Ann Rehabil Med.
2019 Apr;43(2):178-186. 10.5535/arm.2019.43.2.178.
Scapular Upward Rotation During Passive Humeral Abduction in Individuals With Hemiplegia Post-stroke
- Affiliations
-
- 1Department of Physical Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand. jonjin.r@cmu.ac.th
- 2Department of Physical Therapy, California State University, Northridge, CA, USA.
- KMID: 2449000
- DOI: http://doi.org/10.5535/arm.2019.43.2.178
Abstract
OBJECTIVE
To describe scapular upward rotation during passive humeral abduction in individuals with hemiplegia post-stroke compared to normal subjects.
METHODS
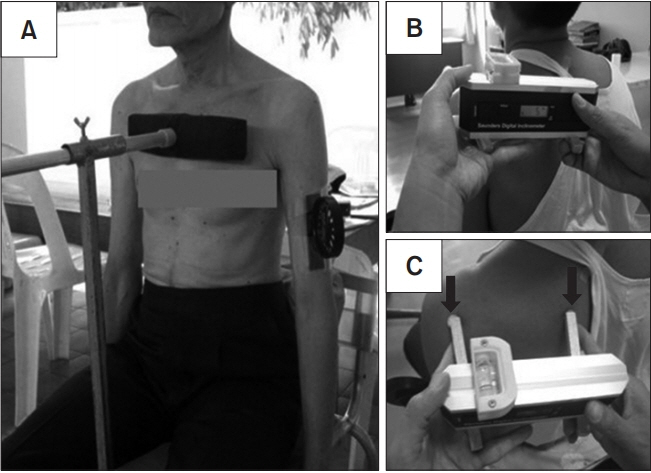
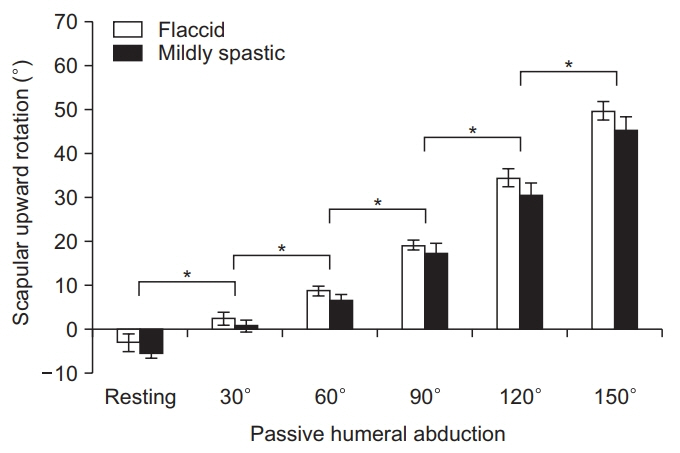
Twenty-five individuals with hemiplegia post-stroke and 25 age- and gender-matched normal subjects voluntarily participated in this study. Scapular upward rotation during resting and passive humeral abduction at 30°, 60°, 90°, 120°, and 150° were measured using a digital inclinometer.
RESULTS
In both groups, scapular upward rotation significantly increased as humeral abduction increased (p<0.001). Scapular upward rotation was significantly less in the hemiplegic group compared to that in the control at 90° (p=0.002), 120° (p<0.001), and 150° of humeral abduction (p<0.001). The mean difference in scapular upward rotation between these two groups ranged from 6.3° to 11.38°.
CONCLUSION
Passive humeral abductions ranging from 90° to 150° can significantly alter scapular upward rotation in individuals with hemiplegia post-stroke compared to those of matched normal subjects. The magnitude of reduction of the scapular upward rotation may potentially lead to the development of hemiplegic shoulder pain after prolonged repetitive passive movement. Scapular upward rotation should be incorporated during passive humeral abduction in individuals with hemiplegia post-stroke, especially when the humeral is moved beyond 90° of humeral abduction. Combined movements of scapular and humeral will help maintain the relative movement between the scapula and humerus. However, further longitudinal study in patients with shoulder pain post-stroke is needed to confirm these findings.
Keyword
MeSH Terms
Figure
Reference
-
1. Snels IA, Dekker JH, van der Lee JH, Lankhorst GJ, Beckerman H, Bouter LM. Treating patients with hemiplegic shoulder pain. Am J Phys Med Rehabil. 2002; 81:150–60.
Article2. Lo SF, Chen SY, Lin HC, Jim YF, Meng NH, Kao MJ. Arthrographic and clinical findings in patients with hemiplegic shoulder pain. Arch Phys Med Rehabil. 2003; 84:1786–91.3. Roy CW, Sands MR, Hill LD. Shoulder pain in acutely admitted hemiplegics. Clin Rehabil. 1994; 8:334–40.
