Clin Orthop Surg.
2019 Jun;11(2):192-199. 10.4055/cios.2019.11.2.192.
Preoperative Pain Control in Arthroscopic Rotator Cuff Repair: Does It Matter?
- Affiliations
-
- 1Funabashi Orthopaedic Sports Medicine Center, Funabashi, Japan. nqi37568@nifty.com
- 2Department of Orthopaedic Surgery, The Jikei University School of Medicine, Tokyo, Japan.
- 3Department of Orthopaedic Surgery, Kanagawa Rehabilitation Hospital, Atsugi, Japan.
- KMID: 2445055
- DOI: http://doi.org/10.4055/cios.2019.11.2.192
Abstract
- BACKGROUND
The purpose of this study was to clarify the importance of preoperative pain control using corticosteroid injections in patients with persistent rest pain (RP) before arthroscopic rotator cuff repair (ARCR).
METHODS
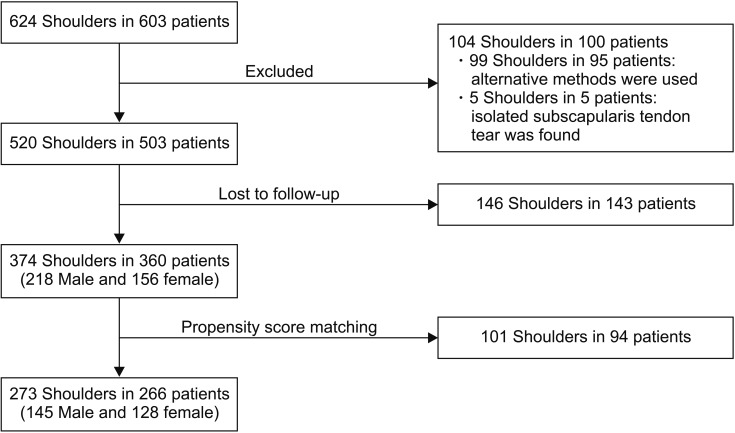
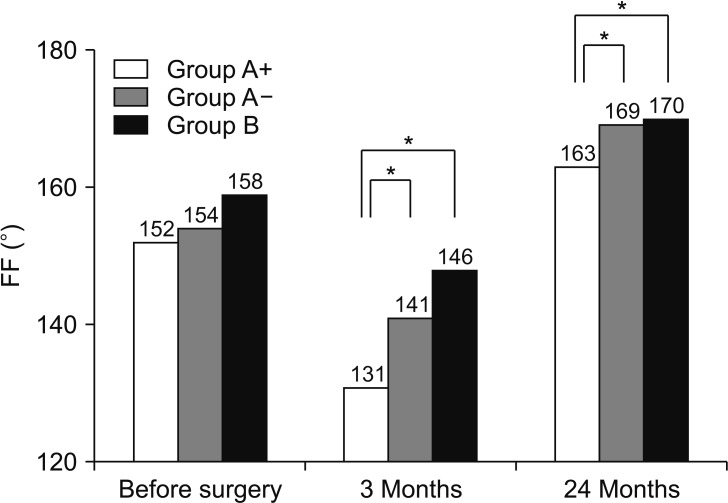
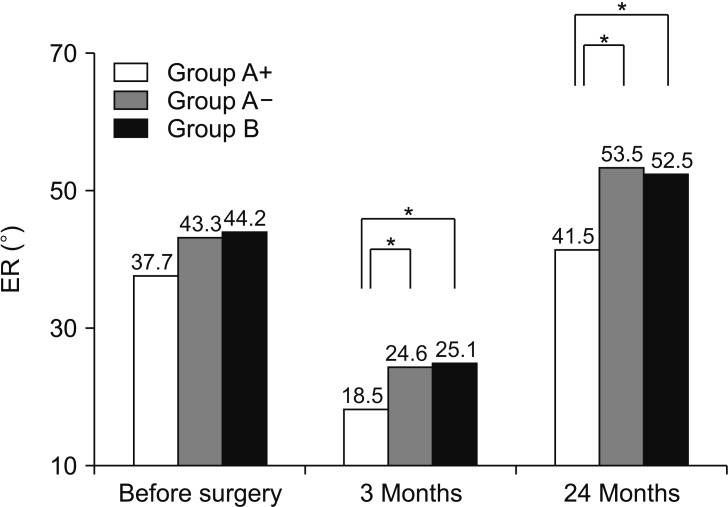
A total of 360 patients (374 shoulders) who underwent primary ARCR and were followed up for at least 2 years were enrolled. After one-to-one propensity score matching, 266 patients (145 men and 128 women, 273 shoulders) were included in the study. Their mean age was 65.2 ± 7.7 years (range, 42 to 88 years) at the time of surgery. The patients were divided into three groups: those who required several intra-articular or subacromial bursa corticosteroid injections preoperatively for refractory RP (group A+), those in whom RP was resolved preoperatively (group A−), and those who had no RP and did not require any injections (group B). The incidence of postoperative RP and preoperative and final follow-up American Shoulder and Elbow Surgeons (ASES) scores were compared among the three groups.
