Dement Neurocogn Disord.
2018 Mar;17(1):11-22. 10.12779/dnd.2018.17.1.11.
Re-standardization of the Korean- Instrumental Activities of Daily Living (K-IADL): Clinical Usefulness for Various Neurodegenerative Diseases
- Affiliations
-
- 1Department of Neurology, Samsung Medical Center, Seoul, Korea.
- 2Department of Neurology, Hallym University Sacred Heart Hospital, Anyang, Korea. ykang@hallym.ac.kr
- 3Department of Neurology, Yonsei University Health System, Seoul, Korea.
- 4Department of Neurology, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- 5The BOM Brain Health Neuropsychology Center and Cognitive Rehabilitation Research Institute, Seoul, Korea.
- 6Cognitive Neuroscience Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- 7Department of Neurology, Konkuk University Medical Center, Seoul, Korea.
- 8Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 9Human Brain Research & Consulting, Seoul, Korea.
- 10Department of Psychology, Hallym University, Chuncheon, Korea.
- KMID: 2442813
- DOI: http://doi.org/10.12779/dnd.2018.17.1.11
Abstract
- BACKGROUND AND PURPOSE
Evaluating instrumental activities of daily living (IADL) is an important part of procedure to diagnose dementia. The Korean-Instrumental Activities of Daily Living (K-IADL) has been used extensively in Korea. However, its cut-off score has not been reformulated since 2002. The purpose of this study was to yield a new optimal cut-off score for the K-IADL and confirm the validity of this new cut-off score with various dementia groups.
METHODS
We retrospectively collected a total of 2,347 patients' K-IADL data from 6 general hospitals in Korea. These patients had mild cognitive impairment (MCI) or dementia with various etiologies for cognitive impairment. We also recruited a normal control group (n=254) from the community. Korean-Mini Mental State Examination, Short version of the Geriatric Depression Scale, Clinical Dementia Rating, and Global Deterioration Scale were administered to all participants. Caregivers completed K-IADL and Barthel Index.
RESULTS
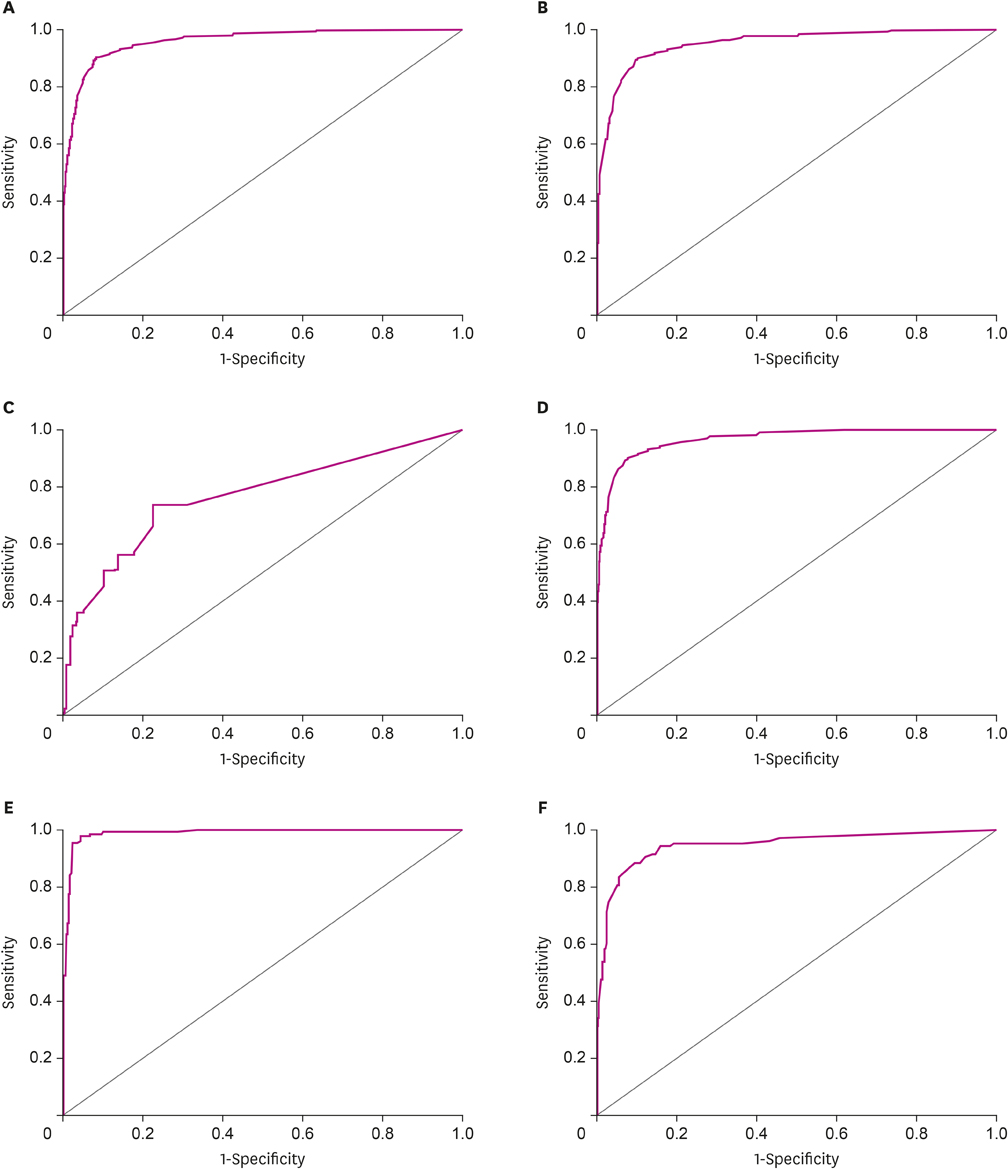
