Korean J Radiol.
2019 Jun;20(6):947-955. 10.3348/kjr.2018.0599.
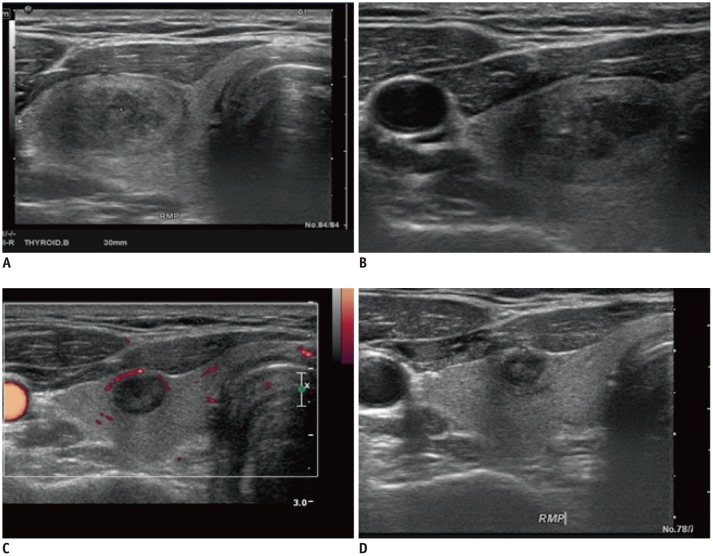
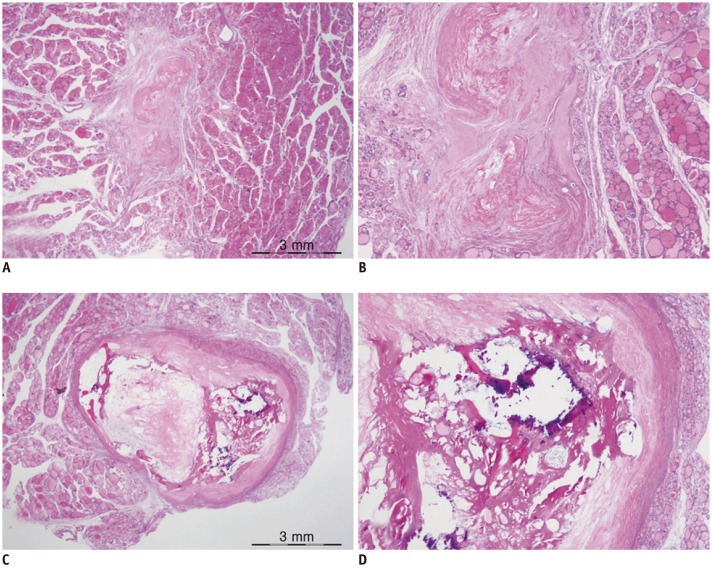
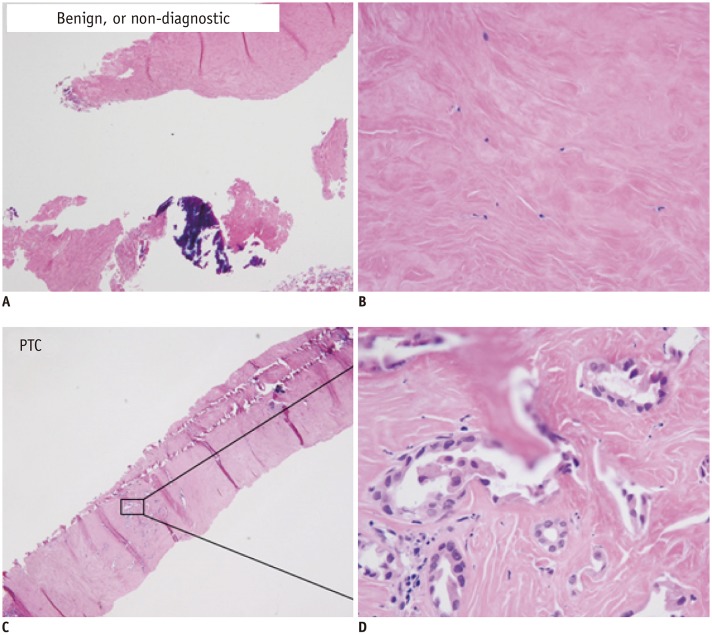
Degenerating Thyroid Nodules: Ultrasound Diagnosis, Clinical Significance, and Management
- Affiliations
-
- 1Department of Medical Ultrasonics, The Third Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China.
