Acute Crit Care.
2019 Feb;34(1):86-91. 10.4266/acc.2016.00794.
Cardiac Arrest from Patient Position Change after Spine Surgery on a Jackson Table
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chungnam National University College of Medicine, Daejeon, Korea. seohwy@cnu.ac.kr
- KMID: 2449385
- DOI: http://doi.org/10.4266/acc.2016.00794
Abstract
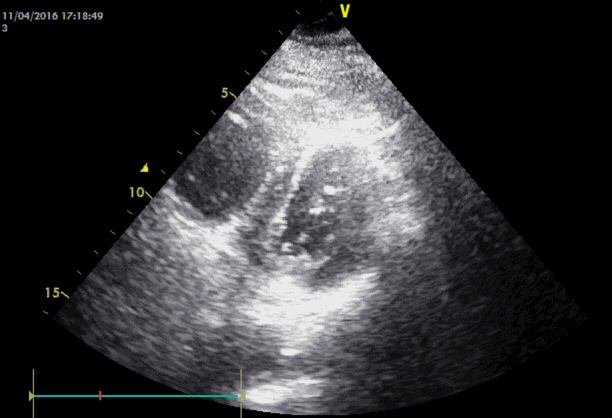
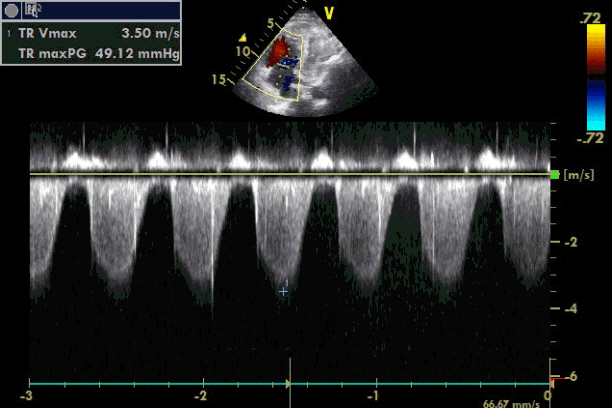
- The Jackson table has minimal effects on cardiac function because it does not elevate abdominal and thoracic pressures. In addition, it decreases venous congestion and increases exposure of the surgical field. However, the hips and knees are flexed with inappropriate padding, and venostasis is promoted and increased. Pulmonary thromboembolism (PTE) is fatal; thus immediate diagnosis and treatment are essential. However, clinical signs of intraoperative PTE are difficult to discern. Thrombolytic therapy can be considered as first-line therapy, but bleeding limits its use. The authors report a case of PTE resulting from patient positional change after spine surgery, and the use of immediate postoperative recombinant tissue-type plasminogen activator.
MeSH Terms
Figure
Reference
-
1. Wood KE. Major pulmonary embolism: review of a pathophysiologic approach to the golden hour of hemodynamically significant pulmonary embolism. Chest. 2002; 121:877–905.2. Schizas C, Neumayer F, Kosmopoulos V. Incidence and management of pulmonary embolism following spinal surgery occurring while under chemical thromboprophylaxis. Eur Spine J. 2008; 17:970–4.
Article3. Kanter DS, Mikkola KM, Patel SR, Parker JA, Goldhaber SZ. Thrombolytic therapy for pulmonary embolism: frequency of intracranial hemorrhage and associated risk factors. Chest. 1997; 111:1241–5.4. Nicol M, Sun Y, Craig N, Wardlaw D. Incidence of thromboembolic complications in lumbar spinal surgery in 1,111 patients. Eur Spine J. 2009; 18:1548–52.
Article5. Tominaga H, Setoguchi T, Tanabe F, Kawamura I, Tsuneyoshi Y, Kawabata N, et al. Risk factors for venous thromboembolism after spine surgery. Medicine (Baltimore). 2015; 94:e466.
Article6. Takahashi H, Yokoyama Y, Iida Y, Terashima F, Hasegawa K, Saito T, et al. Incidence of venous thromboembolism after spine surgery. J Orthop Sci. 2012; 17:114–7.
Article7. Hohl JB, Lee JY, Rayappa SP, Nabb CE, Devin CJ, Kang JD, et al. Prevalence of venous thromboembolic events after elective major thoracolumbar degenerative spine surgery. J Spinal Disord Tech. 2015; 28:E310–5.
Article8. Bohl DD, Webb ML, Lukasiewicz AM, Samuel AM, Basques BA, Ahn J, et al. Timing of complications after spinal fusion surgery. Spine (Phila Pa 1976). 2015; 40:1527–35.
Article9. Jang IS, Kim HT, An SK, Kwon YE, Lee JH. Pulmonary thromboembolism occurred immediately after leg elevation under induction of general anesthesia in a patient with femur fracture: a case report. Anesth Pain Med. 2009; 4:129–32.10. Song JE, Chun DH, Shin JH, Park C, Lee JY. Pulmonary thromboembolism after tourniquet inflation under spinal anesthesia: a case report. Korean J Anesthesiol. 2010; 59(Suppl):S82–5.
Article11. Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014; 35:3033–69.12. Dharmavaram S, Jellish WS, Nockels RP, Shea J, Mehmood R, Ghanayem A, et al. Effect of prone positioning systems on hemodynamic and cardiac function during lumbar spine surgery: an echocardiographic study. Spine (Phila Pa 1976). 2006; 31:1388–93.
Article13. Takahashi S, Kitagawa H, Ishii T. Intraoperative pulmonary embolism during spinal instrumentation surgery. A prospective study using transoesophageal echocardiography. J Bone Joint Surf Br. 2003; 85:90–4.14. Steinestel K, Geiger A, Naraghi R, Kunz U, Danz B, Kraft K, et al. Fatal thromboembolism to the left pulmonary artery by locally applied hemostatic matrix after surgical removal of spinal schwannoma: a case report. Hum Pathol. 2013; 44:294–8.
Article15. Schaefer-Prokop C, Prokop M. MDCT for the diagnosis of acute pulmonary embolism. Eur Radiol. 2005; 15 Suppl 4:D37–41.
Article16. Vieillard-Baron A, Qanadli SD, Antakly Y, Fourme T, Loubières Y, Jardin F, et al. Transesophageal echocardiography for the diagnosis of pulmonary embolism with acute cor pulmonale: a comparison with radiological procedures. Intensive Care Med. 1998; 24:429–33.
Article17. Kucher N, Goldhaber SZ. Cardiac biomarkers for risk stratification of patients with acute pulmonary embolism. Circulation. 2003; 108:2191–4.
Article18. Daniels LB, Parker JA, Patel SR, Grodstein F, Goldhaber SZ. Relation of duration of symptoms with response to thrombolytic therapy in pulmonary embolism. Am J Cardiol. 1997; 80:184–8.
Article19. Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e326S–e350S.20. Darvish-Kazem S, Gandhi M, Marcucci M, Douketis JD. Perioperative management of antiplatelet therapy in patients with a coronary stent who need noncardiac surgery: a systematic review of clinical practice guidelines. Chest. 2013; 144:1848–56.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiovascular Effects of Free Movement of Abdominal Muscle in Prone Positioning during General Anesthesia
- Percutaneous cardiopulmonary support for the management of recurrent cardiac arrest during scoliosis correction surgery in the prone position: A case report
- Cardiac arrest after position change in a morbidly obese patient: A case report
- Sudden hemodynamic collapse after prone positioning on a Jackson spinal table for spinal surgery
- The effect on respiratory mechanics when using a Jackson surgical table in the prone position during spinal surgery