K-IADL scores were significantly different among dementia subgroups, but not significantly different among MCI subgroups. Based on internal consistency, correlations with other scales, and factor analysis, K-IADL showed excellent reliability and validity. The new optimal cut-off score to diagnose dementia was 0.40, which gave a sensitivity of 0.901 and a specificity of 0.916. Positive predictive value for dementia using the new cut-off score was 94.2% for Alzheimer's disease, 100% for vascular dementia, and 84% for Parkinson's disease.
CONCLUSIONS
Our results illustrate that the new K-IADL cut-off score of 0.40 is reliable and valid for screening impairments of daily functioning resulting from various etiologies.
MeSH Terms
Figure
Cited by 2 articles
-
Validation of the Korean-Everyday Cognition (K-ECog)
Minji Song, Sun Hwa Lee, Seungmin Jahng, Seong Yoon Kim, Yeonwook Kang
J Korean Med Sci. 2019;34(9):. doi: 10.3346/jkms.2019.34.e67.Validation of the Short Form of Korean-Everyday Cognition (K-ECog)
Minji Song, Dong Gi Seo, Seong Yoon Kim, Yeonwook Kang
J Korean Med Sci. 2023;38(44):e370. doi: 10.3346/jkms.2023.38.e370.
Reference
-
1. Cumming JL, Benson DF. Dementia: a Clinical Approach. 2nd ed. Boston, MA: Butterworth-Heinemann;1992.2. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology. 1984; 34:939–944.
Article3. Hindmarch I, Lehfeld H, de Jongh P, Erzigkeit H. The Bayer activities of daily living scale (B-ADL). Dement Geriatr Cogn Disord. 1998; 9:Suppl 2. 20–26.
Article4. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969; 9:179–186.
Article5. McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011; 7:263–269.
Article6. Lee HW, Kang SJ, Choi SH. Assessment of activities of daily living and abnormal behavior. Korean Dementia Association. Dementia: Clinical Approach. 2nd ed. Anyang: Academia;2011. p. 125–143.7. Kang SJ, Choi SH, Lee BH, Kwon JC, Na DL, Han SH, et al. The reliability and validity of the Korean Instrumental Activities of Daily Living (K-IADL). J Korean Neurol Assoc. 2002; 20:8–14.8. Choi SH, Na DL, Lee BH, Kang SJ, Ha CK, Han SH, et al. Validation of the Korean version of the Bayer activities of daily living scale. Hum Psychopharmacol. 2003; 18:469–475.
