Acute Crit Care.
2019 Feb;34(1):60-70. 10.4266/acc.2018.00311.
Protecting Postextubation Respiratory Failure and Reintubation by High-Flow Nasal Cannula Compared to Low-Flow Oxygen System: Single Center Retrospective Study and Literature Review
- Affiliations
-
- 1Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Konyang University Hospital, Daejeon, Korea. sjoongkwon@hanmail.net
- 2The 2nd Infantry Division of Republic of Korea Army, Yanggu, Korea.
- KMID: 2449381
- DOI: http://doi.org/10.4266/acc.2018.00311
Abstract
- BACKGROUND
Use of a high-flow nasal cannula (HFNC) reduced postextubation respiratory failure (PERF) and reintubation rate compared to use of a low-flow oxygen system (LFOS) in low-risk patients. However, no obvious conclusion was reached for high-risk patients. Here, we sought to present the current status of HFNC use as adjunctive oxygen therapy in a clinical setting and to elucidate the nature of the protective effect following extubation.
METHODS
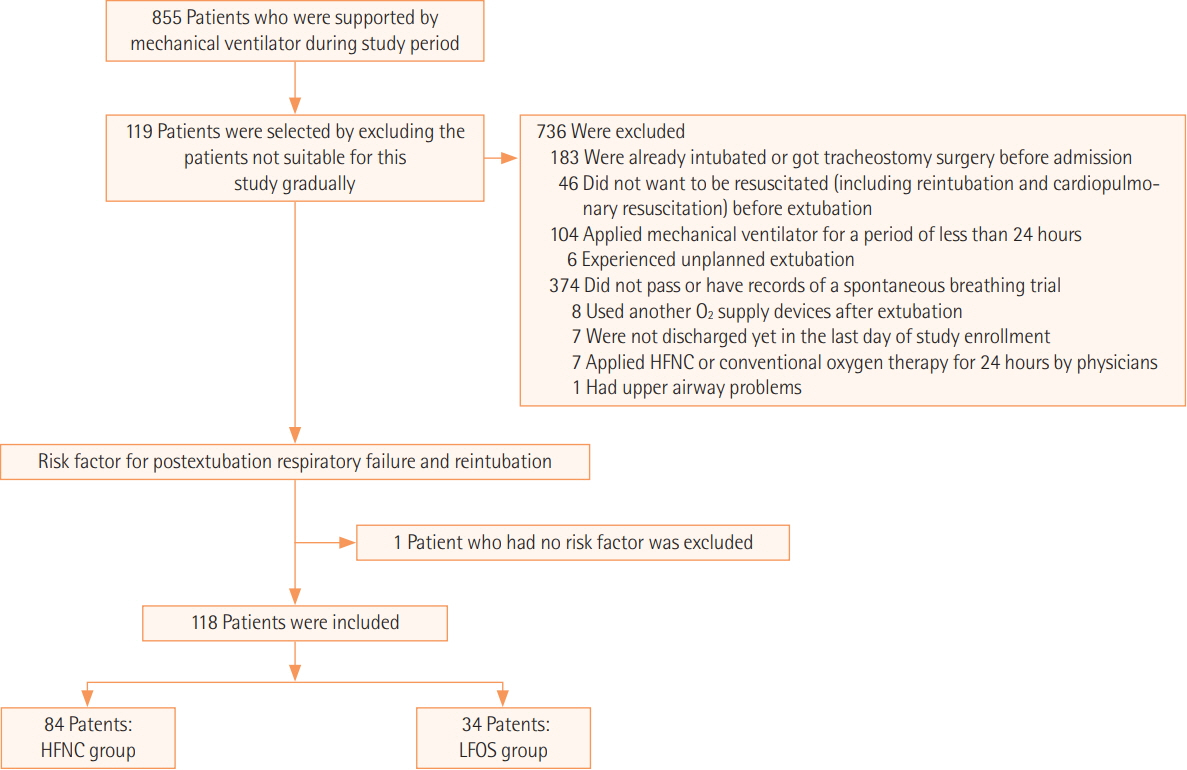
The medical records of 855 patients who were admitted to the intensive care unit of single university hospital during a period of 5.5 years were analyzed retrospectively, with only 118 patients ultimately included in the present research. The baseline characteristics of these patients and the occurrence of PERF and reintubation along with physiologic changes were analyzed.
