Ann Hepatobiliary Pancreat Surg.
2019 May;23(2):145-154. 10.14701/ahbps.2019.23.2.145.
Training in the Japanese Society of Hepato-Biliary-Pancreatic Surgery board certification system for expert surgeons during 225 consecutive pancreaticoduodenectomies
- Affiliations
-
- 1Department of Gastroenterological Surgery, Kumamoto University Graduate School of Medical Sciences, Kumamoto, Japan. daisukeh007@gmail.com
- 2Department of Gastroenterological Surgery, Omuta Tenryo Hospital, Omuta, Japan.
- KMID: 2448768
- DOI: http://doi.org/10.14701/ahbps.2019.23.2.145
Abstract
- BACKGROUNDS/AIMS
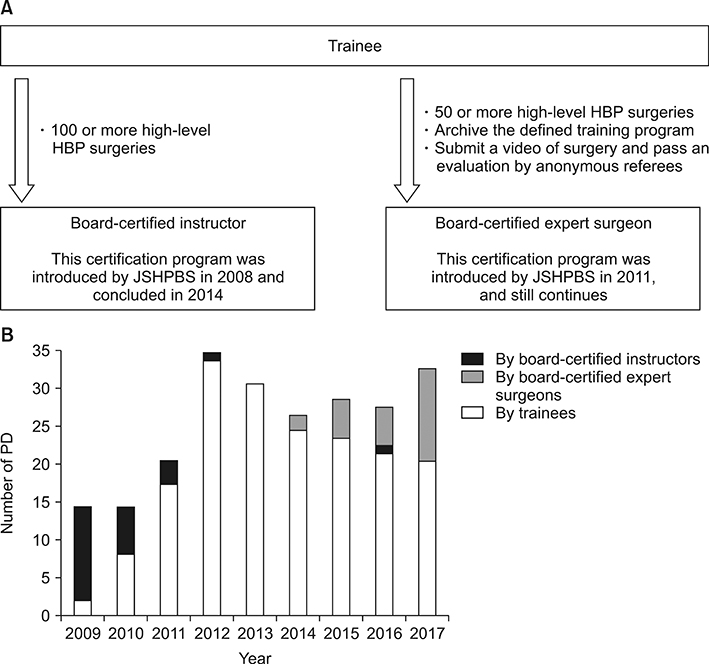
A board certification system has been established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery (JSHBPS) for certifying surgeons who can perform high-level hepato-biliary-pancreatic surgeries safely. The aim of this study was to compare operative outcomes after pancreaticoduodenectomy performed by trainees, board-certified instructors, and expert surgeons of JSHBPS to determine the efficacy of education of trainees and operative safety.
METHODS
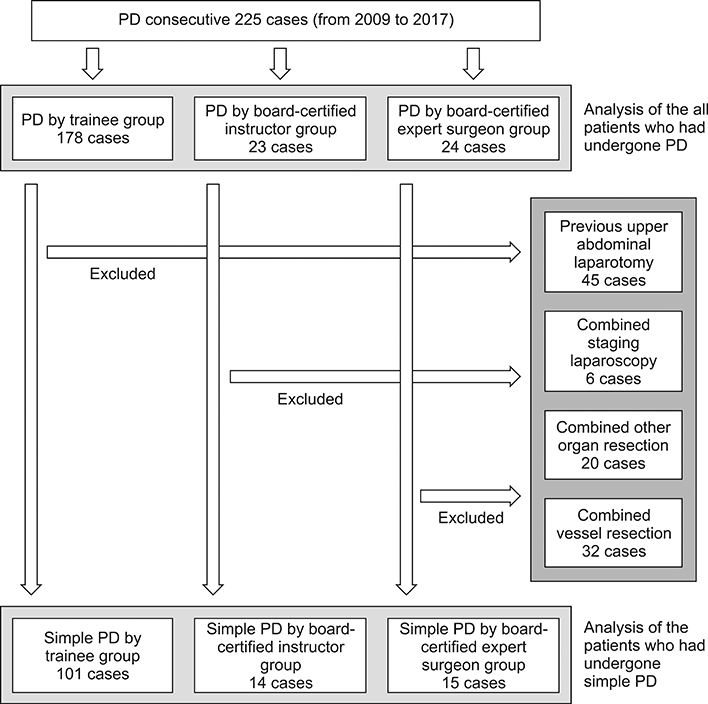
From 2009 to 2017, 225 consecutive patients underwent pancreaticoduodenectomy. Operations were performed by trainees, instructors, or JSHBPS experts. Clinical course and postoperative outcomes were retrospectively evaluated.
