J Korean Ophthalmol Soc.
2019 Apr;60(4):399-405. 10.3341/jkos.2019.60.4.399.
A Report of Two Case of Ocular Toxicity Resulting from Direct or Indirect Bee Venom
- Affiliations
-
- 1Department of Ophthalmology, Dankook University College of Medicine, Cheonan, Korea. mailcarr@naver.com
- KMID: 2443159
- DOI: http://doi.org/10.3341/jkos.2019.60.4.399
Abstract
- PURPOSE
To report a patient stung by a bee, who was diagnosed with sterile endopthalmitis and another patient diagnosed with optic neuritis, with decreasing visual acuity, after refined bee venom injection around the orbital tissue.
CASE SUMMARY
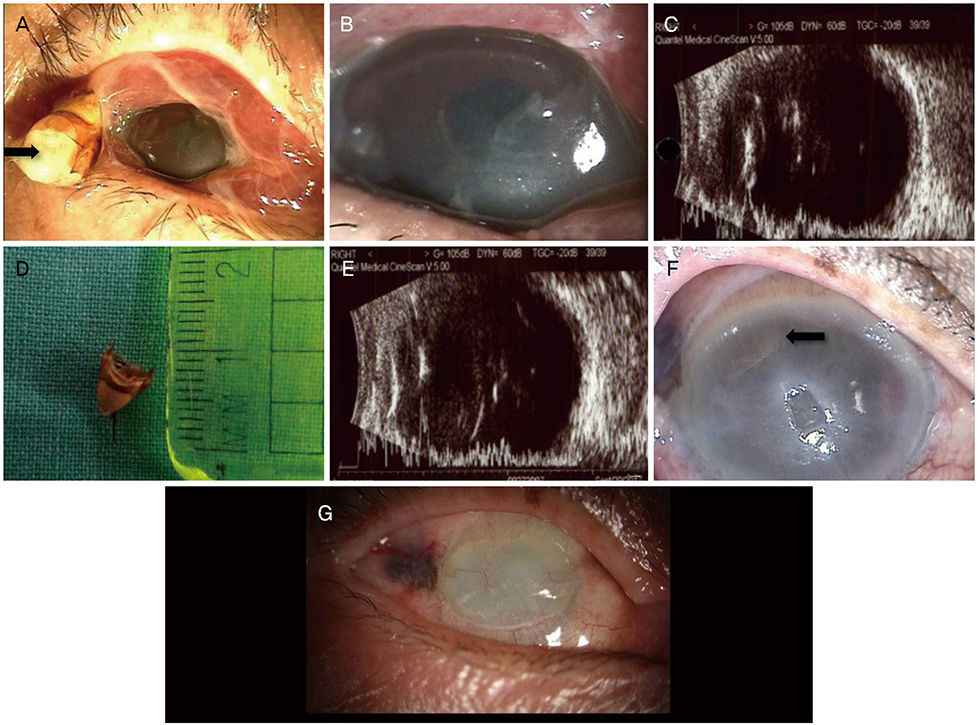
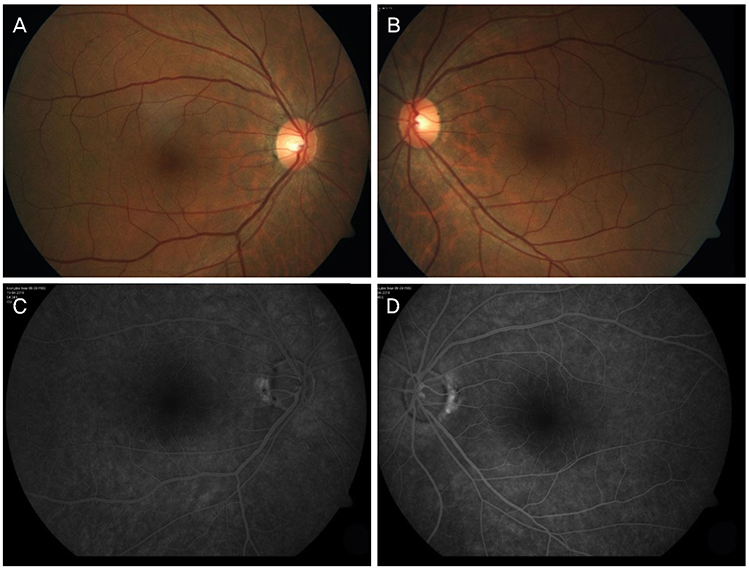
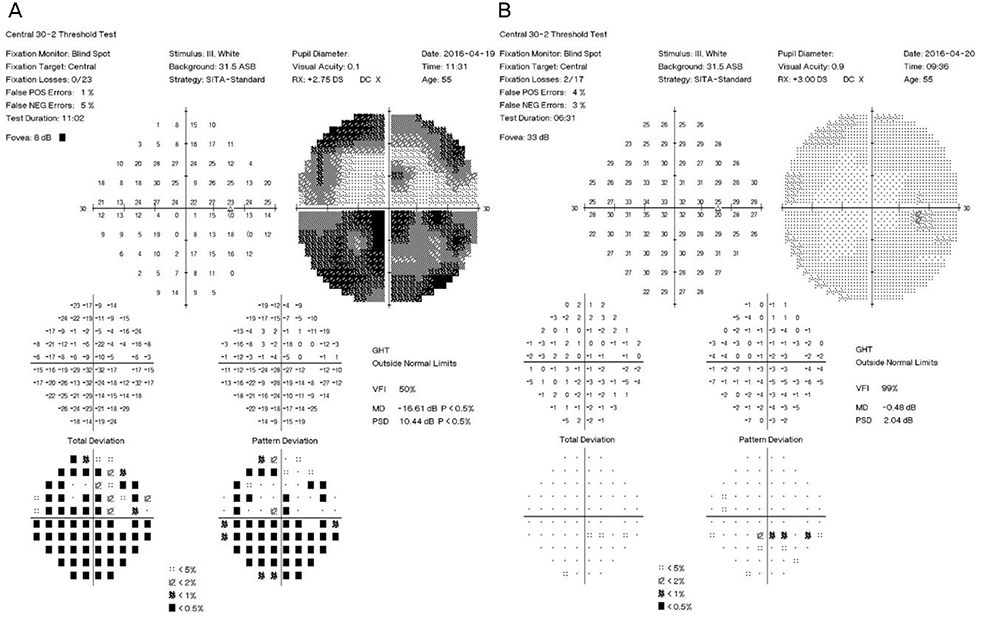
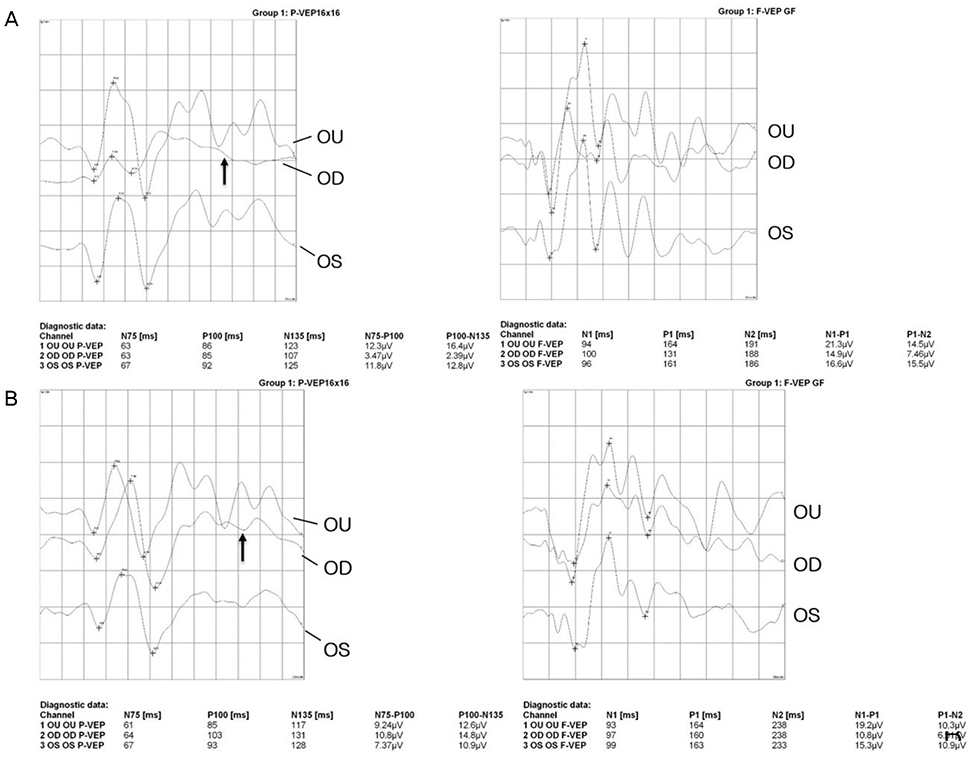
A 82-year-old female visited our hospital for decreased visual acuity in the right eye and ocular pain due to a bee sting. The bee sting penetrated the sclera into the vitreous. In the anterior segment, severe cornea edema and anterior chamber cells were seen. Using ultrasonography, inflammation was seen around the intravitreal area. After 3 months, intravitreal inflammation regressed but the patient's visual acuity was light perception negative, and corneal opacity, neovascularization, and phthisis bulbi were detected. A 55-year-old male visited our hospital for ocular pain in the right eye and decreasing visual acuity after refined bee venom injection around the orbital tissue. The best-corrected visual acuity in the right eye was 15/100, there was moderate injection on the conjunctiva. A relative afferent pupillary defect, abnormal color vision test results, and a defect in the visual field test were observed. There was no pain during external ocular movement, and other general blood tests, and a brain MRI were normal. Based on these symptoms, methylprednisolone megatherapy was started for treatment of optic neuritis. After treatment, visual acuity of the right eye was 9/10 and all other clinical optic neuritis symptoms regressed.