RESULTS
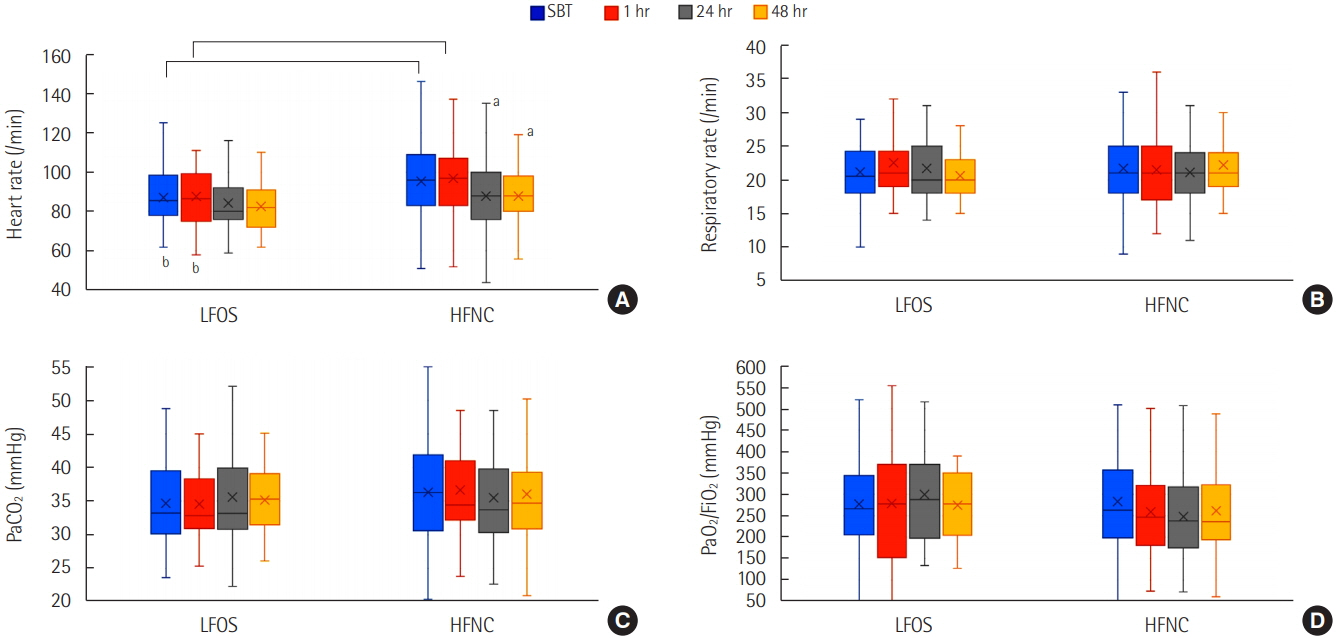
Eighty-four patients underwent HFNC, and the remaining 34 patients underwent conventional LFOS after extubation. Physicians preferred HFNC to LFOS in the face of high-risk features including old age, neurologic disease, moderate to severe chronic obstructive pulmonary disease, a long duration of mechanical ventilation, low baseline arterial partial pressure of oxygen to fraction of inspired oxygen ratio, and a high baseline alveolar-arterial oxygen difference. The reintubation rate at 72 hours after extubation was not different (9.5% vs. 8.8%; P=1.000). Hypoxic respiratory failure was slightly higher in the nonreintubation group than in the reintubation group (31.9% vs. 6.7%; P=0.058). Regarding physiologic effects, heart rate was only stabilized after 24 hours of extubation in the HFNC group.
CONCLUSIONS
No difference was found in the occurrence of PERF and reintubation between both groups. It is worth noting that similar PERF and reintubation ratios were shown in the HFNC group in those with certain exacerbating risk factors versus not. Caution is needed regarding delayed reintubation in the HFNC group.
MeSH Terms
Figure
Reference
-
1. Epstein SK. Decision to extubate. Intensive Care Med. 2002; 28:535–46.
Article2. Nava S, Gregoretti C, Fanfulla F, Squadrone E, Grassi M, Carlucci A, et al. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med. 2005; 33:2465–70.
Article3. Maggiore SM, Idone FA, Vaschetto R, Festa R, Cataldo A, Antonicelli F, et al. Nasal high-flow versus venturi mask oxygen therapy after extubation: effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med. 2014; 190:282–8.
Article4. Hernández G, Vaquero C, González P, Subira C, Frutos-Vivar F, Rialp G, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in lowrisk patients: a randomized clinical trial. JAMA. 2016; 315:1354–61.5. Yoo JW, Synn A, Huh JW, Hong SB, Koh Y, Lim CM. Clinical efficacy of high-flow nasal cannula compared to noninvasive ventilation in patients with post-extubation respiratory failure. Korean J Intern Med. 2016; 31:82–8.
