Korean J Adult Nurs.
2019 Apr;31(2):165-175. 10.7475/kjan.2019.31.2.165.
Factors Influencing Functional Health of Patients with Chronic Insomnia based on Theory of Unpleasant Symptoms
- Affiliations
-
- 1Assistant Professor, College of Nursing, Eulji University, Seongnam, Korea. haahaa21@hanmail.net
- 2Professor, College of Nursing, Yonsei University, Seoul, Korea.
- 3Professor, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2444135
- DOI: http://doi.org/10.7475/kjan.2019.31.2.165
Abstract
- PURPOSE
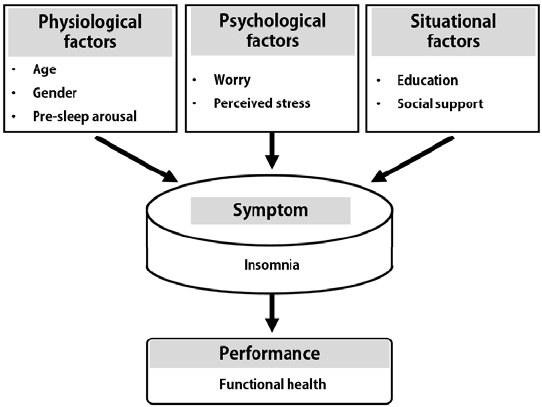
The purpose of this study was to identify factors influencing functional health of patients with chronic insomnia based on the Theory of Unpleasant Symptoms (TOUS).
METHODS
Data were collected from 184 patients with chronic insomnia who had been treated at the sleep center in hospital in South Korea. Data were collected from 23 December 2014 to 18 May 2015 through self-reported questionnaires from pre-sleep arousal, worry, perceived stress, social support, insomnia symptom, and functional health. Data were analyzes using an independent t-test, one-way ANOVA, Pearson's correlation coefficient, and hierarchical multiple regression analysis with the SPSS/WIN 21.0 program.
RESULTS
The regression model had an adjusted R2 of 50%, which indicated that pre-sleep arousal, social support, perceived stress, education, and insomnia symptom were significant predictors of functional health in patients with insomnia.
CONCLUSION
In order to improve the functional health of patient's with chronic insomnia, clinical nurses should develop and provide nursing interventions that improve social support and reduce pre-sleep arousal, stress, and insomnia symptoms.
Figure
Cited by 1 articles
-
Factors influencing the health-related quality of life in Korean menopausal women: a cross-sectional study based on the theory of unpleasant symptoms
Ji-Hyun Kang, Moon-Jeong Kim
Korean J Women Health Nurs. 2022;28(2):100-111. doi: 10.4069/kjwhn.2022.05.29.
Reference
-
1. Rosekind MR, Gregory KB. Insomnia risks and costs: health, safety, and quality of life. The American Journal of Managed Care. 2010; 16(8):617–626.2. Vgontzas AN, Fernandez-Mendoza J, Bixler EO, Singareddy R, Shaffer ML, Calhoun SL, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012; 35(1):61–68. DOI: 10.5665/sleep.1586.
Article3. Karlson CW, Gallagher MW, Olson CA, Hamilton NA. Insomnia symptoms and well-being: longitudinal follow-up. Health Psychology. 2013; 32(3):311–319. DOI: 10.1037/a0028186.
Article4. Trauer JM, Qian MY, Doyle JS, Rajaratnam SMW, Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta analysis. Annals of Internal Medicine. 2015; 163(3):191–204. DOI: 10.7326/M14-2841.5. Martínez MP, Miró E, Sánchez AI, Díaz-Piedra C, Cáliz R, Vlaeyen JWS, et al. Cognitive -behavioral therapy for insomnia and sleep hygiene in fibromyalgia: a randomized controlled trial. Journal of Behavioral Medicine. 2014; 37(4):683–697. DOI: 10.1007/s10865-013-9520-y.6. Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Medicine Reviews. 2010; 14(1):9–15. DOI: 10.1016/j.smrv.2009.05.002.
Article7. Shim TG, Rhee M-K. Does the sleep and emotion regulation mediates the effects of stress and worry on well-being? Korean Journal of Health Psychology. 2013; 18(4):783–806.8. Gosling JA, Batterham PJ, Glozier N, Christensen H. The influence of job stress, social support and health status on intermittent and chronic sleep disturbance: an 8-year longitudinal analysis. Sleep Medicine. 2014; 15(8):979–985. DOI: 10.1016/j.sleep.2014.04.007.
Article9. Jones D, Duffy ME, Flanagan J, Foster F. Psychometric evaluation of the Functional Health Pattern Assessment Screening Tool (FHPAST). International Journal of Nursing Knowledge. 2012; 23(3):140–145. DOI: 10.1111/j.2047-3095.2012.01224.x.
Article10. Lenz ER, Suppe F, Gift AG, Pugh LC, Milligan RA. Collaborative development of middle-range nursing theories: toward a theory of unpleasant symptoms. Advances in Nursing Science. 1995; 17(3):1–13. DOI: 10.1097/00012272-199503000-00003.11. Woods SJ, Kozachik SL, Hall RJ. Subjective sleep quality in women experiencing intimate partner violence: contributions of situational, psychological, and physiological factors. Journal of Traumatic Stress. 2010; 23(1):141–150. DOI: 10.1002/jts.20495.
