Hip Pelvis.
2019 Mar;31(1):4-10. 10.5371/hp.2019.31.1.4.
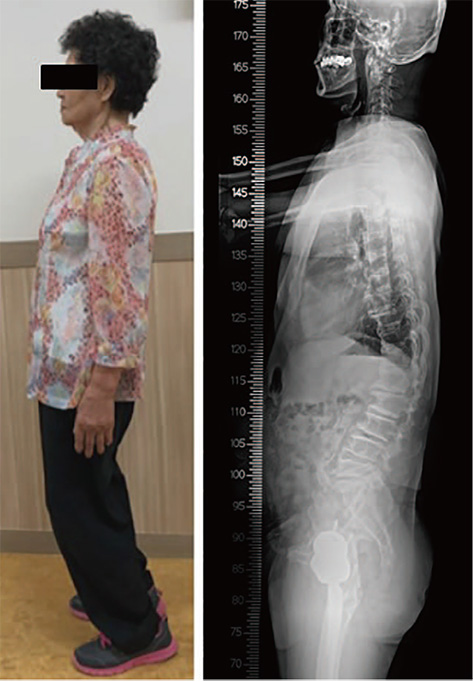
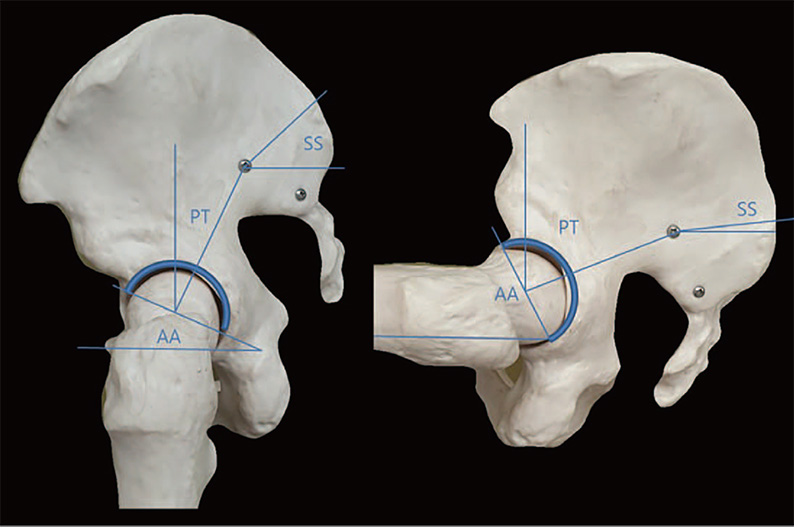
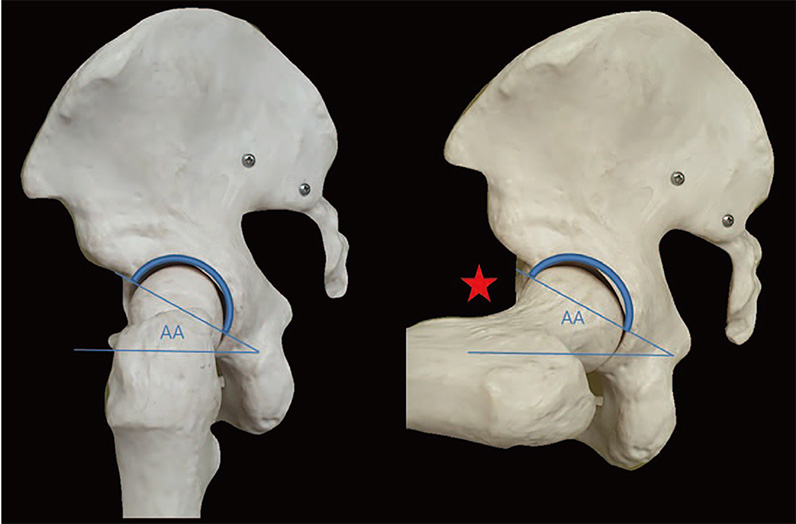
Effect of Spine-Pelvis Relationship in Total Hip Arthroplasty
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Chosun University, Gwangju, Korea. jo.suenghwan@chosun.ac.kr
- KMID: 2448035
- DOI: http://doi.org/10.5371/hp.2019.31.1.4
Abstract
- When spine-pelvic motion is normally coordinated, the pelvis may tilt posteriorly and acetabular anteversion may increase as the patient's position changes from standing to sitting; this scenario allows for improved clearance of the femoral head and neck during hip flexion. However, changes in the mobility of the spine and pelvis may result in impingement after total hip arthroplasty (THA), with the most obvious complication being dislocation. Understanding the spinal-pelvic relationship in the sagittal plane is essential for planning THA in patients with spinal fusion or a known spine disease. Careful attention should be payed to the cup position when performing THA on patients with an increased risk of dynamic impingement.
