Korean J Radiol.
2016 Jun;17(3):351-363. 10.3348/kjr.2016.17.3.351.
Interventional Radiology in the Management of Visceral Artery Pseudoaneurysms: A Review of Techniques and Embolic Materials
- Affiliations
-
- 1Department of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi 110029, India. drmadhuks@gmail.com
- 2Department of Gastroenterology, All India Institute of Medical Sciences, New Delhi 110029, India.
- KMID: 2451410
- DOI: http://doi.org/10.3348/kjr.2016.17.3.351
Abstract
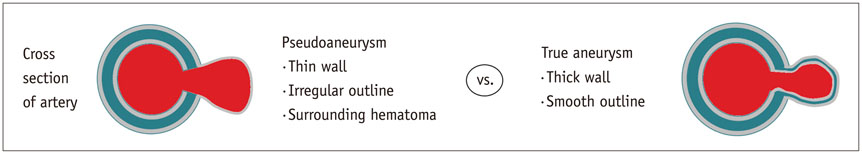
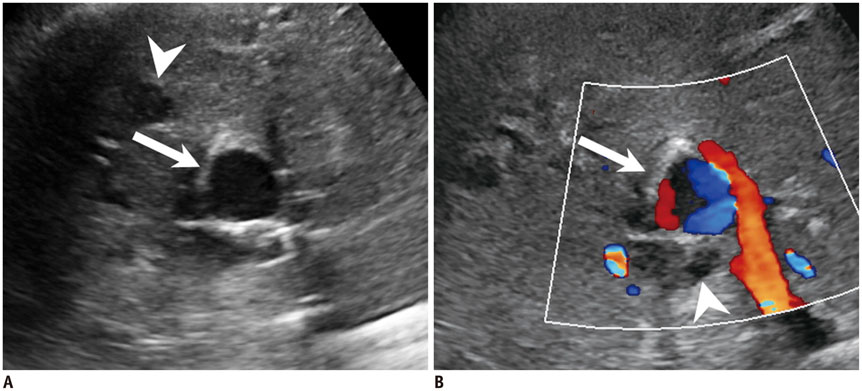
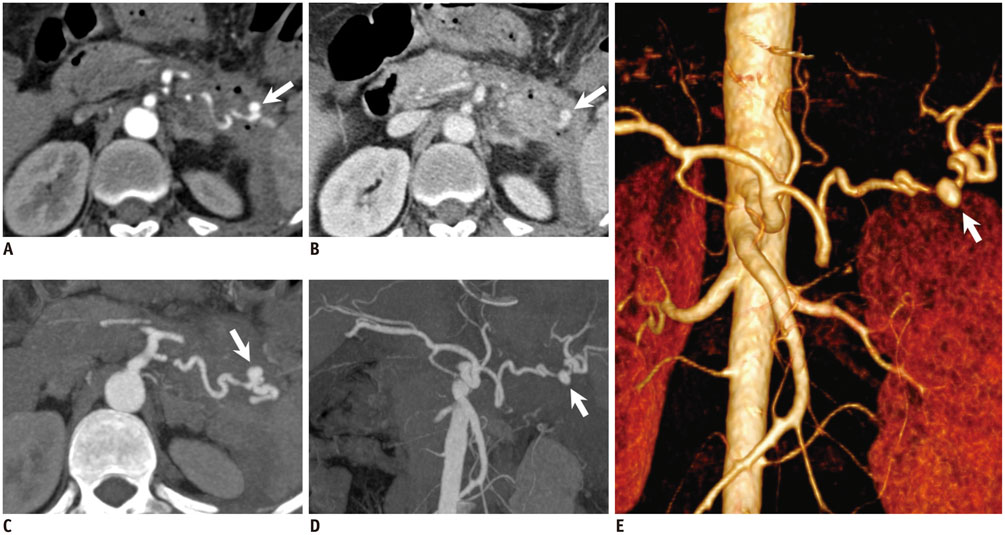
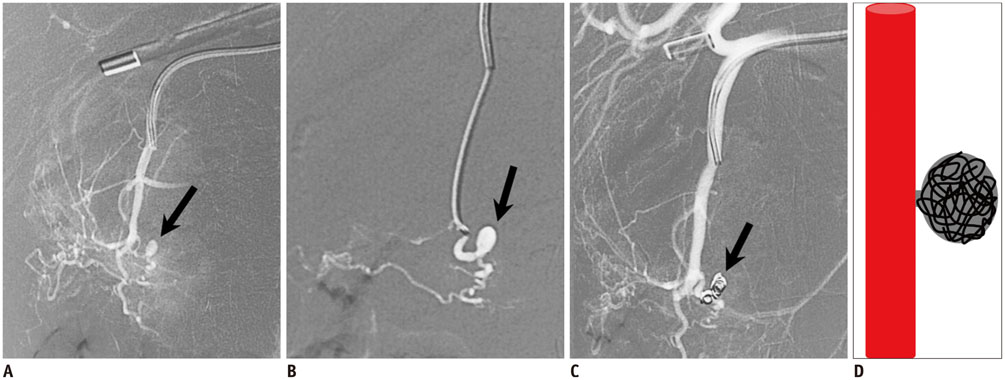
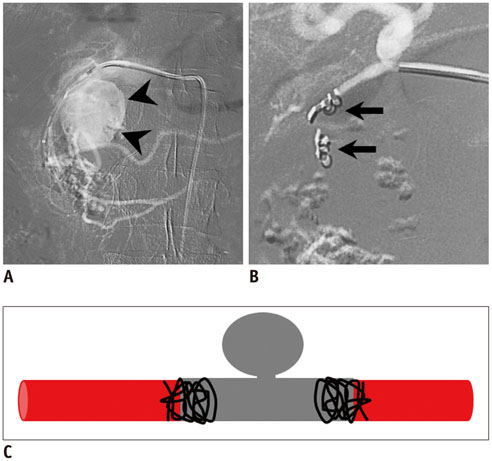
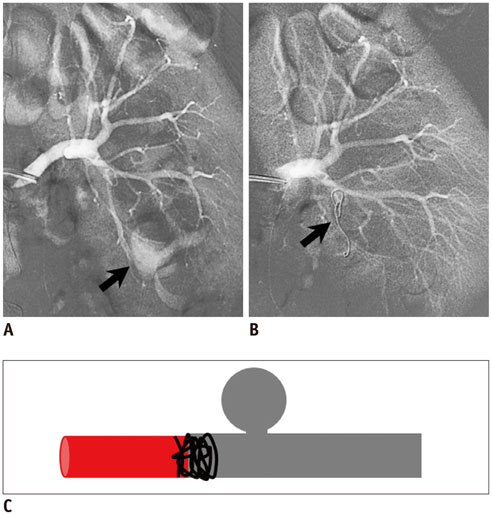
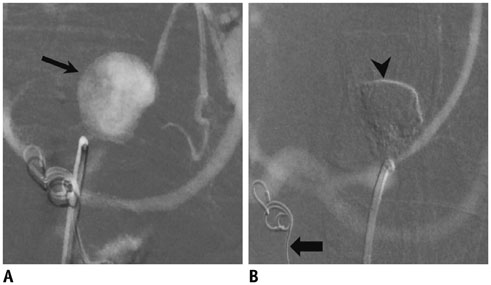
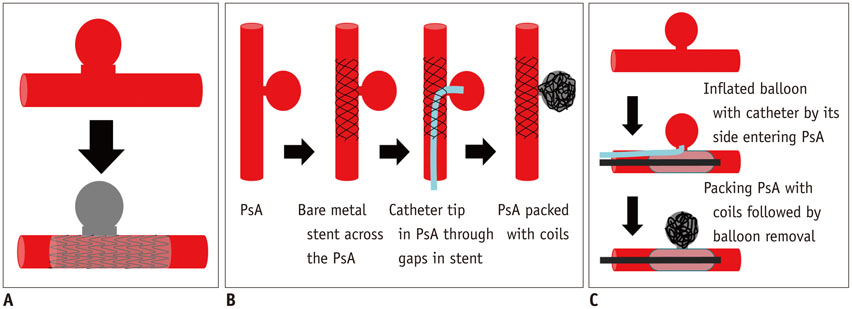
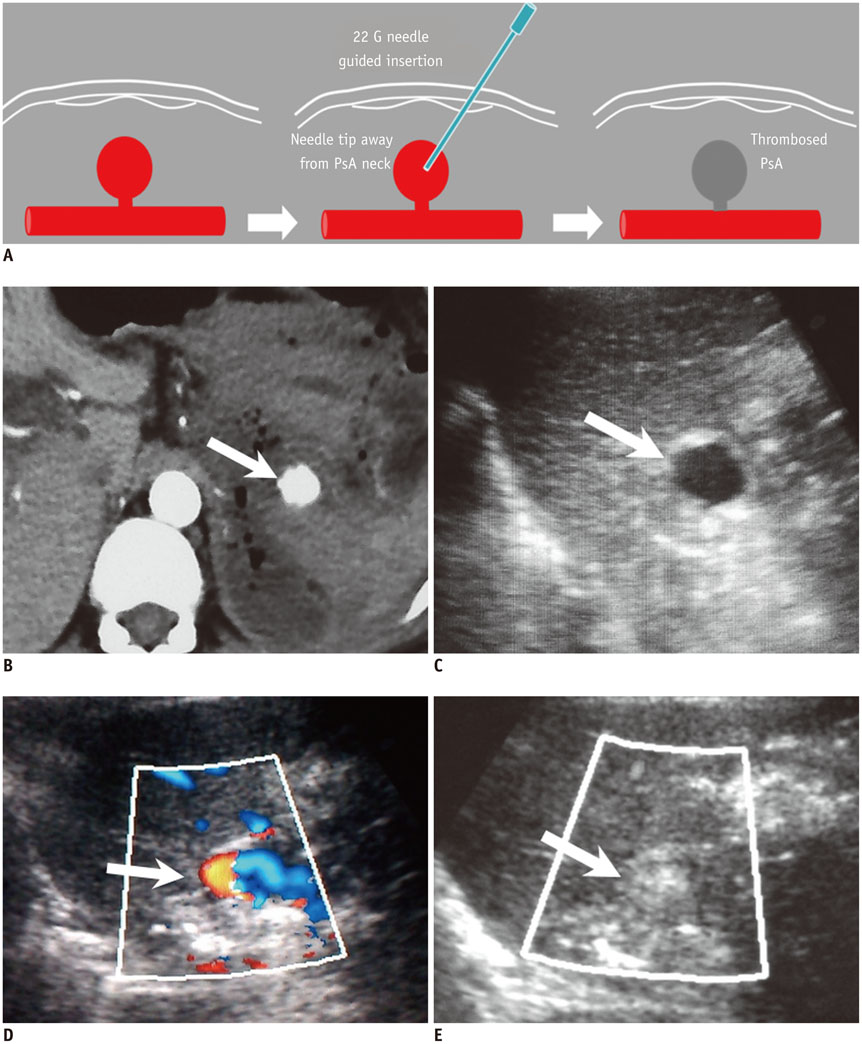
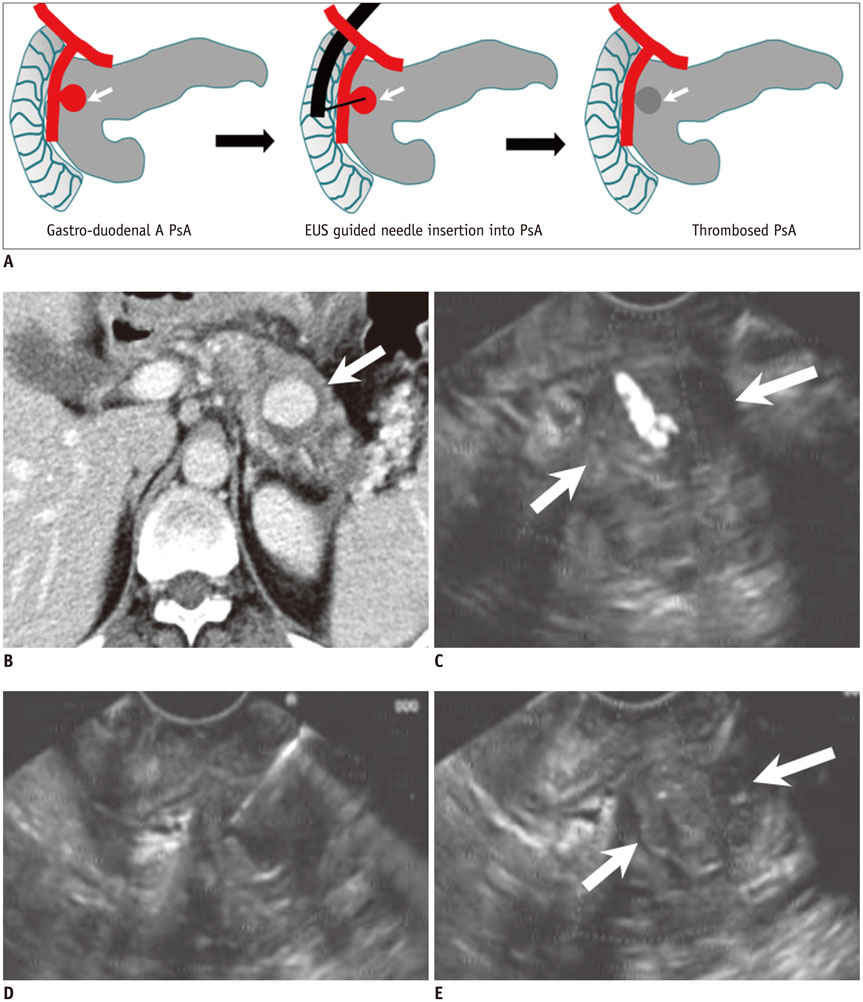
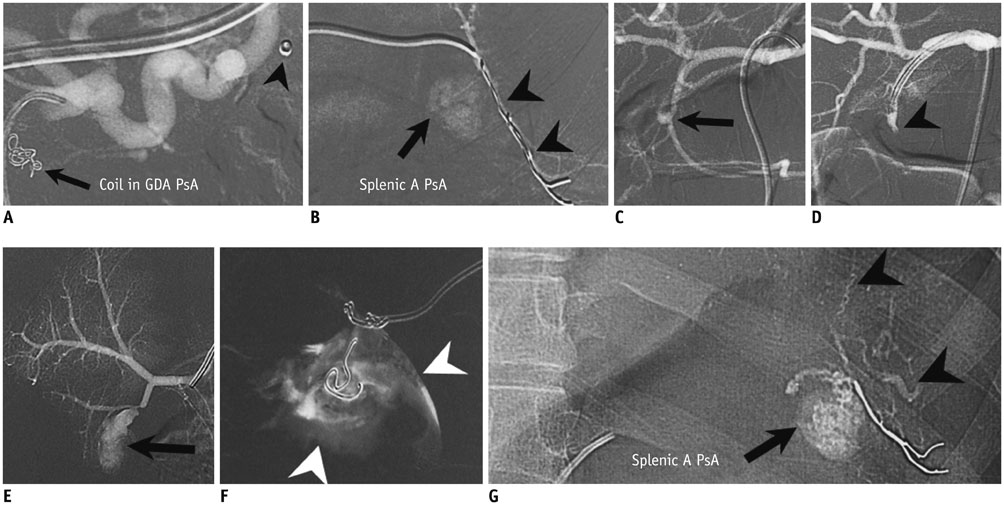
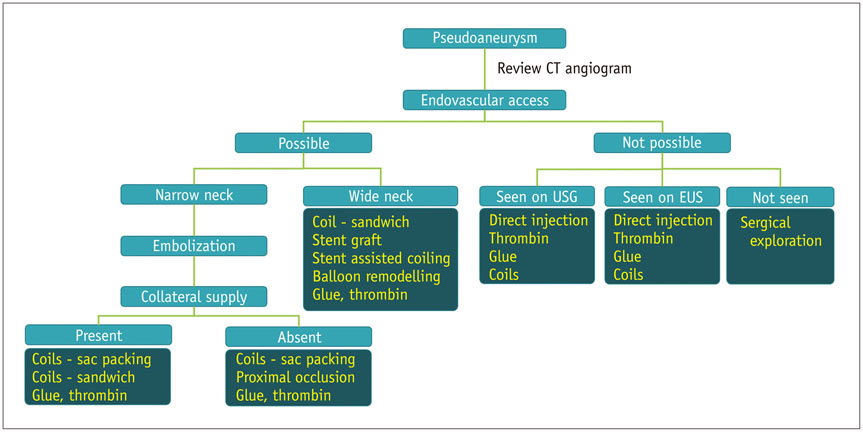
- Visceral artery pseudoaneurysms occur mostly as a result of inflammation and trauma. Owing to high risk of rupture, they require early treatment to prevent lethal complications. Knowledge of the various approaches of embolization of pseudoaneurysms and different embolic materials used in the management of visceral artery pseudoaneurysms is essential for successful and safe embolization. We review and illustrate the endovascular, percutaneous and endoscopic ultrasound techniques used in the treatment of visceral artery pseudoaneurysm and briefly discuss the embolic materials and their benefits and risks.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Management of hepatic artery aneurysm: A case series
Ashley Rosenberg, Katarzyna Trebska-McGowan, Trevor Reichman, Amit Sharma, Adrian Cotterell, Brian Strife, Aamir A. Khan, Vinay Kumaran, David A. Bruno, Marlon F. Levy, Chandra Shekhar Bhati
Ann Hepatobiliary Pancreat Surg. 2020;24(3):333-338. doi: 10.14701/ahbps.2020.24.3.333.
