J Korean Soc Radiol.
2019 May;80(3):412-424. 10.3348/jksr.2019.80.3.412.
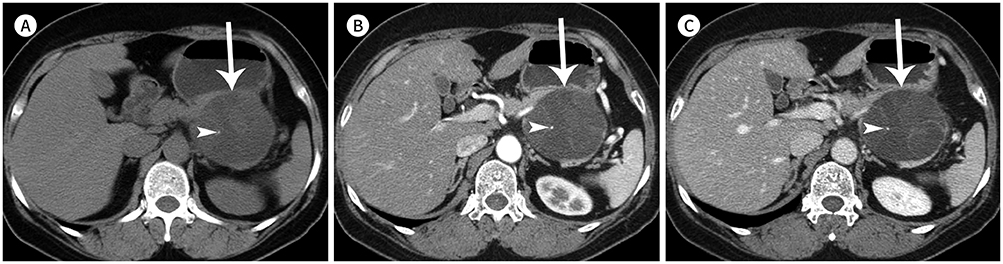
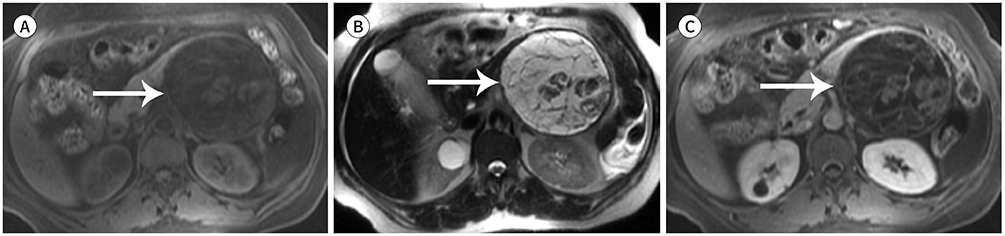
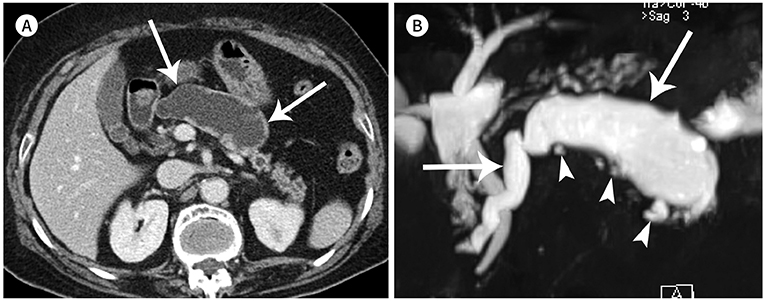
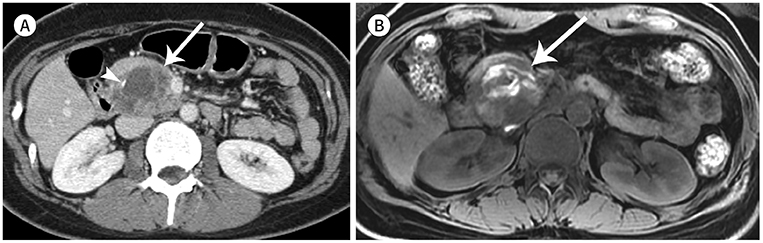
Imaging Diagnosis and Management of Pancreatic Cystic Neoplasms
- Affiliations
-
- 1Department of Radiology, Chonnam National University Medical School, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- 2Department of Radiology, Chonnam National University Medical School, Chonnam National University Hospital, Gwangju, Korea. kjradsss@gmail.com
- KMID: 2454023
- DOI: http://doi.org/10.3348/jksr.2019.80.3.412
Abstract
- Incidental pancreatic cysts may show various clinical courses, from benign to invasive malignant lesions. To adequately treat asymptomatic pancreatic cystic tumors, accurate diagnosis is needed. However, in many cases, clinical and imaging findings do not provide a definitive diagnosis. Therefore, if there is any evidence suggestive of a malignant lesion, the lesion should be removed surgically. If not, follow-up should be done continuously. To date, several academic societies have issued guidelines that suggest malignant features and follow-up strategies for incidental pancreatic cysts. These guidelines ultimately aim to increase the cure rate by surgical resection and reduce the likelihood of unnecessary surgery by early and efficient screening of high-risk cases. The purpose of this study is to review the relevant findings for the definitive diagnosis of relatively common pancreatic cystic neoplasms and to discuss guidelines for the management of incidental pancreatic cystic neoplasms.
