Ann Hepatobiliary Pancreat Surg.
2019 May;23(2):183-186. 10.14701/ahbps.2019.23.2.183.
Wedged-patch venoplasty of the left liver graft portal vein for size matching in pediatric living donor liver transplantation
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2448774
- DOI: http://doi.org/10.14701/ahbps.2019.23.2.183
Abstract
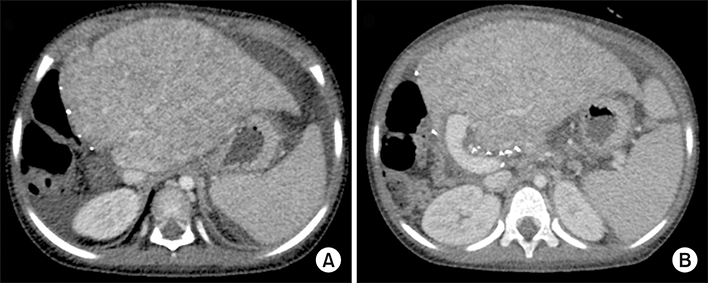
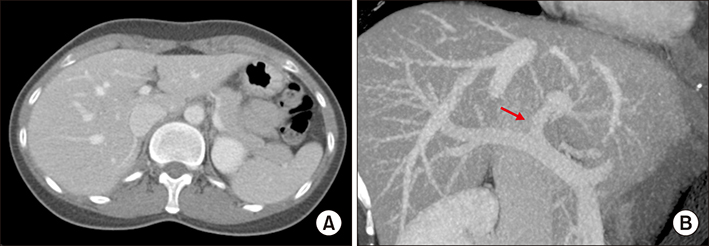
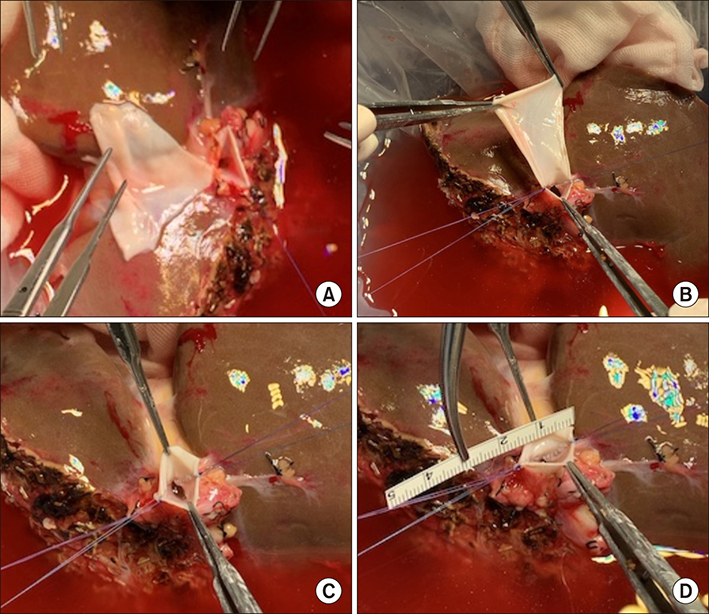
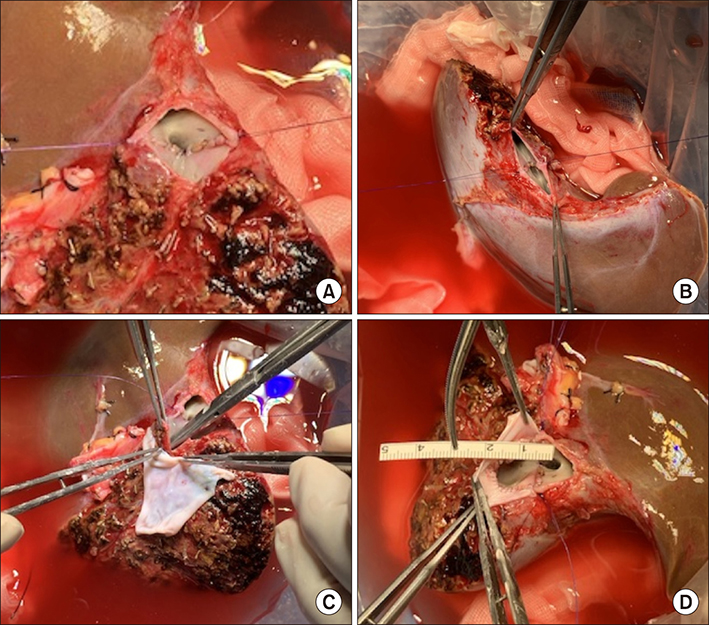
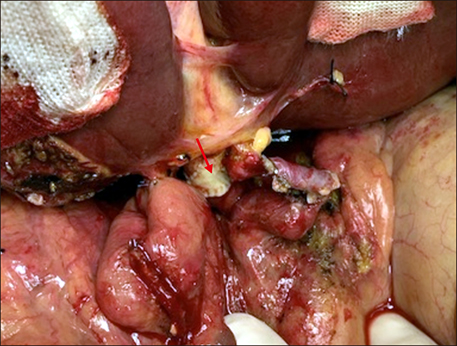
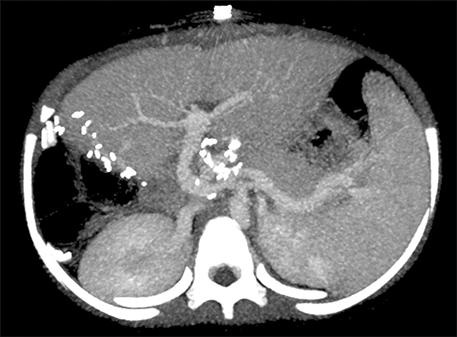
- Portal vein (PV) size matching between recipient and liver graft is important in preventing anastomotic stenosis in living donor liver transplantation (LDLT). In right liver grafts, the diameter of graft PV is usually >10 mm. Thus, PV size matching does not become critical in adult recipients. If the recipient PV is very large, funneling fence can be attached to graft PV. However, if the diameter of graft PV is <8 mm, it can induce anastomotic stenosis. We experienced a few cases of PV anastomotic stenosis due to small-sized graft PV in >5000 LDLT cases, but graft PV widening was not performed because graft PV is considered as being a no-touch area. In thinking out of the box, we performed wedged-patch venoplasty to exceptionally narrow graft PV. A 4 year-old female patient underwent second LDLT due to progressive deterioration of graft function after 3 years. At first LDLT operation for biliary stresia, an iliac vein conduit was interposed for PV reconstruction. At second LDLT operation, the diameter of interposed PV was 10 mm, but the left liver graft PV was only 6 mm-sized. Uniquely, the left PV was waist only at first-order PV. To resolve this PV waist, a longitudinal incision was made to release the waist. A cold-preserved fresh iliac vein patch was inserted to widen the PV orifice. The patch size was adjusted to match the size of the recipient PV. The patient recovered uneventfully. This wedged-patch venoplasty technique can be applied to small-sized graft PV, to cope with PV size mismatching in LDLT.
MeSH Terms
Figure
Reference
-
1. Kang SH, Hwang S, Jung DH, Ahn CS, Moon DB, Ha TY, et al. Unification venoplasty to cope with recipient portal vein anomaly during living donor liver transplantation. Transplant Proc. 2013; 45:3000–3004.
Article2. Moon DB, Lee SG, Ahn CS, Ha TY, Park GC, Yu YD. Side-to-end renoportal anastomosis using an externally stented polytetrafluoroethylene vascular graft for a patient with a phlebosclerotic portal vein and a large spontaneous splenorenal shunt. J Am Coll Surg. 2011; 212:e7–e11.
