Korean J Women Health Nurs.
2022 Jun;28(2):100-111. 10.4069/kjwhn.2022.05.29.
Factors influencing the health-related quality of life in Korean menopausal women: a cross-sectional study based on the theory of unpleasant symptoms
- Affiliations
-
- 1Department of Nursing, Pukyong National University, Busan, Korea
- KMID: 2535427
- DOI: http://doi.org/10.4069/kjwhn.2022.05.29
Abstract
- Purpose
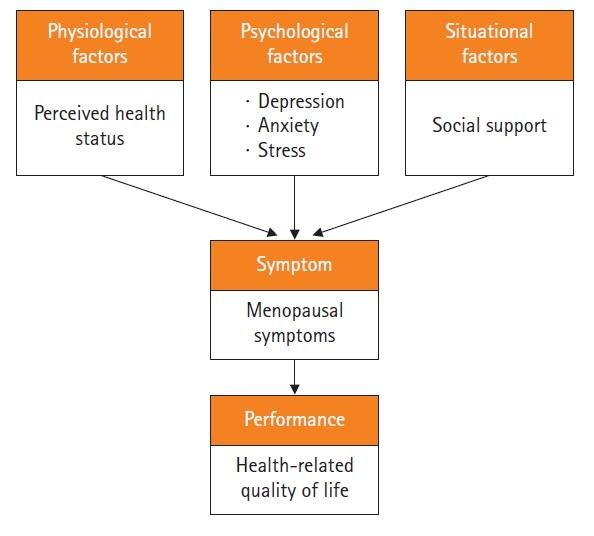
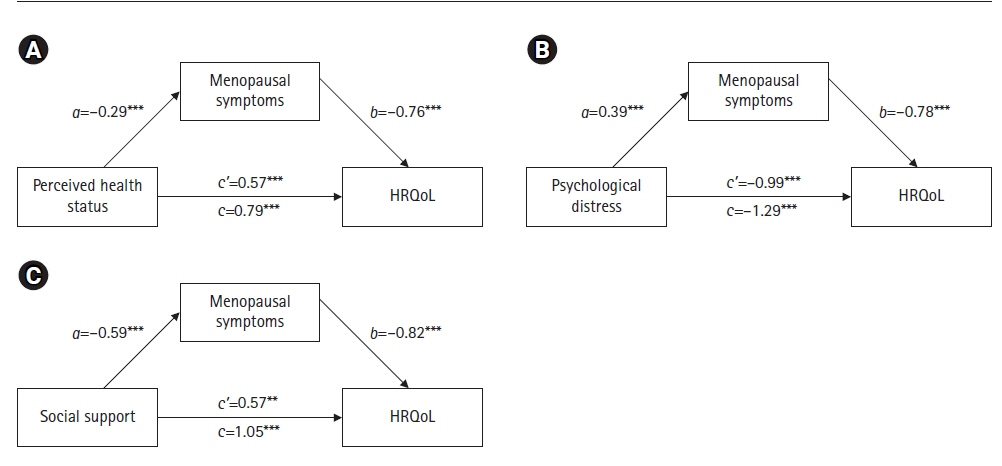
Based on the theory of unpleasant symptoms (TOUS), this study aimed to examine the direct effect of antecedent factors on health-related quality of life (HRQoL) and its indirect effect via symptoms in Korean women during the late menopausal transition (MT) and early postmenopause.
Methods
This cross-sectional survey employed a descriptive correlational research design. The respondents were 152 middle-aged women 40 to 60 years with an intermenstrual interval of 60 days or more (late MT) or less than 5 years from the last menstrual period (early postmenopause). The respondents were recruited through convenience sampling in Busan, Korea, from December 1, 2020, to January 31, 2021. Based on the TOUS, self-report data were collected on perceived health status, psychological distress, social support, menopausal symptoms, and HRQoL. The collected data were analyzed using descriptive statics, independent t-test, one-way analysis of variance, Pearson’s correlation coefficient, and the Hayes’ PROCESS macro.
