Factors Affecting Radiation Exposure during Lumbar Epidural Steroid Injection: A Prospective Study in 759 Patients
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam 13620, Korea. joongmoahn@gmail.com
- 2Department of Law, Hanyang University, Seoul 04763, Korea.
- 3Department of Rehabilitation, National Rehabilitation Center, Seoul 01022, Korea.
- KMID: 2451414
- DOI: http://doi.org/10.3348/kjr.2016.17.3.405
Abstract
OBJECTIVE
To estimate and compare radiation exposure and intervention time during lumbar epidural steroid injection (ESI) 1) under different practitioners and methods with continuous fluoroscopic monitoring, and 2) under one practitioner with different methods and monitoring.
MATERIALS AND METHODS
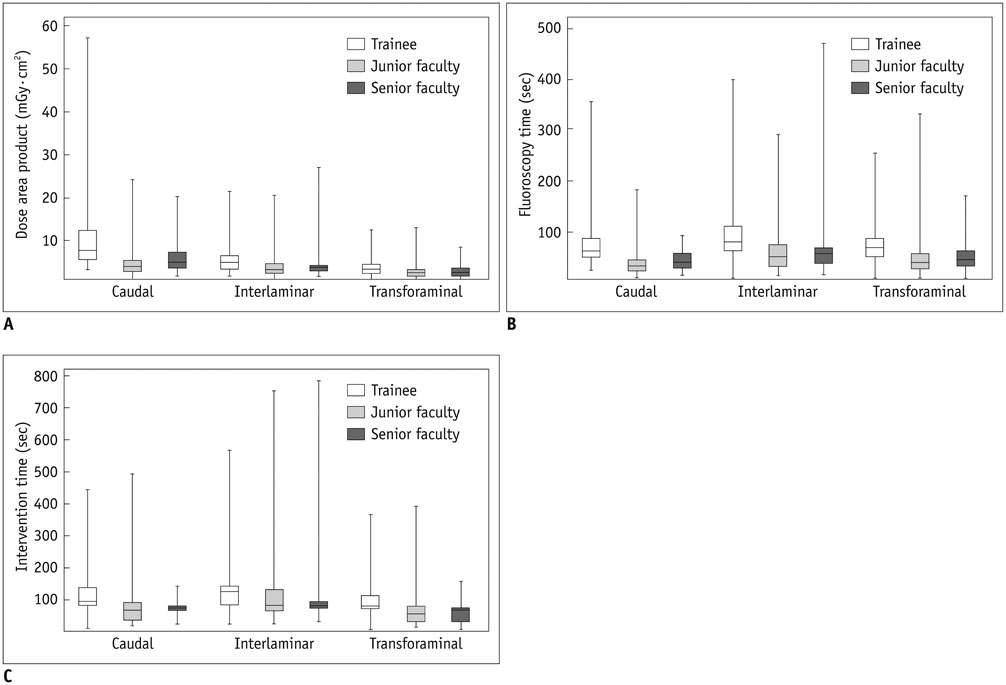
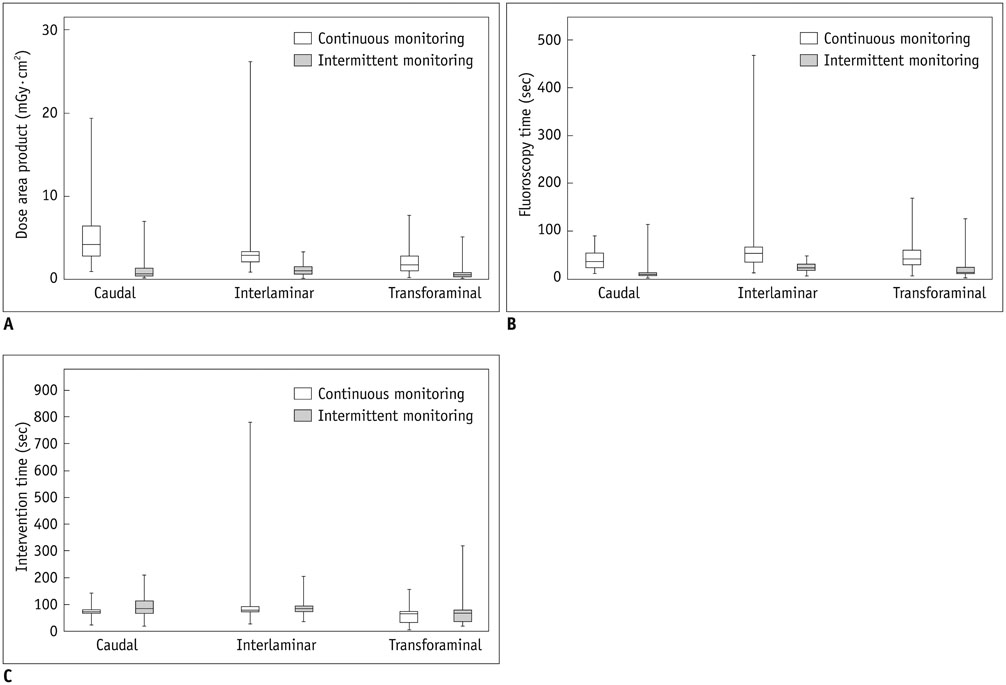
We consecutively recruited 804 patients who underwent lumbar ESI and 759 patients who underwent 922 interventions were included for analysis in this investigation. Three different practitioners (a senior faculty member, junior faculty member, trainee) performed lumbar ESI using different methods (caudal, interlaminar, transforaminal). The senior faculty member performed lumbar ESI under two different methods of fluoroscopic monitoring (continuous [CM] and intermittent monitoring [IM]). The dose area product (DAP) fluoroscopy time, and intervention time during lumbar ESI were compared for 1) ESI methods and practitioners under CM, and 2) ESI methods and monitoring.