Keyword
MeSH Terms
Figure
Reference
-
1. Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006; 447:19–23.
Article2. Berry DJ. Unstable total hip arthroplasty: detailed overview. Instr Course Lect. 2001; 50:265–274.3. Gausden EB, Parhar HS, Popper JE, Sculco PK, Rush BNM. Risk factors for early dislocation following primary elective total hip arthroplasty. J Arthroplasty. 2018; 33:1567–1571.e2.
Article4. Malkani AL, Garber AT, Ong KL, et al. Total hip arthroplasty in patients with previous lumbar fusion surgery: are there more dislocations and revisions? J Arthroplasty. 2018; 33:1189–1193.
Article5. Sultan AA, Khlopas A, Piuzzi NS, Chughtai M, Sodhi N, Mont MA. The impact of spino-pelvic alignment on total hip arthroplasty outcomes: a critical analysis of current evidence. J Arthroplasty. 2018; 33:1606–1616.
Article6. Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978; 60:217–220.
Article7. Murphy WS, Yun HH, Hayden B, Kowal JH, Murphy SB. The safe zone range for cup anteversion is narrower than for inclination in THA. Clin Orthop Relat Res. 2018; 476:325–335.
Article8. Duval-Beaupére G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992; 20:451–462.
Article9. Legaye J, Duval-Beaupére G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998; 7:99–103.
Article10. Mac-Thiong JM, Berthonnaud E, Dimar JR 2nd, Betz RR, Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976). 2004; 29:1642–1647.
Article11. Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002; 11:80–87.
Article12. Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007; 16:1459–1467.
Article13. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010; 35:2224–2231.14. Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976). 1995; 20:1351–1358.
Article15. Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006; 15:415–422.
Article16. Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976). 1994; 19:1611–1618.
Article17. Rajnics P, Templier A, Skalli W, Lavaste F, Illés T. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord Tech. 2002; 15:24–30.
Article18. Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine (Phila Pa 1976). 2006; 31:E320–E325.19. Legaye J, Duval-Beaupere G, Barrau A, et al. Relationship between sacral pelvic incidence and acetabular orientation. Hip Int. 2011; 21:87–97.
Article20. Lazennec JY, Charlot N, Gorin M, et al. Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat. 2004; 26:136–144.
Article21. Lazennec JY, Riwan A, Gravez F, et al. Hip spine relationships: application to total hip arthroplasty. Hip Int. 2007; 17:Suppl 5. S91–S104.
Article22. Ike H, Dorr LD, Trasolini N, Stefl M, McKnight B, Heckmann N. Spine-pelvis-hip relationship in the functioning of a total hip replacement. J Bone Joint Surg Am. 2018; 100:1606–1615.
Article23. Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009; 467:32–42.
Article24. Lazennec JY, Boyer P, Gorin M, Catonné Y, Rousseau MA. Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res. 2011; 469:1103–1109.
Article25. Kanawade V, Dorr LD, Wan Z. Predictability of acetabular component angular change with postural shift from standing to sitting position. J Bone Joint Surg Am. 2014; 96:978–986.
Article26. Stefl M, Lundergan W, Heckmann N, et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017; 99-B:1 Supple A. 37–45.
Article27. Phan D, Bederman SS, Schwarzkopf R. The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J. 2015; 97-B:1017–1023.
Article28. Philippot R, Wegrzyn J, Farizon F, Fessy MH. Pelvic balance in sagittal and Lewinnek reference planes in the standing, supine and sitting positions. Orthop Traumatol Surg Res. 2009; 95:70–76.
Article29. Staibano P, Winemaker M, Petruccelli D, de Beer J. Total joint arthroplasty and preoperative low back pain. J Arthroplasty. 2014; 29:867–871.
Article30. McCarthy TF, Alipit V, Nevelos J, Elmallah RK, Mont MA. Acetabular cup anteversion and inclination in hip range of motion to impingement. J Arthroplasty. 2016; 31:9 Suppl. 264–268.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis on Radiologic Assessment Following Uncemented Total Hip Arthroplasty
- The Current Concepts of Total Hip Arthroplasty
- Consideration about Bearing Surfaces of Total Hip Arthroplasty
- New Paradigm of Total Hip Arthroplasty in Asia in 21st Century
- Spinopelvic Motion: A Simplified Approach to a Complex Subject