Results
TOUS was supported on this sample (n=152) of Korean women during the late MT and early postmenopause. Perceived health status, psychological distress, and social support had significant direct relationships with HRQoL. Menopausal symptoms had significant indirect relationships between antecedent factors (perceived health status, psychological distress, and social support) and partially mediated HRQoL.
Conclusion
The findings of this study indicate that menopausal symptoms play an important role as an intervening factor of HRQoL in women during the late MT and early postmenopause. Therefore, women need an integrated program that manages antecedent factors and menopausal symptoms to improve HRQoL in these menopausal stages.
Figure
Cited by 1 articles
-
Stepping stones for the future—2022 major developments, journal metrics, and appreciation for reviewers
Sue Kim
Korean J Women Health Nurs. 2022;28(4):265-268. doi: 10.4069/kjwhn.2022.12.14.1.
Reference
-
References
1. Clarfield AM. Healthy life expectancy is expanding. J Am Geriatr Soc. 2018; 66(1):200–201. https://doi.org/10.1111/jgs.15165.
Article2. Statistics Korea. Birth statistics in 2018 [Internet]. Daejeon: Author; 2018 [cited 2021 Feb 9]. Available from: https://kostat.go.kr/portal/korea/kor_nw/1/6/9/index.board?bmode=read&bSeq=&aSeq=378711.3. Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017; 389(10076):1323–1335. https://doi.org/10.1016/S0140-6736(16)32381-9.
Article4. Stoker MJ, Dunbar GC, Beaumont G. The SmithKline Beecham ‘quality of life’ scale: a validation and reliability study in patients with affective disorder. Qual Life Res. 1992; 1(6):385–395. https://doi.org/10.1007/BF00704433.
Article5. Cho JH. Assessment of women’s health during menopausal periods. Cheongju, Korea: Korea Center for Disease Control and Prevention;2013. p. 170.6. Lee EJ. Factors influencing health-related quality of life in middle-aged women: the Sixth Korea National Health and Nutrition Examination Survey. Asia-Pacific J Multimed Serv Converg Art Humanit Soc. 2017; 7(2):659–670.
Article7. Sohn JN. Factors influencing depression in middle aged women: focused on quality of life on menopause. J Health Info Stat. 2018; 43(2):148–157. https://doi.org/10.21032/jhis.2018.43.2.148.
Article8. Kwag BG, Park JC, Lee W, Chang SH, Chun DH. The relationship between depression and health-related quality of life in Korean adult: using 2014 Korea National Health and Nutrition Examination Survey data. Korean J Fam Pract. 2018; 8(2):236–243. https://doi.org/10.21215/kjfp.2018.8.2.236.
Article9. Jung KH, Chun N. Influence of stress, social support and lifestyle on health-related quality of life in middle aged women. J Korean Biol Nurs Sci. 2019; 21(1):62–69. https://doi.org/10.7586/jkbns.2019.21.1.62.
Article10. Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012; 97(4):1159–1168. https://doi.org/10.1210/jc.2011-3362.
Article11. Lenz ER, Suppe F, Gift AG, Pugh LC, Milligan RA. Collaborative development of middle-range nursing theories: toward a theory of unpleasant symptoms. ANS Adv Nurs Sci. 1995; 17(3):1–13. https://doi.org/10.1097/00012272-199503000-00003.
Article12. Lenz ER, Pugh LC, Milligan RA, Gift A, Suppe F. The middle-range theory of unpleasant symptoms: an update. ANS Adv Nurs Sci. 1997; 19(3):14–27. https://doi.org/10.1097/00012272-199703000-00003.
Article13. Speake DL, Cowart ME, Pellet K. Health perceptions and lifestyles of the elderly. Res Nurs Health. 1989; 12(2):93–100. https://doi.org/10.1002/nur.4770120206.
