Blood Res.
2019 Jun;54(2):120-124. 10.5045/br.2019.54.2.120.
Determining the risk factors associated with the development of Clostridium difficile infection in patients with hematological diseases
- Affiliations
-
- 1Department of Hematology and Oncology, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico. chrisbourlon@hotmail.com
- 2Department of Infectology, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico.
- 3Departament of Hospital Epidemiology and Quality Control of Medical Care, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico.
- KMID: 2451012
- DOI: http://doi.org/10.5045/br.2019.54.2.120
Abstract
- BACKGROUND
Clostridium difficile infection (CDI) is a nosocomial condition prevalent in patients with hematological disorders. We aimed to identify the risk factors associated with the development of CDI and assess the mortality rate at 15 and 30 days among hematologic patients admitted to a tertiary care center.
METHODS
We conducted a retrospective case-control study from January 2010 to December 2015. Forty-two patients with hematologic malignancy and CDI, and 84 with hematologic disease and without history of CDI were included in the case and control groups, respectively.
RESULTS
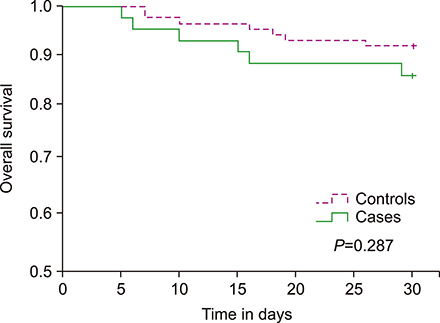
Univariate analysis revealed that episodes of febrile eutropenia [odds ratio (OR), 5.5; 95% confidence interval (CI), 2.3-12.9; P<0.001], admission to intensive care unit (OR, 3.8; 95% CI, 1.4-10.2; P=0.009), gastrointestinal surgery (OR, 1.2; 95% CI, 1.1-1.4; P<0.001), use of therapeutic (OR, 6.4; 95% CI, 2.5-15.9; P<0.001) and prophylactic antibiotics (OR, 4.2; 95% CI, 1.6-10.7; P=0.003) in the last 3 months, and >1 hospitalization (OR, 5.6; 95% CI, 2.5-12.6; P<0.001) were significant risk factors. Multivariate analysis showed that use of therapeutic antibiotics in the last 3 months (OR, 6.3; 95% CI, 2.1-18.8; P=0.001) and >1 hospitalization (OR, 4.3; 95% CI, 1.7-11.0; P=0.002) were independent risk factors. Three (7.1%) and 6 (14.2%) case patients died at 15 and 30 days, respectively.
CONCLUSION
The risk factors for developing CDI were exposure to therapeutic antibiotics and previous hospitalization. Hematological patients who developed CDI had higher early mortality rates, suggesting that new approaches for prevention and treatment are needed.
MeSH Terms
Figure
Reference
-
1. Martin JS, Monaghan TM, Wilcox MH. Clostridium difficile infection: epidemiology, diagnosis and understanding transmission. Nat Rev Gastroenterol Hepatol. 2016; 13:206–216.
Article2. Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013; 108:478–498.
Article3. Khan FY, Elzouki AN. Clostridium difficile infection: a review of the literature. Asian Pac J Trop Med. 2014; 7S1:S6–S13.
Article4. Kachrimanidou M, Malisiovas N. Clostridium difficile infection: a comprehensive review. Crit Rev Microbiol. 2011; 37:178–187.5. Lopardo G, Morfin-Otero R, Moran-Vazquez II, et al. Epidemiology of Clostridium difficile: a hospital-based descriptive study in Argentina and Mexico. Braz J Infect Dis. 2015; 19:8–14.
Article6. Dávila LP, Garza-González E, Rodríguez-Zulueta P, et al. Increasing rates of Clostridium difficile infection in Mexican hospitals. Braz J Infect Dis. 2017; 21:530–534.
Article7. Dupont HL. Diagnosis and management of Clostridium difficile infection. Clin Gastroenterol Hepatol. 2013; 11:1216–1223.
Article8. Dubberke ER, Reske KA, Yan Y, Olsen MA, McDonald LC, Fraser VJ. Clostridium difficile--associated disease in a setting of endemicity: identification of novel risk factors. Clin Infect Dis. 2007; 45:1543–1549.
Article9. Camacho-Ortiz A, Galindo-Fraga A, Rancel-Cordero A, et al. Factors associated with Clostridium difficile disease in a tertiary-care medical institution in Mexico: a case-control study. Rev Invest Clin. 2009; 61:371–377.10. Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31:431–455.
Article11. Anand A, Glatt AE. Clostridium difficile infection associated with antineoplastic chemotherapy: a review. Clin Infect Dis. 1993; 17:109–113.