- 2Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. radbaek@naver.com
- 3Department of Hospital Pathology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2447073
- DOI: http://doi.org/10.3348/kjr.2018.0599
Abstract
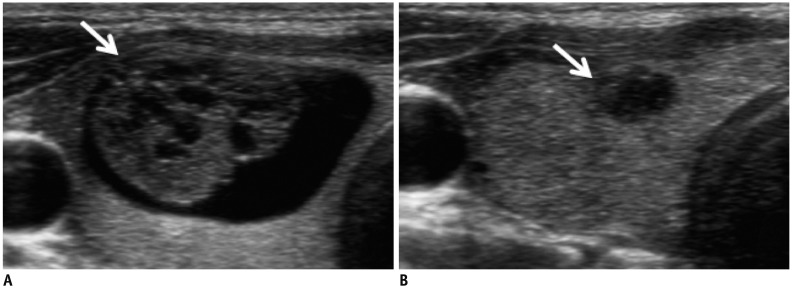
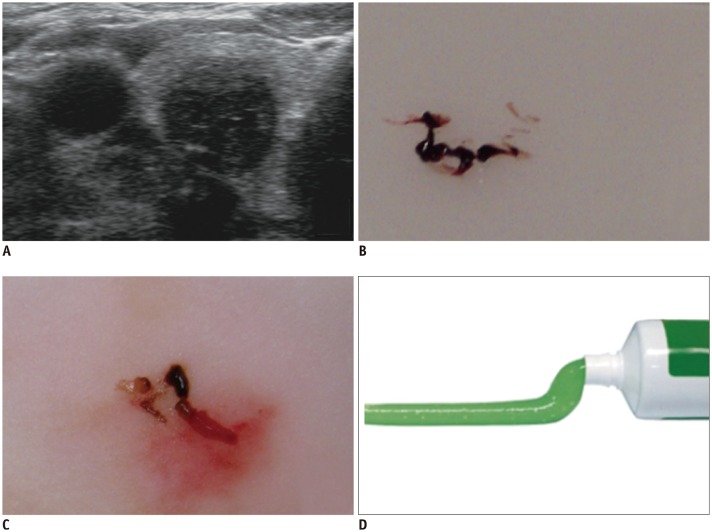
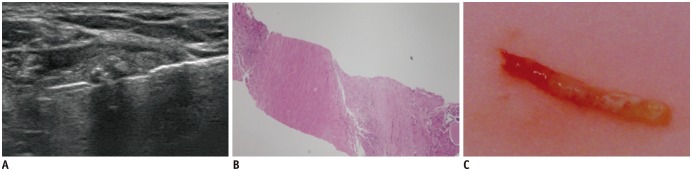
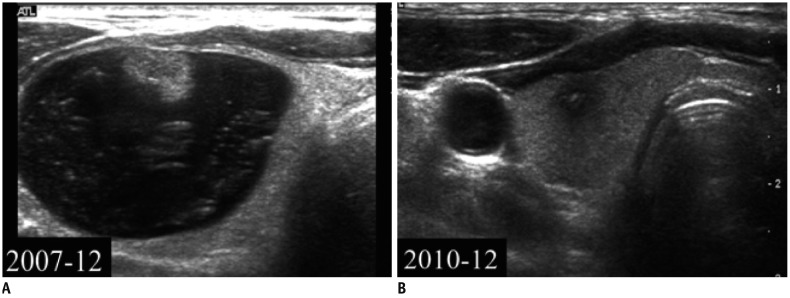
- Degenerating nodules (DNs), which primarily manifest as benign thyroid nodules, are one of the main causes of discordance in ultrasonography (US) and cytological assessments. Intranodular hemorrhage is one of the mechanisms contributing to discordant nodules, and an impaired blood supply may explain further DN shrinkage and infarction. The surgical specimens can be divided into acute and chronic stages based on the histological changes, which usually mimic the US features of malignant tumors. Serial US follow-up should be recommended instead of other unnecessary procedures. However, repeated fine-needle aspiration, diagnostic surgery, or core-needle biopsy may still be necessary for indeterminable or highly suspicious DNs.