Article14. Kweon YR, Jeon HO. Effects of perceived health status, self-esteem and family function on expectations regarding aging among middle-aged women. J Korean Acad Nurs. 2013; 43(2):176–184. https://doi.org/10.4040/jkan.2013.43.2.176.
Article15. Lee SI, Oh ET, Baek K. Effect of the subjective exercise ability and passion on exercise self-efficacy and perceived health in life sport participants. J Sport Leis Stud. 2011; 43(2):985–997. https://doi.org/10.51979/KSSLS.2011.02.43.985.
Article16. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995; 33(3):335–343. https://doi.org/10.1016/0005-7967(94)00075-u.
Article17. Cha ES, Park MY, Kim GA. A comparison analysis of somatotype, physical activity, mental health, healthy behavior between normal weight and overweight college students in Korea. Korean J Health Promot Dis Prev. 2008; 8(4):245–255.18. Park JW. A study to development a scale of social support [master’s thesis]. Seoul: Yonsei University;1985. 127.19. Heinemann LA, Potthoff P, Schneider HP. International versions of the Menopause Rating Scale (MRS). Health Qual Life Outcomes. 2003; 1:28. https://doi.org/10.1186/1477-7525-1-28.
Article20. Sun SK, Song HY, Kim JS, Min YK, Oh HJ, Lee JK. Decisional conflict about hormone replacement therapy in postmenopausal women and its related factors. J Korean Acad Fam Med. 2006; 27(8):629–636.21. Yoon JS, Kook SH, Lee MS. A preliminary study on Korean version of the SmithKline Beecham Quality of Life Scale (KvSBQOL). J Korean Neuropsychiatr Assoc. 1998; 37(2):280–294.22. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. 2nd ed. New York, NY: Guilford Press;2018. p. 692.23. Kim HS. Effect of pain, nutritional risk, loneliness, perceived health status on health-related quality of life in elderly women living alone. J Korea Converg Soc. 2017; 8(7):207–218. https://doi.org/10.15207/jkcs.2017.8.7.207.
Article24. Jung YO, Oh HS. The effects of social support, self-efficacy and perceived health status on aging anxiety of the middle-aged women. J Korean Pubilc Health Nurs. 2016; 30(1):30–41. https://doi.org/10.5932/JKPHN.2016.30.1.30.
Article25. Lee S, Son H, Lee D, Kang H. The influence of e-health literacy, subjective health status, and health information seeking behavior on the internet on health promoting behavior. J Wellness. 2017; 12(4):55–67. https://doi.org/10.21097/ksw.2017.11.12.4.55.
Article26. Felger JC. Imaging the role of inflammation in mood and anxiety-related disorders. Curr Neuropharmacol. 2018; 16(5):533–558. https://doi.org/10.2174/1570159X15666171123201142.
Article27. Kivimäki M, Steptoe A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol. 2018; 15(4):215–229. https://doi.org/10.1038/nrcardio.2017.189.
Article28. Park JM, Choi IR. The effect of K-MBSR program on stress, stress coping style, depression, anger and sleep of middle aged women. J Korean Acad Nurs. 2016; 46(2):194–206. https://doi.org/ 10.4040/jkan.2016.46.2.194.
Article29. Lee HS, Chong YS. The relationships between social support (giving and receiving) and subjective well-being in the elderly: mediating effects of basic psychological needs. Korean J Develop Psychol. 2020; 33(3):43–64. https://doi.org/10.35574/kjdp.2020.9.33.3.43.
Article30. Sim YS, Kim YM. The impact of volunteer activities on the cognitive health of middle-aged women in the digital transformation infrastructure. J Digit Converg. 2018; 16(8):11–18. https://doi.org/10.14400/jdc.2018.16.8.011.
Article31. Kim HY, Ko E. Factors influencing sexual function in postmenopausal married women. Korean J Women Health Nurs. 2016; 22(4):287–296. https://doi.org/10.4069/kjwhn.2016.22.4.287.