MeSH Terms
Figure
Reference
-
1. Lee KS, Sekhar A, Rofsky NM, Pedrosa I. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol. 2010; 105:2079–2084.2. De Jong K, Nio CY, Hermans JJ, Dijkgraaf MG, Gouma DJ, Van Eijck CH, et al. High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin Gastroenterol Hepatol. 2010; 8:806–811.3. Laffan TA, Horton KM, Klein AP, Berlanstein B, Siegelman SS, Kawamoto S, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008; 191:802–807.4. Zhang XM, Mitchell DG, Dohke M, Holland GA, Parker L. Pancreatic cysts: depiction on single-shot fast spin-echo MR images. Radiology. 2002; 223:547–553.5. Scheiman JM, Hwang JH, Moayyedi P. American gastroenterological association technical review on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015; 148:824–848.e22.6. Sahani DV, Kambadakone A, Macari M, Takahashi N, Chari S, Fernandez-del Castillo C. Diagnosis and management of cystic pancreatic lesions. AJR Am J Roentgenol. 2013; 200:343–354.7. Kim YH, Saini S, Sahani D, Hahn PF, Mueller PR, Auh YH. Imaging diagnosis of cystic pancreatic lesions: pseudocyst versus nonpseudocyst. Radiographics. 2005; 25:671–685.8. Sahani DV, Kadavigere R, Saokar A, Fernandez-del Castillo C, Brugge WR, Hahn PF. Cystic pancreatic lesions: a simple imaging-based classification system for guiding management. Radiographics. 2005; 25:1471–1484.9. Kim SY, Lee JM, Kim SH, Shin KS, Kim YJ, An SK, et al. Macrocystic neoplasms of the pancreas: CT differentiation of serous oligocystic adenoma from mucinous cystadenoma and intraductal papillary mucinous tumor. AJR Am J Roentgenol. 2006; 187:1192–1198.10. Farrell JJ, Fernández-del Castillo C. Pancreatic cystic neoplasmss: management and unanswered questions. Gastroenterology. 2013; 144:1303–1315.11. Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017; 17:738–753.12. Bollen TL, Wessels FJ. Radiological workup of cystic neoplasms of the pancreas. Visc Med. 2018; 34:182–190.13. Curry CA, Eng J, Horton KM, Urban B, Siegelman S, Kuszyk BS, et al. CT of primary cystic pancreatic neoplasms: can CT be used for patient triage and treatment? AJR Am J Roentgenol. 2000; 175:99–103.14. Visser BC, Yeh BM, Qayyum A, Way LW, McCulloch CE, Coakley FV. Characterization of cystic pancreatic masses: relative accuracy of CT and MRI. AJR Am J Roentgenol. 2007; 189:648–656.15. Lennon AM, Manos LL, Hruban RH, Ali SZ, Fishman EK, Kamel IR, et al. Role of a multidisciplinary clinic in the management of patients with pancreatic cysts: a single-center cohort study. Ann Surg Oncol. 2014; 21:3668–3674.16. Chiang AL, Lee LS. Clinical approach to incidental pancreatic cysts. World J Gastroenterol. 2016; 22:1236–1245.17. Del Chiaro M, Verbeke C, Salvia R, Klöppel G, Werner J, McKay C, et al. European experts consensus statement on cystic tumours of the pancreas. Dig Liver Dis. 2013; 45:703–711.18. Gore RM, Wenzke DR, Thakrar KH, Newmark GM, Mehta UK, Berlin JW. The incidental cystic pancreas mass: a practical approach. Cancer Imaging. 2012; 12:414–421.19. Choi SH, Park SH, Kim KW, Lee JY, Lee SS. Progression of unresected intraductal papillary mucinous neoplasms of the pancreas to cancer: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2017; 15:1509–1520.e4.20. Valsangkar NP, Morales-Oyarvide V, Thayer SP, Ferrone CR, Wargo JA, Warshaw AL, et al. 851 resected cystic tumors of the pancreas: a 33-year experience at the Massachusetts General Hospital. Surgery. 2012; 152:S4–S12.21. Fernández-Del Castillo C, Tanaka M. Management of pancreatic cysts: the evidence is not here yet. Gastroenterology. 2015; 148:685–687.22. Jais B, Rebours V, Malleo G, Salvia R, Fontana M, Maggino L, et al. Serous cystic neoplasm of the pancreas: a multinational study of 2622 patients under the auspices of the International Association of Pancreatology and European Pancreatic Club (European Study Group on Cystic Tumors of the Pancreas). Gut. 2016; 65:305–312.23. Freeny PC, Saunders MD. Moving beyond morphology: new insights into the characterization and management of cystic pancreatic lesions. Radiology. 