RESULTS
The incidence of postoperative RP was significantly higher in group A+ (35/91 cases, 38.5%) than in group A− (10/91, 11.0%) and group B (7/91, 7.7%, p < 0.001 for both). The preoperative ASES score was significantly lower in group A+ (33.2 ± 14.2) than in group A− (53.9 ± 11.9) and group B (62.3 ± 11.2, p < 0.001 for both), and it was significantly lower in group A− than in group B (p = 0.000). The final follow-up ASES score was significantly lower in group A+ (92.1 ± 8.4) than in group A− (97.6 ± 5.4) and group B (99.0 ± 2.5, p < 0.001 for both). There was no significant difference in the final follow-up ASES score between group A− and group B (p = 0.242).
CONCLUSIONS
Patients in whom preoperative RP could be resolved before surgery achieved postoperative outcomes comparable to those in patients who had no RP before surgery, whereas the outcomes in patients with refractory preoperative RP were inferior. The results suggest that preoperative pain control is important in patients undergoing ARCR.
Figure
Reference
-
1. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005; 21(11):1307–1316. PMID: 16325080.
Article2. Walton JR, Murrell GA. A two-year clinical outcomes study of 400 patients, comparing open surgery and arthroscopy for rotator cuff repair. Bone Joint Res. 2012; 1(9):210–217. PMID: 23610693.
Article3. Tonotsuka H, Sugaya H, Takahashi N, Kawai N, Sugiyama H, Marumo K. Target range of motion at 3 months after arthroscopic rotator cuff repair and its effect on the final outcome. J Orthop Surg (Hong Kong). 2017; 25(3):2309499017730423. PMID: 28920548.
Article4. Gotoh M, Hamada K, Yamakawa H, et al. Interleukin-1-induced glenohumeral synovitis and shoulder pain in rotator cuff diseases. J Orthop Res. 2002; 20(6):1365–1371. PMID: 12472254.
Article5. Weiss JJ. Intra-articular steroids in the treatment of rotator cuff tear: reappraisal by arthrography. Arch Phys Med Rehabil. 1981; 62(11):555–557. PMID: 7316710.6. Gialanella B, Prometti P. Effects of corticosteroids injection in rotator cuff tears. Pain Med. 2011; 12(10):1559–1565. PMID: 21951654.
Article7. Lee DH, Hong JY, Lee MY, Kwack KS, Yoon SH. Relation between subacromial bursitis on ultrasonography and efficacy of subacromial corticosteroid injection in rotator cuff disease: a prospective comparison study. Arch Phys Med Rehabil. 2017; 98(5):881–887. PMID: 28034721.
Article8. Shin SJ, Do NH, Lee J, Ko YW. Efficacy of a subacromial corticosteroid injection for persistent pain after arthroscopic rotator cuff repair. Am J Sports Med. 2016; 44(9):2231–2236. PMID: 27268240.
Article9. Okamura K, Kobayashi T, Yamamoto A, et al. Shoulder pain and intra-articular interleukin-8 levels in patients with rotator cuff tears. Int J Rheum Dis. 2017; 20(2):177–181. PMID: 25930944.
Article10. Santavirta S, Konttinen YT, Antti-Poika I, Nordstrom D. Inflammation of the subacromial bursa in chronic shoulder pain. Arch Orthop Trauma Surg. 1992; 111(6):336–340. PMID: 1360227.
Article11. Terabayashi N, Watanabe T, Matsumoto K, et al. Increased blood flow in the anterior humeral circumflex artery correlates with night pain in patients with rotator cuff tear. J Orthop Sci. 2014; 19(5):744–749. PMID: 25069807.
Article12. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007; 89(5):953–960. PMID: 17473131.13. Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009; 25(8):880–890. PMID: 19664508.14. Clement ND, Hallett A, MacDonald D, Howie C, McBirnie J. Does diabetes affect outcome after arthroscopic repair of the rotator cuff? J Bone Joint Surg Br. 2010; 92(8):1112–1117. PMID: 20675756.
Article15. Manaka T, Ito Y, Matsumoto I, Takaoka K, Nakamura H. Functional recovery period after arthroscopic rotator cuff repair: is it predictable before surgery? Clin Orthop Relat Res. 2011; 469(6):1660–1666. PMID: 21107925.
Article16. Keener JD, Galatz LM, Stobbs-Cucchi G, Patton R, Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair: a prospective randomized trial of immobilization compared with early motion. J Bone Joint Surg Am. 2014; 96(1):11–19. PMID: 24382719.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revisional Rotator Cuff Repair
- New Retear Pattern after Rotator Cuff Repair at Previous Intact Portion of Rotator Cuff
- Various Regimens for the Functional Recovery after Arthroscopic Shoulder Surgery
- Surgical treatment for rotator cuff tears: the way it ought to be
- Arthroscopic Bony Procedure During of Rotator Cuff Repair: Acromioplasty, Distal Clavicle Resection, Footprint Preparation and Coracoplasty