Article32. Kim JH, Oh PJ. Menopause symptoms and perceived cognitive decline in menopausal women: The mediating effect of health promotion behavior. Korean J Adult Nurs. 2017; 9(2):200–210. https://doi.org/10.7475/kjan.2017.29.2.200.
Article33. Health Insurance Review & Assessment Service. Disease subcategory (tier 3 morbidity) statistics [Internet]. Wonju, Korea: Author; c2015 [cited 2021 Aug 7]. Available from: https://opendata.hira.or.kr/op/opc/olap3thDsInfo.do.34. The NAMS 2017 Hormone Therapy Position Statement Advisory Panel. The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017; 24(7):728–753. https://doi.org/10.1097/GME.0000000000000921.
Article35. Shin H, Lee E. Factors influencing quality of life in post-menopausal women. Korean J Women Health Nurs. 2020; 26(4):336–345. https://doi.org/10.4069/kjwhn.2020.11.14.
Article36. Soh BP, Man RE, Tham YC, Febwick E, Yong TT, Wong TY, et al. Hormone replacement therapy (HRT): utilisation rates, determinants and impact on health-related quality of life in a multi-ethnic asian population. J Clin Diagn Res. 2020; 14(1):8–15. https://doi.org/10.7860/jcdr/2020/42545.13463.
Article37. Kim KR, Lee JS. The effect of combined exercise on bone mineral density, blood osteocalcin, and health-related fitness in postmenopausal women. J Sport Leis Stud. 2016; 64:887–896. https://doi.org/10.51979/kssls.2016.05.64.887.
Article38. Berin E, Hammar M, Lindblom H, Lindh-Åstrand L, Rubér M, Spetz Holm AC. Resistance training for hot flushes in postmenopausal women: a randomised controlled trial. Maturitas. 2019; 126:55–60. https://doi.org/10.1016/j.maturitas.2019.05.005.
Article39. Kim KH, Park SA. Horticultural therapy program for middle-aged women’s depression, anxiety, and self-identify. Complement Ther Med. 2018; 39:154–159. https://doi.org/10.1016/j.ctim.2018.06.008.
Article40. Kim HG, Lee YH, Koo CD, Yeon PS. The effect of emotional freedom technique (EFT) as forest therapy program on the menopause symptoms and the quality of life of the middle-aged women. J Korean Instit For Recreat. 2016; 20(3):83–95. https://doi.org/10.34272/forest.2016.20.3.008.
Article41. Seo HJ, Ryu EJ, Ham MY. Relationships among mood status, social support, symptom experience and quality of life in colorectal cancer patients-based on the theory of unpleasant symptoms. Asian Oncol Nurs. 2018; 18(2):104–113. https://doi.org/10.5388/aon.2018.18.2.104.
Article42. Han EK, Kim SA, Yoon IY. Factors influencing functional health of patients with chronic insomnia based on theory of unpleasant symptoms. Korean J Adult Nurs. 2019; 31(2):165–175. https://doi.org/10.7475/kjan.2019.31.2.165.
Article43. Bridgland VM, Moeck EK, Green DM, Swain TL, Nayda DM, Matson LA, et al. Why the COVID-19 pandemic is a traumatic stressor. PLoS One. 2021; 16(1):e0240146. https://doi.org/ 10.1371/journal.pone.0240146.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors influencing quality of life in post-menopausal women
- Influencing Factors on Health-related Quality of Life among Japanese Middle-aged Marriage-based Immigrant Women in South Korea: A Cross-Sectional Study
- Comparison of quality of life and related factors according to premature menopause using the Korea National Health and Nutrition Examination Survey (2014-2017)
- Factors of Intention to take Hormone Replacement Therapy in Korean Menopausal Women
- Analysis and Evaluation of the Theory of Unpleasant Symptoms