MeSH Terms
Figure
Cited by 1 articles
-
2019 Practice guidelines for thyroid core needle biopsy: a report of the Clinical Practice Guidelines Development Committee of the Korean Thyroid Association
Chan Kwon Jung, Jung Hwan Baek, Dong Gyu Na, Young Lyun Oh, Ka Hee Yi, Ho-Cheol Kang
J Pathol Transl Med. 2020;54(1):64-86. doi: 10.4132/jptm.2019.12.04.
Reference
-
1. Alexander EK, Hurwitz S, Heering JP, Benson CB, Frates MC, Doubilet PM, et al. Natural history of benign solid and cystic thyroid nodules. Ann Intern Med. 2003; 138:315–318. PMID: 12585829.
Article2. Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedüs L, et al. AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. J Endocrinol Invest. 2010; 33(5 Suppl):1–50.
Article3. Ha EJ, Baek JH, Lee JH, Song DE, Kim JK, Shong YK, et al. Sonographically suspicious thyroid nodules with initially benign cytologic results: the role of a core needle biopsy. Thyroid. 2013; 23:703–708. PMID: 23544697.
Article4. Lee HY, Baek JH, Ha EJ, Park JW, Lee JH, Song DE, et al. Malignant-looking thyroid nodules with size reduction: core needle biopsy results. Ultrasonography. 2016; 35:327–334. PMID: 27184652.
Article5. Ko MS, Jeong KS, Shong YK, Gong GY, Baek JH, Lee JH. Collapsing benign cystic nodules of the thyroid gland: sonographic differentiation from papillary thyroid carcinoma. AJNR Am J Neuroradiol. 2012; 33:124–127. PMID: 22158923.
Article6. Lacout A, Chevenet C, Marcy PY. Suspicious thyroid nodule management with nondiagnostic results at cytologic examination: how to diagnosis mummified benign thyroid nodules. Radiology. 2015; 277:303–304. PMID: 26402498.
Article7. Lacout A, Chevenet C, Marcy PY. Mummified thyroid syndrome. AJR Am J Roentgenol. 2016; 206:837–845. PMID: 27003052.
Article8. Kholová I. Vanishing thyroid gland tumors: infarction as consequence of FNA? Diagn Cytopathol. 2016; 44:568–573. PMID: 27094979.
Article9. Bhatia P, Deniwar A, Mohamed HE, Sholl A, Murad F, Aslam R, et al. Vanishing tumors of thyroid: histological variations after fine needle aspiration. Gland Surg. 2016; 5:270–277. PMID: 27294033.
Article10. Bolat F, Kayaselcuk F, Nursal TZ, Reyhan M, Bal N, Yildirim S, et al. Histopathological changes in thyroid tissue after fine needle aspiration biopsy. Pathol Res Pract. 2007; 203:641–645. PMID: 17582696.
Article11. LiVolsi VA, Merino MJ. Worrisome histologic alterations following fine-needle aspiration of the thyroid (WHAFFT). Pathol Annu. 1994; 29(Pt 2):99–120. PMID: 7936753.12. Polyzos SA, Patsiaoura K, Zachou K. Histological alterations following thyroid fine needle biopsy: a systematic review. Diagn Cytopathol. 2009; 37:455–465. PMID: 19306421.
Article13. Lacout A, Isaac S, Marcy PY. Micro-medullary thyroid carcinoma: a diagnosis not to be missed. Postgrad Med J. 2015; 91:236–237. PMID: 25862709.
Article14. Cochand-Priollet B, Vielh P, Royer B, Belleannée G, Collet JF, Goubin-Versini I, et al. sous l'égide de la Société française de cytologie clinique. [Thyroid cytopathology: Bethesda System 2010]. Ann Pathol. 2012; 32:177–183. PMID: 22748331.15. Yeon JS, Baek JH, Lim HK, Ha EJ, Kim JK, Song DE, et al. Thyroid nodules with initially nondiagnostic cytologic results: the role of core-needle biopsy. Radiology. 2013; 268:274–280. PMID: 23525204.
Article16. Screaton NJ, Berman LH, Grant JW. US-guided core-needle biopsy of the thyroid gland. Radiology. 2003; 226:827–832. PMID: 12601219.
Article17. Gharib H, Goellner JR. Fine-needle aspiration biopsy of the thyroid: an appraisal. Ann Intern Med. 1993; 118:282–289. PMID: 8420446.