RESULTS
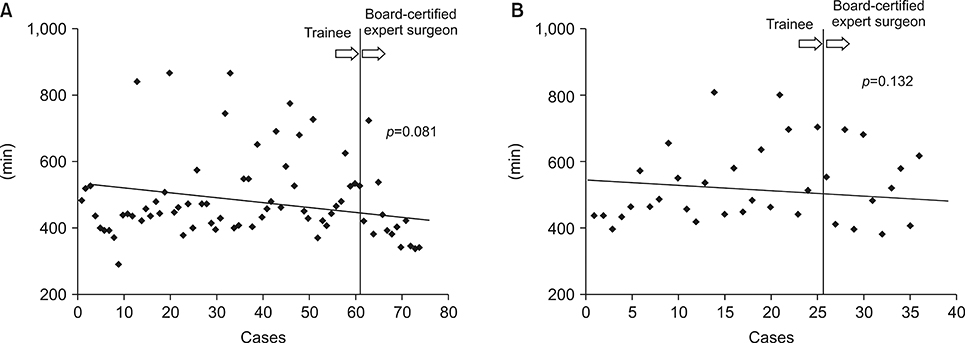
Twenty-two surgeons performed pancreaticoduodenectomy and two became expert surgeons. First, data of all patients who underwent pancreaticoduodenectomy (n=225) were analyzed. Significantly shorter median operating time and less median operative bleeding were documented in the experts' group (428 min, 576 g, respectively) than in the trainees' (498.5 min, 818 g, respectively) and instructors' (557 min, 911 g, respectively) groups. Morbidity did not differ significantly between the three groups. Second, data of patients who underwent simple pancreaticoduodenectomy (n=130) were analyzed. Similarly, operating time was shorter and operative bleeding less in the experts' group. With increasing their experiences, intraoperative bleeding by 2 surgeons became the expert surgeons decreased.
CONCLUSIONS
Surgeons judged experts by the JSHBPS board certification system achieve significantly shorter operating time and less operative bleeding during pancreaticoduodenectomy. In addition, PD performed by trainees has an acceptable incidence of postoperative complications. This is the first report which indicated the efficacy of education toward being the JSHPBS board-certified expert surgeon.
Keyword
MeSH Terms
Figure
Reference
-
1. Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 2014; 259:773–780.2. Otsubo T, Kobayashi S, Sano K, Misawa T, Ota T, Katagiri S, et al. Safety-related outcomes of the Japanese Society of Hepato-Biliary-Pancreatic Surgery board certification system for expert surgeons. J Hepatobiliary Pancreat Sci. 2017; 24:252–261.
Article3. Aoki S, Miyata H, Konno H, Gotoh M, Motoi F, Kumamaru H, et al. Risk factors of serious postoperative complications after pancreaticoduodenectomy and risk calculators for predicting postoperative complications: a nationwide study of 17,564 patients in Japan. J Hepatobiliary Pancreat Sci. 2017; 24:243–251.
Article4. Sugiura T, Mizuno T, Okamura Y, Ito T, Yamamoto Y, Kawamura I, et al. Impact of bacterial contamination of the abdominal cavity during pancreaticoduodenectomy on surgical-site infection. Br J Surg. 2015; 102:1561–1566.
Article5. Hashimoto D, Chikamoto A, Ohmuraya M, Hirota M, Baba H. Pancreaticodigestive anastomosis and the postoperative management strategies to prevent postoperative pancreatic fistula formation after pancreaticoduodenectomy. Surg Today. 2014; 44:1207–1213.