RESULTS
With CM, interaction between the effects of the practitioner and the intervention on DAP was significant (p < 0.001), but not fluoroscopy time (p = 0.672) or intervention time (p = 0.852). The significant main effects included the practitioner and intervention on DAP, fluoroscopy time, and intervention time with CM (p < 0.001). DAPs and fluoroscopy time for caudal, interlaminar, and transforaminal ESI were higher with CM than with IM (p < 0.001). Intervention time did not differ between CM and IM.
CONCLUSION
Radiation exposure is dependent on the practitioners and methods and within the established safety limits during lumbar ESIs under CM. With an experienced practitioner, IM leads to less radiation exposure than CM.
MeSH Terms
Figure
Cited by 3 articles
-
The radiation safety education and the pain physicians' efforts to reduce radiation exposure
Tae Hee Kim, Seung Wan Hong, Nam Sik Woo, Hae Kyoung Kim, Jae Hun Kim
Korean J Pain. 2017;30(2):104-115. doi: 10.3344/kjp.2017.30.2.104.Comparison of clinical efficacy in epidural steroid injections through transforaminal or parasagittal approaches
Ji Hee Hong, Eun Kyul Park, Ki Bum Park, Ji Hoon Park, Sung Won Jung
Korean J Pain. 2017;30(3):220-228. doi: 10.3344/kjp.2017.30.3.220.Radiation safety: a focus on lead aprons and thyroid shields in interventional pain management
Bo Kyung Cheon, Cho Long Kim, Ka Ram Kim, Min Hye Kang, Jeong Ae Lim, Nam Sik Woo, Ka Young Rhee, Hae Kyoung Kim, Jae Hun Kim
Korean J Pain. 2018;31(4):244-252. doi: 10.3344/kjp.2018.31.4.244.
Reference
-
1. White AH, Derby R, Wynne G. Epidural injections for the diagnosis and treatment of low-back pain. Spine (Phila Pa 1976). 1980; 5:78–86.2. Bartynski WS, Grahovac SZ, Rothfus WE. Incorrect needle position during lumbar epidural steroid administration: inaccuracy of loss of air pressure resistance and requirement of fluoroscopy and epidurography during needle insertion. AJNR Am J Neuroradiol. 2005; 26:502–505.3. Liu SS, Melmed AP, Klos JW, Innis CA. Prospective experience with a 20-gauge Tuohy needle for lumbar epidural steroid injections: is confirmation with fluoroscopy necessary? Reg Anesth Pain Med. 2001; 26:143–146.4. Weil L, Frauwirth NH, Amirdelfan K, Grant D, Rosenberg JA. Fluoroscopic analysis of lumbar epidural contrast spread after lumbar interlaminar injection. Arch Phys Med Rehabil. 2008; 89:413–416.5. Botwin KP, Natalicchio J, Hanna A. Fluoroscopic guided lumbar interlaminar epidural injections: a prospective evaluation of epidurography contrast patterns and anatomical review of the epidural space. Pain Physician. 2004; 7:77–80.6. Stitz MY, Sommer HM. Accuracy of blind versus fluoroscopically guided caudal epidural injection. Spine (Phila Pa 1976). 1999; 24:1371–1376.7. Trentman TL, Rosenfeld DM, Seamans DP, Hentz JG, Stanek JP. Vasovagal reactions and other complications of cervical vs. lumbar translaminar epidural steroid injections. Pain Pract. 2009; 9:59–64.8. Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: two case reports. Pain Med. 2009; 10:1389–1394.9. Bogduk N, Dreyfuss P, Baker R, Yin W, Landers M, Hammer M, et al. Complications of spinal diagnostic and treatment procedures. Pain Med. 2008; 9:S11–S34.10. Fitzgibbon DR, Posner KL, Domino KB, Caplan RA, Lee LA, Cheney FW. American Society of Anesthesiologists. Chronic pain management: American Society of Anesthesiologists Closed Claims Project. Anesthesiology. 2004; 100:98–105.11. Manchikanti L, Cash KA, Moss TL, Pampati V. Radiation exposure to the physician in interventional pain management. Pain Physician. 2002; 5:385–393.12. Friedly J, Chan L, Deyo R. Increases in lumbosacral injections in the Medicare population: 1994 to 2001. Spine (Phila Pa 1976). 