Article18. Hamburger JI, Hamburger SW. Fine needle biopsy of thyroid nodules: avoiding the pitfalls. N Y State J Med. 1986; 86:241–249. PMID: 3520410.19. Ito Y, Amino N, Yokozawa T, Ota H, Ohshita M, Murata N, et al. Ultrasonographic evaluation of thyroid nodules in 900 patients: comparison among ultrasonographic, cytological, and histological findings. Thyroid. 2007; 17:1269–1276. PMID: 17988196.
Article20. Kwak JY, Koo H, Youk JH, Kim MJ, Moon HJ, Son EJ, et al. Value of US correlation of a thyroid nodule with initially benign cytologic results. Radiology. 2010; 254:292–300. PMID: 20019136.
Article21. Kwak JY, Kim EK, Kim HJ, Kim MJ, Son EJ, Moon HJ. How to combine ultrasound and cytological information in decision making about thyroid nodules. Eur Radiol. 2009; 19:1923–1931. PMID: 19277669.
Article22. Chernyavsky VS, Shanker BA, Davidov T, Crystal JS, Eng O, Ibrahim K, et al. Is one benign fine needle aspiration enough? Ann Surg Oncol. 2012; 19:1472–1476. PMID: 21969084.
Article23. Kuma K, Matsuzuka F, Kobayashi A, Hirai K, Morita S, Miyauchi A, et al. Outcome of long standing solitary thyroid nodules. World J Surg. 1992; 16:583–587. discussion 587-588. PMID: 1413828.
Article24. Aulicino MR, Kaneko M, Uinger PD. Excessive endothelial cell proliferation occurring in an organizing thyroid hematoma: report of a case and review of the literature. Endocr Pathol. 1995; 6:153–158. PMID: 12114651.
Article25. Ersöz C, Soylu L, Erkoçak EU, Tetiker T, Gümürdülü D. Histologic alterations in the thyroid gland after fine-needle aspiration. Diagn Cytopathol. 1997; 16:230–232. PMID: 9099543.
Article26. Pandit AA, Phulpagar MD. Worrisome histologic alterations following fine needle aspiration of the thyroid. Acta Cytol. 2001; 45:173–179. PMID: 11284302.
Article27. Ha EJ, Baek JH, Lee JH, Lee HY, Song DE, Kim JK, et al. A focal marked hypoechogenicity within an isoechoic thyroid nodule: is it a focal malignancy or not? Acta Radiol. 2015; 56:814–819. PMID: 24938659.
Article28. Jung SL, Jung CK, Kim SH, Kang BJ, Ahn KJ, Kim BS, et al. Histopathologic findings related to the indeterminate or inadequate results of fine-needle aspiration biopsy and correlation with ultrasonographic findings in papillary thyroid carcinomas. Korean J Radiol. 2010; 11:141–148. PMID: 20191060.
Article29. Chung SR, Baek JH, Park HS, Choi YJ, Sung TY, Song DE, et al. Ultrasound-pathology discordant nodules on core-needle biopsy: malignancy risk and management strategy. Thyroid. 2017; 27:707–713. PMID: 28326900.
Article30. Koo JH, Shin JH, Han BK, Ko EY, Kang SS. Cystic thyroid nodules after aspiration mimicking malignancy: sonographic characteristics. J Ultrasound Med. 2010; 29:1415–1421. PMID: 20876894.31. Moon HJ, Kim EK, Kwak JY. Malignancy risk stratification in thyroid nodules with benign results on cytology: combination of thyroid imaging reporting and data system and Bethesda system. Ann Surg Oncol. 2014; 21:1898–1903. PMID: 24558069.
Article32. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2016; 17:370–395. PMID: 27134526.
Article33. Kim JH, Na DG, Lee H. Ultrasonographic echogenicity and histopathologic correlation of thyroid nodules in core needle biopsy specimens. Korean J Radiol. 2018; 19:673–681. PMID: 29962873.
Article34. Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002; 87:1941–1946. PMID: 11994321.
Article35. Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002; 178:687–691. PMID: 11856699.
Article36. Frates MC, Benson CB, Doubilet PM, Cibas ES, Marqusee E. Can color Doppler sonography aid in the prediction of malignancy of thyroid nodules? J Ultrasound Med. 2003; 22:127–131. quiz 132–134. PMID: 12562117.