Article6. Hirono S, Murakami Y, Tani M, Kawai M, Okada K, Uemura K, et al. Identification of risk factors for pancreatic exocrine insufficiency after pancreaticoduodenectomy using a 13C-labeled mixed triglyceride breath test. World J Surg. 2015; 39:516–525.
Article7. Wood TW, Ross SB, Bowman TA, Smart A, Ryan CE, Sadowitz B, et al. High-volume hospitals with high-volume and low-volume surgeons: is there a “field effect” for pancreaticoduodenectomy? Am Surg. 2016; 82:407–411.
Article8. Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010; 145:634–640.9. Relles DM, Burkhart RA, Pucci MJ, Sendecki J, Tholey R, Drueding R, et al. Does resident experience affect outcomes in complex abdominal surgery? Pancreaticoduodenectomy as an example. J Gastrointest Surg. 2014; 18:279–285. discussion 285.
Article10. Shirai Y, Shiba H, Horiuchi T, Saito N, Furukawa K, Sakamoto T, et al. Assessment of outcome after pancreaticoduodenectomy by junior surgeons. Anticancer Res. 2016; 36:3505–3510.11. Hashimoto D, Takamori H, Sakamoto Y, Ikuta Y, Nakahara O, Furuhashi S, et al. Is an estimation of physiologic ability and surgical stress able to predict operative morbidity after pancreaticoduodenectomy? J Hepatobiliary Pancreat Sci. 2010; 17:132–138.
Article12. Hashimoto D, Chikamoto A, Arima K, Taki K, Inoue R, Imai K, et al. Unused sterile instruments for closure prevent wound surgical site infection after pancreatic surgery. J Surg Res. 2016; 205:38–42.
Article13. Hashimoto D, Nakagawa S, Umezaki N, Yamao T, Kitano Y, Yamamura K, et al. Efficacy and safety of postoperative anti-coagulation prophylaxis with enoxaparin in patients undergoing pancreatic surgery: a prospective trial and literature review. Pancreatology. 2017; 17:464–470.
Article14. DeOliveira ML, Winter JM, Schafer M, Cunningham SC, Cameron JL, Yeo CJ, et al. Assessment of complications after pancreatic surgery: a novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg. 2006; 244:931–937. discussion 937-939.15. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017; 161:584–591.16. Japan Pancreas Society. General rules for the study of pancreatic cancer. 6th ed. Osaka: Japan Pancreas Society;2009.17. Japanese Society of Biliary Surgery Society. General rules for surgical and pathological studies on cancer of the biliary tract. 5th ed. Japanese Society of Biliary Surgery Society;2003.18. Japan Pancreas Society. General rules for the study of pancreatic cancer. 7th ed. Osaka: Japan Pancreas Society;2009.19. Miyazaki M, Ohtsuka M, Miyakawa S, Nagino M, Yamamoto M, Kokudo N, et al. Classification of biliary tract cancers established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery: 3(rd) english edition. J Hepatobiliary Pancreat Sci. 2015; 22:181–196.20. Ito Y. Surgical education and postgraduate training in Japan. World J Surg. 2008; 32:2134–2137.
Article21. Krautz C, Nimptsch U, Weber GF, Mansky T, Grützmann R. Effect of hospital volume on in-hospital morbidity and mortality following pancreatic surgery in Germany. Ann Surg. 2018; 267:411–417.
Article22. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003; 349:2117–2127.
Article23. Tseng JF, Pisters PW, Lee JE, Wang H, Gomez HF, Sun CC, et al. The learning curve in pancreatic surgery. Surgery. 2007; 141:694–701.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pancreatobiliary Endoscopy Certification System from the Perspective of Insurance Policy
- Pediatric Abdominal Ultrasound Training Program: Standard Views
- An overview and the future of pediatric subspecialty board certification of the Korean Pediatric Society
- A Model of Accreditation System for Medical Subspecialty Board Certification in Korea
- Introduction to the Rule Book of Pancreatobiliary Endoscopy Certification