Article12. Peretz A, Shlomo IB, Nitzan O, Bonavina L, Schaffer PM, Schaffer M. Clostridium difficile infection: associations with chemotherapy, radiation therapy, and targeting therapy treatments. Curr Med Chem. 2016; 23:4442–4449.
Article13. Gu SL, Chen YB, Lv T, et al. Risk factors, outcomes and epidemiology associated with Clostridium difficile infection in patients with haematological malignancies in a tertiary care hospital in China. J Med Microbiol. 2015; 64:209–216.
Article14. Gweon TG, Choi MG, Baeg MK, et al. Hematologic diseases: high risk of Clostridium difficile associated diarrhea. World J Gastroenterol. 2014; 20:6602–6607.
Article15. Selvey LA, Slimings C, Joske DJ, Riley TV. Clostridium difficile infections amongst patients with haematological malignancies: A data linkage study. PLoS One. 2016; 11:e0157839.
Article16. Parmar SR, Bhatt V, Yang J, Zhang Q, Schuster M. A retrospective review of metronidazole and vancomycin in the management of Clostridium difficile infection in patients with hematologic malignancies. J Oncol Pharm Pract. 2014; 20:172–182.
Article17. Altclas J, Requejo A, Jaimovich G, Milovic V, Feldman L. Clostridium difficile infection in patients with neutropenia. Clin Infect Dis. 2002; 34:723.
Article18. Schalk E, Bohr UR, König B, Scheinpflug K, Mohren M. Clostridium difficile-associated diarrhoea, a frequent complication in patients with acute myeloid leukaemia. Ann Hematol. 2010; 89:9–14.
Article19. Spadão F, Gerhardt J, Guimarães T, et al. Incidence of diarrhea by Clostridium difficile in hematologic patients and hematopoietic stem cell transplantation patients: risk factors for severe forms and death. Rev Inst Med Trop Sao Paulo. 2014; 56:325–331.
Article20. Swerdlow SH, Campo E, Harris NL, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th ed. Lyon, France: IARC Press;2017.21. National Institutes of Health. Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. Bethesda, MD: National Institutes of Health;2017. Accessed September 18, 2018. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf.22. Shane AL, Mody RK, Crump JA, et al. 2017 infectious diseases society of america clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017; 65:e45–e80.
Article23. Eckert C, Said O, Rambaud C, et al. Comparison of the VIDAS® C. difficile GDH and the GDH component of the C. diff Quik Chek Complete for detection of Clostridium difficile in stools. ECCMID (Annual Congress Abstracts). 2013; eP187.24. CM0601. Clostridium difficile agar base. Basingstoke, UK: Thermo Fisher Scientific Inc;2013. Accessed September 18, 2018. http://www.oxoid.com/UK/blue/prod_detail/prod_detail.asp?pr=CM0601&org=52&c=UK&lang=EN.25. Xpert® C. difficile/Epi. 45-minute detection & differentiation of clostridium difficile & the Epidemic 027 strain. Sunnyvale, CA: Cepheid;2018. Accessed September 18, 2018. http://www.cepheid.com/us/cepheid-solutions/clinical-ivd-tests/healthcare-associated-infections/xpert-c-difficile-epi.26. Gorschlüter M, Glasmacher A, Hahn C, et al. Clostridium difficile infection in patients with neutropenia. Clin Infect Dis. 2001; 33:786–791.
Article27. Clabots CR, Johnson S, Olson MM, Peterson LR, Gerding DN. Acquisition of Clostridium difficile by hospitalized patients: evidence for colonized new admissions as a source of infection. J Infect Dis. 1992; 166:561–567.
Article28. Apostolopoulou E, Raftopoulos V, Terzis K, Elefsiniotis I. Infection Probability Score: a predictor of Clostridium difficile-associated disease onset in patients with haematological malignancy. Eur J Oncol Nurs. 2011; 15:404–409.
Article29. Fuereder T, Koni D, Gleiss A, et al. Risk factors for Clostridium difficile infection in hemato-oncological patients: A case control study in 144 patients. Sci Rep. 2016; 6:31498.
Article30. Yoon YK, Kim MJ, Sohn JW, et al. Predictors of mortality attributable to Clostridium difficile infection in patients with underlying malignancy. Support Care Cancer. 2014; 22:2039–2048.
Article31. McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018; 66:e1–e48.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clostridium difficile Infection: What's New?
- Clostridium difficile Infection at Diagnosis and during the Disease Course of Pediatric Inflammatory Bowel Disease
- Clostridium difficile in Children: To Treat or Not to Treat?
- New Treatment Option for Recurrent Clostridium difficile Infection
- A Case of Reactive Arthritis in a Patient with Clostridium Difficile Diarrhea