Article4. Wanklyn P, Forster A, Young J. Hemiplegic shoulder pain (HSP): natural history and investigation of associated features. Disabil Rehabil. 1996; 18:497–501.
Article5. Roy CW, Sands MR, Hill LD, Harrison A, Marshall S. The effect of shoulder pain on outcome of acute hemiplegia. Clin Rehabil. 1995; 9:21–7.
Article6. Blennerhassett JM, Gyngell K, Crean R. Reduced active control and passive range at the shoulder increase risk of shoulder pain during inpatient rehabilitation post-stroke: an observational study. J Physiother. 2010; 56:195–9.
Article7. Karaahmet OZ, Eksioglu E, Gurcay E, Karsli PB, Tamkan U, Bal A, et al. Hemiplegic shoulder pain: associated factors and rehabilitation outcomes of hemiplegic patients with and without shoulder pain. Top Stroke Rehabil. 2014; 21:237–45.8. Lindgren I, Lexell J, Jonsson AC, Brogardh C. Leftsided hemiparesis, pain frequency, and decreased passive shoulder range of abduction are predictors of long-lasting poststroke shoulder pain. PM R. 2012; 4:561–8.
Article9. Bender L, McKenna K. Hemiplegic shoulder pain: defining the problem and its management. Disabil Rehabil. 2001; 23:698–705.10. Lynch D, Ferraro M, Krol J, Trudell CM, Christos P, Volpe BT. Continuous passive motion improves shoulder joint integrity following stroke. Clin Rehabil. 2005; 19:594–9.
Article11. Tseng CN, Chen CC, Wu SC, Lin LC. Effects of a range-of-motion exercise programme. J Adv Nurs. 2007; 57:181–91.
Article12. Tyson SF, Chissim C. The immediate effect of handling technique on range of movement in the hemiplegic shoulder. Clin Rehabil. 2002; 16:137–40.
Article13. Hardwick DD, Lang CE. Scapular and humeral movement patterns of people with stroke during range-ofmotion exercises. J Neurol Phys Ther. 2011; 35:18–25.
Article14. Stefko JM, Tibone JE, Cawley PW, ElAttrache NE, McMahon PJ. Strain of the anterior band of the inferior glenohumeral ligament during capsule failure. J Shoulder Elbow Surg. 1997; 6:473–9.
Article15. Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St. Louis: Mosby;2002.16. Ebaugh DD, McClure PW, Karduna AR. Three-dimensional scapulothoracic motion during active and passive arm elevation. Clin Biomech (Bristol, Avon). 2005; 20:700–9.
Article17. McQuade KJ, Smidt GL. Dynamic scapulohumeral rhythm: the effects of external resistance during elevation of the arm in the scapular plane. J Orthop Sports Phys Ther. 1998; 27:125–33.
Article18. Price CI, Franklin P, Rodgers H, Curless RH, Johnson GR. Active and passive scapulohumeral movement in healthy persons: a comparison. Arch Phys Med Rehabil. 2000; 81:28–31.
Article19. Karduna AR, McClure PW, Michener LA. Scapular kinematics: effects of altering the Euler angle sequence of rotations. J Biomech. 2000; 33:1063–8.
Article20. Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009; 39:90–104.
Article21. Culham E, Peat M. Functional anatomy of the shoulder complex. J Orthop Sports Phys Ther. 1993; 18:342–50.
Article22. Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999; 80:945–50.
Article23. Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001; 31:81–9.
Article24. Scibek JS, Carcia CR. Assessment of scapulohumeral rhythm for scapular plane shoulder elevation using a modified digital inclinometer. World J Orthop. 2012; 3:87–94.
Article25. Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. Upper Saddle River: Pearson;2009.26. Flatow EL, Soslowsky LJ, Ticker JB, Pawluk RJ, Hepler M, Ark J, et al. Excursion of the rotator cuff under the acromion: patterns of subacromial contact. Am J Sports Med. 1994; 22:779–88.27. Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon). 2003; 18:369–79.
Article28. Petersson CJ, Redlund-Johnell I. The subacromial space in normal shoulder radiographs. Acta Orthop Scand. 1984; 55:57–8.
Article29. Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000; 80:276–91.
Article30. Warner JJ, Deng XH, Warren RF, Torzilli PA. Static capsuloligamentous restraints to superior-inferior translation of the glenohumeral joint. Am J Sports Med. 1992; 20:675–85.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Abduction Motion Analysis of Hemiplegic Shoulders with a Fluoroscopic Guide
- Measurement of the Shoulder Motion Using 3-D Motion Capture Technique
- Comparison of In Vivo Three-Dimensional Glenohumeral Positions and Scapular Kinematics between Young and Older Male Groups
- Biomechanical investigation of arm position on deforming muscular forces in proximal humerus fractures
- Three-Dimensional Scapular Kinematics in Patients with Reverse Total Shoulder Arthroplasty during Arm Motion