2007; 32:1754–1760.13. Manchikanti L, Cash KA, Moss TL, Rivera J, Pampati V. Risk of whole body radiation exposure and protective measures in fluoroscopically guided interventional techniques: a prospective evaluation. BMC Anesthesiol. 2003; 3:2.14. Rosenthal LS, Mahesh M, Beck TJ, Saul JP, Miller JM, Kay N, et al. Predictors of fluoroscopy time and estimated radiation exposure during radiofrequency catheter ablation procedures. Am J Cardiol. 1998; 82:451–458.15. Mahesh M. Fluoroscopy: patient radiation exposure issues. Radiographics. 2001; 21:1033–1045.16. Aufrichtig R, Xue P, Thomas CW, Gilmore GC, Wilson DL. Perceptual comparison of pulsed and continuous fluoroscopy. Med Phys. 1994; 21:245–256.17. Pfirrmann CW, Oberholzer PA, Zanetti M, Boos N, Trudell DJ, Resnick D, et al. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness--a study with patients and cadavers. Radiology. 2001; 221:704–711.18. Lee JW, Kim SH. Epidural steroid injection. Neurointervention. 2008; 3:20–27.19. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007; 37:1–332.20. 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 1991; 21:1–201.21. Shope TB. Radiation-induced skin injuries from fluoroscopy. Radiographics. 1996; 16:1195–1199.22. Turner JE. Atoms, radiation, and radiation protection. Weinheim: Wiley-VCH;2007.23. Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain: a systematic review. Pain Physician. 2009; 12:163–188.24. Reitman CA, Watters W 3rd. Subdural hematoma after cervical epidural steroid injection. Spine (Phila Pa 1976). 2002; 27:E174–E176.25. Rozin L, Rozin R, Koehler SA, Shakir A, Ladham S, Barmada M, et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol. 2003; 24:351–355.26. Goodman BS, Posecion LW, Mallempati S, Bayazitoglu M. Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr Rev Musculoskelet Med. 2008; 1:212–222.27. Karambatsakidou A, Tornvall P, Saleh N, Chouliaras T, Löfberg PO, Fransson A. Skin dose alarm levels in cardiac angiography procedures: is a single DAP value sufficient? Br J Radiol. 2005; 78:803–809.28. Bogaert E, Bacher K, Thierens H. A large-scale multicentre study in Belgium of dose area product values and effective doses in interventional cardiology using contemporary X-ray equipment. Radiat Prot Dosimetry. 2008; 128:312–323.29. Wagner LK, Eifel PJ, Geise RA. Potential biological effects following high X-ray dose interventional procedures. J Vasc Interv Radiol. 1994; 5:71–84.30. Shim DM, Kim YM, Oh SK, Lim CM, Kown BT. Radiation induced hand necrosis of an orthopaedic surgeon who had treated a patient with fluoroscopy-guided spine injection. J Korean Orthop Assoc. 2014; 49:250–254.31. Manchikanti L, Cash KA, Moss TL, Pampati V. Effectiveness of protective measures in reducing risk of radiation exposure in interventional pain management: a prospective evaluation. Pain Physician. 2003; 6:301–305.32. Botwin KP, Thomas S, Gruber RD, Torres FM, Bouchlas CC, Rittenberg JJ, et al. Radiation exposure of the spinal interventionalist performing fluoroscopically guided lumbar transforaminal epidural steroid injections. Arch Phys Med Rehabil. 2002; 83:697–701.33. Botwin KP, Freeman ED, Gruber RD, Torres-Rames FM, Bouchtas CG, Sanelli JT, et al. Radiation exposure to the physician performing fluoroscopically guided caudal epidural steroid injections. Pain Physician. 2001; 4:343–348.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Persistent Hiccup after Epidural Steroid Injection: Case reports
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy
- Hyperprolactinemia and Galactorrhea Following Single Epidural Steroid Injection
- Generalized Ecchymosis after Volumetric Caudal Steroid Injection for Lumbar Radiculopathy: A case report
- Epidural Steroid Injection