Article3. Chen CL, Concejero A, Wang CC, Wang SH, Lin CC, Liu YW, et al. Living donor liver transplantation for biliary atresia: a single-center experience with first 100 cases. Am J Transplant. 2006; 6:2672–2679.
Article4. Ou HY, Concejero AM, Huang TL, Chen TY, Tsang LL, Chen CL, et al. Portal vein thrombosis in biliary atresia patients after living donor liver transplantation. Surgery. 2011; 149:40–47.
Article5. Hwang S, Kim DY, Ahn CS, Moon DB, Kim KM, Park GC, et al. Computational simulation-based vessel interposition reconstruction technique for portal vein hypoplasia in pediatric liver transplantation. Transplant Proc. 2013; 45:255–258.
Article6. Kwon JH, Hwang S, Song GW, Moon DB, Park GC, Kim SH, et al. Conjoined unification venoplasty for triple portal vein branches of right liver graft: a case report and technical refinement. Korean J Hepatobiliary Pancreat Surg. 2016; 20:61–65.
Article7. Lee HJ, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Long-term outcomes of portal Y-graft interposition for anomalous right portal veins in living donor liver transplantation. Transplant Proc. 2012; 44:454–456.
Article8. Hwang S, Lee SG, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Technique and outcome of autologous portal Y-graft interposition for anomalous right portal veins in living donor liver transplantation. Liver Transpl. 2009; 15:427–434.
Article9. Lee SG, Hwang S, Kim KH, Ahn CS, Park KM, Lee YJ, et al. Approach to anatomic variations of the graft portal vein in right lobe living-donor liver transplantation. Transplantation. 2003; 75:3 Suppl. S28–S32.
Article10. Ha TY, Hwang S, Moon DB, Ahn CS, Kim KH, Song GW, et al. Conjoined unification venoplasty for graft double portal vein branches as a modification of autologous Y-graft interposition. Liver Transpl. 2015; 21:707–710.
Article11. Hwang S, Kim KH, Kim DY, Kim KM, Ahn CS, Moon DB, et al. Anomalous hepatic vein anatomy of left lateral section grafts and customized unification venoplasty for pediatric living donor liver transplantation. Liver Transpl. 2013; 19:184–190.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wedged-patch venoplasty for graft left portal vein in pediatric living donor liver transplantation
- Tailored standardization of portal vein reconstruction for pediatric liver transplantation at Asan Medical Center
- Tailored techniques of graft outflow vein reconstruction in pediatric liver transplantation at Asan Medical Center
- Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft
- Graft outflow vein venoplasty for a laparoscopically harvested left lateral section graft in pediatric living donor liver transplantation