Article9. Suh GH. Development of the Korean version of Disability Assessment for Dementia Scale (DAD-K) to assess function in dementia. J Korean Geriatr Soc. 2003; 7:278–287.10. Ku HM, Kim JH, Kwon EJ, Kim SH, Lee HS, Ko HJ, et al. A study on the reliability and validity of Seoul-Instrumental Activities of Daily Living (S-IADL). J Korean Neuropsychiatr Assoc. 2004; 43:189–199.11. Won CW, Rho YG. SunWoo D, Lee YS. The validity and reliability of Korean Instrumental Activities of Daily Living (K-IADL) Scale. J Korean Geriatr Soc. 2002; 6:273–280.12. Kang Y, Jahng S, Na DL. Seoul Neuropsychological Screening Battery II. Seoul: Human Brain Research & Consulting Co.;2012.13. Christensen KJ, Multhaup KS, Nordstrom S, Voss K. A cognitive battery for dementia: development and measurement characteristics. Psychol Assess. 1991; 3:168–174.
Article14. Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004; 256:183–194.
Article15. Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:2672–2713.
Article16. Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992; 55:181–184.
Article17. Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord. 2007; 22:1689–1707.
Article18. Kang Y. A normative study of the Korean-Mini Mental State Examination (K-MMSE) in the elderly. Korean J Psychol Gen. 2006; 25:1–12.19. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993; 43:2412–2414.20. Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982; 139:1136–1139.
Article21. Cho MJ, Bae JN, Suh GH, Hahm BJ, Kim JK, Lee DW, et al. Validation of Geriatric Depression Scale, Korean version (GDS) in the assessment of DSM-III-R major depression. J Korean Neuropsychiatr Assoc. 1999; 38:48–63.22. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index: a simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md State Med J. 1965; 14:61–65.23. Cheon SM, Park KW, Kim JW. Identification of daily activity impairments in the diagnosis of Parkinson disease dementia. Cogn Behav Neurol. 2015; 28:220–228.
Article24. Aretouli E, Brandt J. Everyday functioning in mild cognitive impairment and its relationship with executive cognition. Int J Geriatr Psychiatry. 2010; 25:224–233.
Article25. Gold DA. An examination of instrumental activities of daily living assessment in older adults and mild cognitive impairment. J Clin Exp Neuropsychol. 2012; 34:11–34.
Article26. Perneczky R, Pohl C, Sorg C, Hartmann J, Tosic N, Grimmer T, et al. Impairment of activities of daily living requiring memory or complex reasoning as part of the MCI syndrome. Int J Geriatr Psychiatry. 2006; 21:158–162.
Article27. Pedrosa H, De Sa A, Guerreiro M, Maroco J, Simoes MR, Galasko D, et al. Functional evaluation distinguishes MCI patients from healthy elderly people--the ADCS/MCI/ADL scale. J Nutr Health Aging. 2010; 14:703–709.
Article28. Jekel K, Damian M, Wattmo C, Hausner L, Bullock R, Connelly PJ, et al. Mild cognitive impairment and deficits in instrumental activities of daily living: a systematic review. Alzheimers Res Ther. 2015; 7:17.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness of Cognitive Training to Instrumental Activities of Daily Living in Community-Dwelling Elderly
- The Validity and Reliability of Korean Instrumental Activities of Daily Living(K-IADL) Scale
- Factors Affecting the Instrumental Activities of Daily Living of Elderly People with Mild Cognitive Impairment and Mild Dementia
- Why Do Older Korean Adults Respond Differently to Activities of Daily Living and Instrumental Activities of Daily Living? A Differential Item Functioning Analysis
- Impairment of Instrumental Activities of Daily Living in Patients with Mild Cognitive Impairment