Article37. Iannuccilli JD, Cronan JJ, Monchik JM. Risk for malignancy of thyroid nodules as assessed by sonographic criteria: the need for biopsy. J Ultrasound Med. 2004; 23:1455–1464. PMID: 15498910.38. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Thyroid Study Group, Korean Society of Neuro- and Head and Neck Radiology. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008; 247:762–770. PMID: 18403624.
Article39. Silver RJ, Parangi S. Management of thyroid incidentalomas. Surg Clin North Am. 2004; 84:907–919. PMID: 15145242.
Article40. Propper RA, Skolnick ML, Weinstein BJ, Dekker A. The nonspecificity of the thyroid halo sign. J Clin Ultrasound. 1980; 8:129–132. PMID: 6767745.
Article41. Sillery JC, Reading CC, Charboneau JW, Henrichsen TL, Hay ID, Mandrekar JN. Thyroid follicular carcinoma: sonographic features of 50 cases. AJR Am J Roentgenol. 2010; 194:44–54. PMID: 20028904.42. Lacout A, Marcy PY. Highlights on power Doppler US of thyroid malignancy. Radiology. 2010; 257:586–587. author reply 587. PMID: 20959551.
Article43. Lacout A, Chevenet C, Marcy PY. Reverse mummified thyroid syndrome. AJR Am J Roentgenol. 2016; 207:W23. PMID: 27145041.
Article44. Simpson KW, Albores-Saavedra J. Unusual findings in papillary thyroid microcarcinoma suggesting partial regression: a study of two cases. Ann Diagn Pathol. 2007; 11:97–102. PMID: 17349567.
Article45. Hwang SH, Sung JM, Kim EK, Moon HJ, Kwak JY. Imaging-cytology correlation of thyroid nodules with initially benign cytology. Int J Endocrinol. 2014; 2014:491508. PMID: 25374600.
Article46. Shin JH, Han BK, Ko K, Choe YH, Oh YL. Value of repeat ultrasound-guided fine-needle aspiration in nodules with benign cytological diagnosis. Acta Radiol. 2006; 47:469–473. PMID: 16796308.
Article47. Nasrollah N, Trimboli P, Guidobaldi L, Cicciarella Modica DD, Ventura C, Ramacciato G, et al. Thin core biopsy should help to discriminate thyroid nodules cytologically classified as indeterminate. A new sampling technique. Endocrine. 2013; 43:659–665. PMID: 23070753.
Article48. Park KT, Ahn SH, Mo JH, Park YJ, Park DJ, Choi SI, et al. Role of core needle biopsy and ultrasonographic finding in management of indeterminate thyroid nodules. Head Neck. 2011; 33:160–165. PMID: 20848434.
Article49. Suh CH, Baek JH, Lee JH, Choi YJ, Kim JK, Sung TY, et al. The role of core-needle biopsy as a first-line diagnostic tool for initially detected thyroid nodules. Thyroid. 2016; 26:395–403. PMID: 26651390.
Article50. Yoon JH, Kim EK, Kwak JY, Moon HJ. Effectiveness and limitations of core needle biopsy in the diagnosis of thyroid nodules: review of current literature. J Pathol Transl Med. 2015; 49:230–235. PMID: 26018514.
Article51. Zhang M, Zhang Y, Fu S, Lv F, Tang J. Thyroid nodules with suspicious ultrasound findings: the role of ultrasound-guided core needle biopsy. Clin Imaging. 2014; 38:434–438. PMID: 24746446.
Article52. Trimboli P, Nasrollah N, Guidobaldi L, Taccogna S, Cicciarella Modica DD, Amendola S, et al. The use of core needle biopsy as first-line in diagnosis of thyroid nodules reduces false negative and inconclusive data reported by fine-needle aspiration. World J Surg Oncol. 2014; 12:61. PMID: 24661377.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Updated guidelines for the diagnosis and management of thyroid nodules
- Elastography of the Thyroid Glands
- Application of contrast-enhanced ultrasound for evaluation of thyroid nodules
- Sonographic Evaluation of Thyroid Nodules
- Diagnosis of Parathyroid Adenoma Detected during Thyroid Ultrasound: The Role of Parathormone Measurement in Fine-Needle Aspiration Washout