.
Article22. Beathard GA. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992; 42:1390–1397.
Article23. Hodges TC, Fillinger MF, Zwolak RM, Walsh DB, Bech F, Cronenwett JL. Longitudinal comparison of dialysis access methods: risk factors for failure. J Vasc Surg. 1997; 26:1009–1019.24. Quinn SF, Schuman ES, Demlow TA, Standage BA, Ragsdale JW, Green GS, et al. Percutaneous transluminal angioplasty versus endovascular stent placement in the treatment of venous stenoses in patients undergoing hemodialysis: intermediate results. J Vasc Interv Radiol. 1995; 6:851–855.
Article25. Funaki B, Szymski GX, Leef JA, Rosenblum JD, Burke R, Hackworth CA. Wallstent deployment to salvage dialysis graft thrombolysis complicated by venous rupture: early and intermediate results. AJR Am J Roentgenol. 1997; 169:1435–1437.
Article26. Dale JD, Dolmatch BL, Duch JM, Winder R, Davidson IJ. Expanded polytetrafluoroethylene-covered stent treatment of angioplasty-related extravasation during hemodialysis access intervention: technical and 180-day patency. J Vasc Interv Radiol. 2010; 21:322–326.
Article27. Manninen HI, Kaukanen E, Mäkinen K, Karhapää P. Endovascular salvage of nonmaturing autogenous hemodialysis fistulas: comparison with endovascular therapy of failing mature fistulas. J Vasc Interv Radiol. 2008; 19:870–876.
Article28. Forauer AR, Hoffer EK, Homa K. Dialysis access venous stenoses: treatment with balloon angioplasty—1-versus 3-minute inflation times. Radiology. 2008; 249:375–381.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of arteriovenous fistula with drainage into the coronary sinus during the percutaneous tranluminal coronary angioplasty of chronic total occlusion of circumflex coronary artery
- Successful Treatment of Resistant Arteriovenous Fistula Stenosis by Cutting Balloon Angioplasty
- Treatment of an Immature Autogenous Arteriovenous Fistula with Percutaneous Transluminal Angioplasty
- Effect of Percutaneous Transluminal Angioplasty on the Stenosis of Autogenous Radiocephalic Arteriovenous Fistula for Hemodialysis
- Percutaneous transluminal coronary angioplasty for ostial stenosis of the left coronary artery