Reference
-
1. Belli AM, Markose G, Morgan R. The role of interventional radiology in the management of abdominal visceral artery aneurysms. Cardiovasc Intervent Radiol. 2012; 35:234–243.2. Gabelmann A, Görich J, Merkle EM. Endovascular treatment of visceral artery aneurysms. J Endovasc Ther. 2002; 9:38–47.3. Lu M, Weiss C, Fishman EK, Johnson PT, Verde F. Review of visceral aneurysms and pseudoaneurysms. J Comput Assist Tomogr. 2015; 39:1–6.4. Guillon R, Garcier JM, Abergel A, Mofid R, Garcia V, Chahid T, et al. Management of splenic artery aneurysms and false aneurysms with endovascular treatment in 12 patients. Cardiovasc Intervent Radiol. 2003; 26:256–260.5. Cordova AC, Sumpio BE. Visceral artery aneurysms and pseudoaneurysms--should they all be managed by endovascular techniques? Ann Vasc Dis. 2013; 6:687–693.6. Pasha SF, Gloviczki P, Stanson AW, Kamath PS. Splanchnic artery aneurysms. Mayo Clin Proc. 2007; 82:472–479.7. Bergert H, Hinterseher I, Kersting S, Leonhardt J, Bloomenthal A, Saeger HD. Management and outcome of hemorrhage due to arterial pseudoaneurysms in pancreatitis. Surgery. 2005; 137:323–328.8. Chadha M, Ahuja C. Visceral artery aneurysms: diagnosis and percutaneous management. Semin Intervent Radiol. 2009; 26:196–206.9. Keeling AN, McGrath FP, Lee MJ. Interventional radiology in the diagnosis, management, and follow-up of pseudoaneurysms. Cardiovasc Intervent Radiol. 2009; 32:2–18.10. Nosher JL, Chung J, Brevetti LS, Graham AM, Siegel RL. Visceral and renal artery aneurysms: a pictorial essay on endovascular therapy. Radiographics. 2006; 26:1687–1704. quiz 168711. Jesinger RA, Thoreson AA, Lamba R. Abdominal and pelvic aneurysms and pseudoaneurysms: imaging review with clinical, radiologic, and treatment correlation. Radiographics. 2013; 33:E71–E96.12. Madhusudhan KS, Sharma S, Seth A. Spontaneous closure of a traumatic intrarenal pseudoaneurysm. J Postgrad Med. 2009; 55:124–126.13. Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005; 25:Suppl 1. S173–S189.14. Loffroy R, Rao P, Ota S, De Lin M, Kwak BK, Krause D, et al. Packing technique for endovascular coil embolisation of peripheral arterial pseudo-aneurysms with preservation of the parent artery: safety, efficacy and outcomes. Eur J Vasc Endovasc Surg. 2010; 40:209–215.15. Fankhauser GT, Stone WM, Naidu SG, Oderich GS, Ricotta JJ, Bjarnason H, et al. The minimally invasive management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2011; 53:966–970.16. Julianov A, Georgiev Y. Hepatic artery aneurysm causing obstructive jaundice. Quant Imaging Med Surg. 2014; 4:294–295.17. Walker TG. Mesenteric vasculature and collateral pathways. Semin Intervent Radiol. 2009; 26:167–174.18. Yíldírím M, Celik HH, Yíldíz Z, Tatar I, Aldur MM. The middle colic artery originating from the coeliac trunk. Folia Morphol (Warsz). 2004; 63:363–365.19. Saad WE, Davies MG, Sahler L, Lee D, Patel N, Kitanosono T, et al. Arc of buhler: incidence and diameter in asymptomatic individuals. Vasc Endovascular Surg. 2005; 39:347–349.20. Shuaib W, Tiwana MH, Vijayasarathi A, Sadiq MF, Anderson S, Amin N, et al. Imaging of vascular pseudoaneurysms in the thorax and abdomen. Clin Imaging. 2015; 39:352–362.21. Dohan A, Dautry R, Guerrache Y, Fargeaudou Y, Boudiaf M, Le Dref O, et al. Three-dimensional MDCT angiography of splanchnic arteries: pearls and pitfalls. Diagn Interv Imaging. 2015; 96:187–200.22. Sueyoshi E, Sakamoto I, Nakashima K, Minami K, Hayashi K. Visceral and peripheral arterial pseudoaneurysms. AJR Am J Roentgenol. 