CONCLUSIONS
Based on these two cases, ocular toxicity from bee venom could result from both direct and indirect courses. Treatment using refined bee venom might be harmful, and caution is recommended in its use.
Keyword
MeSH Terms
-
Aged, 80 and over
Anterior Chamber
Bee Venoms
Bees*
Bites and Stings
Brain
Color Vision
Conjunctiva
Cornea
Corneal Opacity
Edema
Female
Hematologic Tests
Humans
Inflammation
Magnetic Resonance Imaging
Male
Methylprednisolone
Middle Aged
Optic Neuritis
Orbit
Pupil Disorders
Sclera
Ultrasonography
Visual Acuity
Visual Field Tests
Bee Venoms
Methylprednisolone
Figure
Reference
-
1. Vetter RS, Visscher PK, Camazine S. Mass envenomations by honey bees and wasps. West J Med. 1999; 170:223–227.2. Kim HJ, Shin JH, Moon SW. Prognosis of ocular injury caused by wasp sting: case reports. J Korean Ophthalmol Soc. 2016; 57:1981–1986.
Article3. Banks BE, Shipolini RA. Chemistry and pharmacology of honey-bee venom. In : Piek T, editor. Venoms of the hymenoptera: Biochemical, pharmacological and behavioural aspects. 1986. p. 329–416.4. Kavoussi B, Ross BE. The neuroimmune basis of anti-inflammatory acupuncture. Integr Cancer Ther. 2007; 6:251–257.
Article5. Bäcker M, Grossman P, Schneider J, et al. Acupuncture in migraine: investigation of autonomic effects. Clin J Pain. 2008; 24:106–115.6. Uchida S, Hotta H. Acupuncture affects regional blood flow in various organs. Evid Based Complement Alternat Med. 2008; 5:145–151.
Article7. Chen CJ, Richardson CD. Bee sting-induced ocular change. Ann Ophthalmol. 1986; 18:285–286.8. Lin PH, Wang NK, Hwang YS, et al. Bee Sting of the cornea and conjunctiva: management and outcomes. Cornea. 2011; 30:392–394.
Article9. King TP, Spangfort MD. Structure and biology of stinging insect venom allergens. Int Arch Allergy Immunol. 2000; 123:99–106.
Article10. Song HS, Wray SH. Bee sting optic neuritis. A case report with visual evoked potentials. J Clin Neuroophthalmol. 1991; 11:45–49.11. Koburova KL, Michailova SG, Shkenderov SV. Further investigation on the antiinflammatory properties of adolapin--bee venom polypeptide. Acta Physiol Pharmacol Bulg. 1985; 11:50–55.12. Smolin G, Wong I. Bee sting of the cornea: case report. Ann Ophthalmol. 1982; 14:342–343.13. Sharma P, Sharma R. Toxic optic neuropathy. Indian J Ophthalmol. 2011; 59:137–141.
Article14. Kerrison JB. Optic neuropathies caused by toxins and adverse drug reactions. Ophthalmol Clin North Am. 2004; 17:481–488.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Newly Developed Pemphigus Foliaceus and Possible Association with Alternative Bee-Venom Therapy
- Bee Venom Therapy for Musculoskeletal Disorders
- A Case of Ischemic Stroke Following Bee Venom Acupuncture
- A Case of Delayed Type Skin Reaction Induced by Bee Venom Acupuncture
- A Case of Steven-Johnson Syndrome after Live Bee Acupuncture (Bong-Chim)