Article12. Jeon J, Hwang S. A structural equation modeling on premenstrual syndrome in adolescent girls. Journal of Korean Academy of Nursing. 2014; 44(6):660–671. DOI: 10.4040/jkan.2014.44.6.660.
Article13. Nicassio PM, Mendlowitz DR, Fussell JJ, Petras L. The phenomenology of the pre-sleep state: the development of the presleep arousal scale. Behaviour Research and Therapy. 1985; 23(3):263–271.
Article14. Cho YE, Kwon JH. Verification of the integrated model of insomnia including cognitive process and stress. Korean Journal of Clinical Psychology. 2012; 31(1):135–150.15. Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy. 1990; 28(6):487–495. DOI: 10.1016/0005-7967(90)90135-6.
Article16. Kim JW, Min BB. Intolerance of uncntainty and problem orientation in worry. Poster presented at: The annual conference of the Korean Psychological Association. 1998 June 20; Seoul, South Korea.17. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983; 24(4):385–396. DOI: 10.2307/2136404.
Article18. Lee JE. The effects of self-complexity and self-efficacy on depression and perceived stress [master's thesis]. Suwon: Ajou University;2005. 18–20.19. Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991; 32(6):705–714. DOI: 10.1016/0277-9536(91)90150-B.
Article20. Lim MK. Relationships between social support and health among low income groups in urban area [master's thesis]. Seoul: Seoul National University;2002. 15–20.21. Morin CM. Insomnia psychological assessment and management. New York: Guilford Press;1993. p. 1–23.22. Jones D, Duffy ME, Flanagan J, Foster F. Psychometric evaluation of the Functional Health Pattern Assessment Screening Tool (FHPAST). International Journal of Nursing Knowledge. 2012; 23(3):140–145. DOI: 10.1111/j.2047-3095.2012.01224.x.
Article23. Keum R, Kim SA. Perceived functional health patterns and recovery in people with schizophrenia spectrum disorders. Journal of Korean Academy of Psychiatric and Mental Health Nursing. 2012; 21(3):238–249.
Article24. Lee KC. Statistics for health care. 1st ed. Seoul: Hyunmoonsa;2011. p. 152–162.25. Park SI, Kim S. Mediating effect of self-efficacy in the relationship between anger and functional health of homeless men. Journal of Korean Academy Nursing. 2014; 44(4):361–370. DOI: 10.4040/jkan.2014.44.4.361.
Article26. Andersen ML, Alvarenga TF, Mazaro-Costa R, Hachul HC, Tufik S. The association of testosterone, sleep, and sexual function in men and women. Brain Research. 2011; 1416(6):80–104. DOI: 10.1016/j.brainres.2011.07.060.
Article27. van de Laar M, Verbeek I, Pevernagie D, Aldenkamp A, Overeem S. The role of personality traits in insomnia. Sleep Medicine Reviews. 2010; 14(1):61–68. DOI: 10.1016/j.smrv.2009.07.007.
Article28. Seligman ME, Csikszentmihalyi M. Positive psychology: an introduction. American Psychologist. 2000; 55(1):5–14. DOI: 10.1037/0003-066X.55.1.5.
Article29. Gunn HE, Troxel WM, Hall MH, Buysse DJ. Interpersonal distress is associated with sleep and arousal in insomnia and good sleepers. Journal of Psychosomatic Research. 2014; 76(3):242–248. DOI: 10.1016/j.jpsychores.2013.11.010.
Article30. Palagini L, Bruno RM, Cheng P, Mauri M, Taddei S, Ghiadoni L, et al. Relationship between insomnia symptoms, perceived stress and coping strategies in subjects with arterial hypertension: psychological factors may play a modulating role. Sleep Medicine. 2016; 19:108–115. DOI: 10.1016/j.sleep.2015.09.026.
Article31. Benham G. Sleep: an important factor in stress-health models. Stress & Health. 2010; 26(3):204–214. DOI: 10.1002/smi.1304.
Article32. Barbosa P, Raymond G, Zlotnick C, Wilk J, Toomey R, Mitchell J. Mindfulness-based stress reduction training is associated with greater empathy and reduced anxiety for graduate healthcare students. Education for Health. 2013; 26(1):9–14. DOI: 10.4103/1357-6283.112794.
Article33. Park MH, Choi EH, Choi KS. A study on health knowledge, health promoting behavior and needs for healthcare service in the elderly in a rural area. Journal of East-West Nursing Research. 2015; 21(1):18–27.34. Goldman SE, Stone KL, Ancoli-Israel S, Blackwell T, Ewing SK, Boudreau R, et al. Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep. 2007; 30(10):1317–1324. DOI: 10.1093/sleep/30.10.1317.
Article35. Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, et al. Short sleep duration as a risk factor for hypertension: analyses of the first national health and nutrition examination survey. Hypertension. 2006; 47(5):833–839.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis and Evaluation of the Theory of Unpleasant Symptoms
- Insomnia in Inpatients during Rehabilitation Treatment
- Relationships among Mood Status, Social Support, Symptom Experience and Quality of Life in Colorectal Cancer Patients - based on the Theory of Unpleasant Symptoms
- Self-care in Patients with Atrial Fibrillation Based on the Theory of Unpleasant Symptoms
- Factors influencing the health-related quality of life in Korean menopausal women: a cross-sectional study based on the theory of unpleasant symptoms