2005; 185:741–749.23. Orth RC, Wallace MJ, Kuo MD. Technology Assessment Committee of the Society of Interventional Radiology. C-arm cone-beam CT: general principles and technical considerations for use in interventional radiology. J Vasc Interv Radiol. 2008; 19:814–820.24. Lauric A, Heller RS, Schimansky S, Malek AM. Benefit of cone-beam CT angiography in visualizing aneurysm shape and identification of exact rupture site. J Neuroimaging. 2015; 25:56–61.25. Saeed Kilani M, Haberlay M, Bergère A, Murphy C, Sobocinski J, Donati T, et al. 3D rotational angiography in the endovascular treatment of visceral aneurysms: preliminary experience in a single centre. Eur Radiol. 2016; 26:87–94.26. Patil VV, Fischman AM, Patel RS, Kim E, Lookstein RA, Tabori NE, et al. GI hemorrhage arising from splenic artery: intraprocedure cone-beam CT as problem-solving tool to aide in safe catheterization of offending vessel. Clin Imaging. 2015; 39:928–930.27. Loffroy R, Favelier S, Pottecher P, Genson PY, Estivalet L, Gehin S, et al. Endovascular management of visceral artery aneurysms: when to watch, when to intervene? World J Radiol. 2015; 7:143–148.28. Tétreau R, Beji H, Henry L, Valette PJ, Pilleul F. Arterial splanchnic aneurysms: presentation, treatment and outcome in 112 patients. Diagn Interv Imaging. 2016; 97:81–90.29. Leyon JJ, Littlehales T, Rangarajan B, Hoey ET, Ganeshan A. Endovascular embolization: review of currently available embolization agents. Curr Probl Diagn Radiol. 2014; 43:35–53.30. Vaidya S, Tozer KR, Chen J. An overview of embolic agents. Semin Intervent Radiol. 2008; 25:204–215.31. Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, et al. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007; 45:276–283. discussion 283.32. Barbiero G, Battistel M, Susac A, Miotto D. Percutaneous thrombin embolization of a pancreatico-duodenal artery pseudoaneurysm after failing of the endovascular treatment. World J Radiol. 2014; 6:629–635.33. Lubarsky M, Ray C, Funaki B. Embolization agents-which one should be used when? Part 2: small-vessel embolization. Semin Intervent Radiol. 2010; 27:99–104.34. Manian U, Badri H, Coyne P, Nice C, Ashour H, Bhattacharya V. Endovascular treatment of a ruptured splenic artery aneurysm using Amplatzer(®) vascular plug. Int J Biomed Sci. 2009; 5:81–84.35. Kessel D, Robertson I. Interventional radiology: a survival guide. 3rd ed. Philadelphia: Churchill Livingstone;2011.36. Koetser IC, de Vries EN, van Delden OM, Smorenburg SM, Boermeester MA, van Lienden KP. A checklist to improve patient safety in interventional radiology. Cardiovasc Intervent Radiol. 2013; 36:312–319.37. Dohan A, Eveno C, Dautry R, Guerrache Y, Camus M, Boudiaf M, et al. Role and effectiveness of percutaneous arterial embolization in hemodynamically unstable patients with ruptured splanchnic artery pseudoaneurysms. Cardiovasc Intervent Radiol. 2015; 38:862–870.38. Li L, Zhang Y, Chen Y, Zhu KS, Chen DJ, Zeng XQ, et al. A multicentre retrospective study of transcatheter angiographic embolization in the treatment of delayed haemorrhage after percutaneous nephrolithotomy. Eur Radiol. 2015; 25:1140–1147.39. Spiliopoulos S, Sabharwal T, Karnabatidis D, Brountzos E, Katsanos K, Krokidis M, et al. Endovascular treatment of visceral aneurysms and pseudoaneurysms: long-term outcomes from a multicenter European study. Cardiovasc Intervent Radiol. 