Article6. Hernández G, Vaquero C, Colinas L, Cuena R, González P, Canabal A, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016; 316:1565–74.7. Ornico SR, Lobo SM, Sanches HS, Deberaldini M, Tófoli LT, Vidal AM, et al. Noninvasive ventilation immediately after extubation improves weaning outcome after acute respiratory failure: a randomized controlled trial. Crit Care. 2013; 17:R39.
Article8. Carron M, Freo U, BaHammam AS, Dellweg D, Guarracino F, Cosentini R, et al. Complications of non-invasive ventilation techniques: a comprehensive qualitative review of randomized trials. Br J Anaesth. 2013; 110:896–914.
Article9. Nishimura M. High-flow nasal cannula oxygen therapy in adults. J Intensive Care. 2015; 3:15.
Article10. Fricke K, Tatkov S, Domanski U, Franke KJ, Nilius G, Schneider H. Nasal high flow reduces hypercapnia by clearance of anatomical dead space in a COPD patient. Respir Med Case Rep. 2016; 19:115–7.
Article11. Frizzola M, Miller TL, Rodriguez ME, Zhu Y, Rojas J, Hesek A, et al. High-flow nasal cannula: impact on oxygenation and ventilation in an acute lung injury model. Pediatr Pulmonol. 2011; 46:67–74.
Article12. Fernandez R, Subira C, Frutos-Vivar F, Rialp G, Laborda C, Masclans JR, et al. High-flow nasal cannula to prevent postextubation respiratory failure in high-risk non-hypercapnic patients: a randomized multicenter trial. Ann Intensive Care. 2017; 7:47.
Article13. Futier E, Paugam-Burtz C, Godet T, Khoy-Ear L, Rozencwajg S, Delay JM, et al. Effect of early postextubation high-flow nasal cannula vs conventional oxygen therapy on hypoxaemia in patients after major abdominal surgery: a French multicentre randomised controlled trial (OPERA). Intensive Care Med. 2016; 42:1888–98.
Article14. Yu Y, Qian X, Liu C, Zhu C. Effect of high-flow nasal cannula versus conventional oxygen therapy for patients with thoracoscopic lobectomy after extubation. Can Respir J. 2017; 2017:7894631.
Article15. Song HZ, Gu JX, Xiu HQ, Cui W, Zhang GS. The value of highflow nasal cannula oxygen therapy after extubation in patients with acute respiratory failure. Clinics. 2017; 72:562–7.
Article16. Dhillon NK, Smith EJT, Ko A, Harada MY, Polevoi D, Liang R, et al. Extubation to high-flow nasal cannula in critically ill surgical patients. J Surg Res. 2017; 217:258–64.
Article17. Huang HW, Sun XM, Shi ZH, Chen GQ, Chen L, Friedrich JO, et al. Effect of high-flow nasal cannula oxygen therapy versus conventional oxygen therapy and noninvasive ventilation on reintubation rate in adult patients after extubation: a systematic review and meta-analysis of randomized controlled trials. J Intensive Care Med. 2018; 33:609–23.
Article18. Ni YN, Luo J, Yu H, Liu D, Liang BM, Yao R, et al. Can high-flow nasal cannula reduce the rate of reintubation in adult patients after extubation? A meta-analysis. BMC Pulm Med. 2017; 17:142.
Article19. Vallverdú I, Calaf N, Subirana M, Net A, Benito S, Mancebo J. Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med. 1998; 158:1855–62.
Article20. Lee KH, Hui KP, Chan TB, Tan WC, Lim TK. Rapid shallow breathing (frequency-tidal volume ratio) did not predict extubation outcome. Chest. 1994; 105:540–3.
Article21. Rittayamai N, Tscheikuna J, Rujiwit P. High-flow nasal cannula versus conventional oxygen therapy after endotracheal extubation: a randomized crossover physiologic study. Respir Care. 2014; 59:485–90.
Article22. Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015; 372:2185–96.
Article23. Jeong ES, Lee K. Clinical application of modified burns wean assessment program scores at first spontaneous breathing trial in weaning patients from mechanical ventilation. Acute Crit Care. 2018; 33:260–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study on the Changes of SaO2, According to the Different Type of Oxygen Suppliers
- Factors about Failure after High Flow Oxygen through Nasal Cannula Therapy in Hypoxic Respiratory Failure Patients at Emergency Department Presentation
- High-flow nasal cannula for respiratory failure in adult patients
- High-flow nasal cannula oxygen therapy in children: a clinical review
- Treatment of acute respiratory failure: high-flow nasal cannula