2014; 272:345–363.24. Menard A, Tomlinson G, Cleary S, Wei A, Gallinger S, Haider MA. Serous cystadenomas of the pancreas: long-term follow-up measurement of growth rate. Can Assoc Radiol J. 2011; 62:190–196.25. Chu LC, Singhi AD, Haroun RR, Hruban RH, Fishman EK. The many faces of pancreatic serous cystadenoma: radiologic and pathologic correlation. Diagn Interv Imaging. 2017; 98:191–202.26. Javadi S, Menias CO, Korivi BR, Shaaban AM, Patnana M, Alhalabi K, et al. Pancreatic calcifications and calcified pancreatic masses: pattern recognition approach on CT. AJR Am J Roentgenol. 2017; 209:77–87.27. Sakorafas GH, Smyrniotis V, Reid-Lombardo KM, Sarr MG. Primary pancreatic cystic neoplasms revisited: part II. Mucinous cystic neoplasms. Surg Oncol. 2011; 20:e93–e101.28. Reddy RP, Smyrk TC, Zapiach M, Levy MJ, Pearson RK, Clain JE, et al. Pancreatic mucinous cystic neoplasm defined by ovarian stroma: demographics, clinical features, and prevalence of cancer. Clin Gastroenterol Hepatol. 2004; 2:1026–1031.29. Vege SS, Ziring B, Jain R, Moayyedi P. Clinical Guidelines Committee. American Gastroenterology Association. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015; 148:819–822.30. Megibow AJ, Baker ME, Morgan DE, Kamel IR, Sahani DV, Newman E, et al. Management of incidental pancreatic cysts: a white paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2017; 14:911–923.31. European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018; 67:789–804.32. Kim GE, Shin SS, Kim JW, Heo SH, Lim HS, Jun CH, et al. Incidental, small (< 3 cm), unilocular, pancreatic cysts: factors that predict lesion progression during imaging surveillance. Korean J Radiol. 2017; 18:915–925.33. Manfredi R, Ventriglia A, Mantovani W, Mehrabi S, Boninsegna E, Zamboni G, et al. Mucinous cystic neoplasms and serous cystadenomas arising in the body-tail of the pancreas: MR imaging characterization. Eur Radiol. 2015; 25:940–949.34. Perez-Johnston R, Narin O, Mino-Kenudson M, Ingkakul T, Warshaw AL, Fernandez-Del Castillo C, et al. Frequency and significance of calcification in IPMN. Pancreatology. 2013; 13:43–47.35. Campbell NM, Katz SS, Escalon JG, Do RK. Imaging patterns of intraductal papillary mucinous neoplasms of the pancreas: an illustrated discussion of the International Consensus Guidelines for the Management of IPMN. Abdom Imaging. 2015; 40:663–677.36. Kim JH, Hong SS, Kim YJ, Kim JK, Eun HW. Intraductal papillary mucinous neoplasm of the pancreas: differentiate from chronic pancreatits by MR imaging. Eur J Radiol. 2012; 81:671–676.37. Ganeshan DM, Paulson E, Tamm EP, Taggart MW, Balachandran A, Bhosale P. Solid pseudo-papillary tumors of the pancreas: current update. Abdom Imaging. 2013; 38:1373–1382.38. Anil G, Zhang J, Al Hamar NE, Nga ME. Solid pseudopapillary neoplasm of the pancreas: CT imaging features and radiologic-pathologic correlation. Diagn Interv Radiol. 2017; 23:94–99.39. Papavramidis T, Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J Am Coll Surg. 2005; 200:965–972.40. Chung YE, Kim MJ, Choi JY, Lim JS, Hong HS, Kim YC, et al. Differentiation of benign and malignant solid pseudopapillary neoplasms of the pancreas. J Comput Assist Tomogr. 2009; 33:689–694.41. Choi JY, Kim MJ, Kim JH, Kim SH, Lim JS, Oh YT, et al. Solid pseudopapillary tumor of the pancreas: typical and atypical manifestations. AJR Am J Roentgenol. 2006; 187:W178–W186.42. Yu MH, Lee JY, Kim MA, Kim SH, Lee JM, Han JK, et al. MR imaging features of small solid pseudopapillary tumors: retrospective differentiation from other small solid pancreatic tumors. AJR Am J Roentgenol. 2010; 195:1324–1332.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pathologic Features of Pancreatic Cystic Neoplasms
- Surgical Indications and Postsurgical Follow-up Strategy for Pancreatic Cystic Neoplasm
- Endoscopic Diagnosis of Pancreatic Cystic Tumors
- Pancreatic Cystic Neoplasm: Radiologic Evaluation and Differential Diagnosis
- Radiologic Findings of Pancreatic Cystic Neoplasms