2012; 35:1315–1325.40. Yasumoto T, Osuga K, Yamamoto H, Ono Y, Masada M, Mikami K, et al. Long-term outcomes of coil packing for visceral aneurysms: correlation between packing density and incidence of coil compaction or recanalization. J Vasc Interv Radiol. 2013; 24:1798–1807.41. Ikeda O, Nakasone Y, Tamura Y, Yamashita Y. Endovascular management of visceral artery pseudoaneurysms: transcatheter coil embolization using the isolation technique. Cardiovasc Intervent Radiol. 2010; 33:1128–1134.42. Song HH, Won YD, Kim YJ. Transcatheter N-butyl cyanoacrylate embolization of pseudoaneurysms. J Vasc Interv Radiol. 2010; 21:1508–1511.43. Madhusudhan KS, Gamanagatti S, Garg P, Shalimar , Dash NR, Pal S, et al. Endovascular embolization of visceral artery pseudoaneurysms using modified injection technique with N-butyl cyanoacrylate glue. J Vasc Interv Radiol. 2015; 26:1718–1725.44. Künzle S, Glenck M, Puippe G, Schadde E, Mayer D, Pfammatter T. Stent-graft repairs of visceral and renal artery aneurysms are effective and result in long-term patency. J Vasc Interv Radiol. 2013; 24:989–996.45. Kulkarni CB, Moorthy S, Pullara SK, Kannan RR. Endovascular treatment of aneurysm of splenic artery arising from splenomesentric trunk using stent graft. Korean J Radiol. 2013; 14:931–934.46. Sfyroeras GS, Dalainas I, Giannakopoulos TG, Antonopoulos K, Kakisis JD, Liapis CD. Flow-diverting stents for the treatment of arterial aneurysms. J Vasc Surg. 2012; 56:839–846.47. Amenta PS, Starke RM, Jabbour PM, Tjoumakaris SI, Gonzalez LF, Rosenwasser RH, et al. Successful treatment of a traumatic carotid pseudoaneurysm with the Pipeline stent: case report and review of the literature. Surg Neurol Int. 2012; 3:160.48. Hardman RL, Taussky P, Kim R, O'Hara RG. Post-transplant hepatic artery pseudoaneurysm treated with the pipeline flow-diverting stent. Cardiovasc Intervent Radiol. 2015; 38:1043–1046.49. Roberts KJ, Jones RG, Forde C, Marudanayagam R. Endoscopic ultrasound-guided treatment of visceral artery pseudoaneurysm. HPB (Oxford). 2012; 14:489–490.50. Gamanagatti S, Thingujam U, Garg P, Nongthombam S, Dash NR. Endoscopic ultrasound guided thrombin injection of angiographically occult pancreatitis associated visceral artery pseudoaneurysms: case series. World J Gastrointest Endosc. 2015; 7:1107–1113.51. Bilbao JI, Martínez-Cuesta A, Urtasun F, Cosín O. Complications of embolization. Semin Intervent Radiol. 2006; 23:126–142.52. Tsetis D. Endovascular treatment of complications of femoral arterial access. Cardiovasc Intervent Radiol. 2010; 33:457–468.53. Deuling JH, Vermeulen RP, Anthonio RA, van den, Jaarsma T, Jessurun G, et al. Closure of the femoral artery after cardiac catheterization: a comparison of Angio-Seal, StarClose, and manual compression. Catheter Cardiovasc Interv. 2008; 71:518–523.54. Yap FY, Omene BO, Patel MN, Yohannan T, Minocha J, Knuttinen MG, et al. Transcatheter embolotherapy for gastrointestinal bleeding: a single center review of safety, efficacy, and clinical outcomes. Dig Dis Sci. 2013; 58:1976–1984.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Thrombin Injection for a Pulmonary Artery Pseudoaneurysm: Case Report
- Update on Transradial Access for Percutaneous Transcatheter Visceral Artery Embolization
- Endovascular Management of Thenar-Hypothenar Aneurysms: Two Case Reports and Review of Literature
- Role of interventional radiology in the management of postoperative gastrointestinal leakage
- Interventional management for postoperative arterial bleeding in gastrointestinal surgery