J Cardiovasc Imaging.
2019 Apr;27(2):137-146. 10.4250/jcvi.2019.27.e22.
Evaluation of Left Atrial Electromechanical Delay and Left Atrial Phasic Functions in Surgical Early Menopause Patients
- Affiliations
-
- 1Department of Cardiology, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey. drmuratakcay@hotmail.com
- 2Clinic of Cardiology, Giresun Bulancak State Hospital, Giresun, Turkey.
- 3Department of Obstetrics and Gynecology, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey.
- KMID: 2442748
- DOI: http://doi.org/10.4250/jcvi.2019.27.e22
Abstract
- BACKGROUND
This study evaluated the atrial electromechanical delay (AEMD) and the left atrial (LA) mechanical functions in patients with surgical early menopause.
METHODS
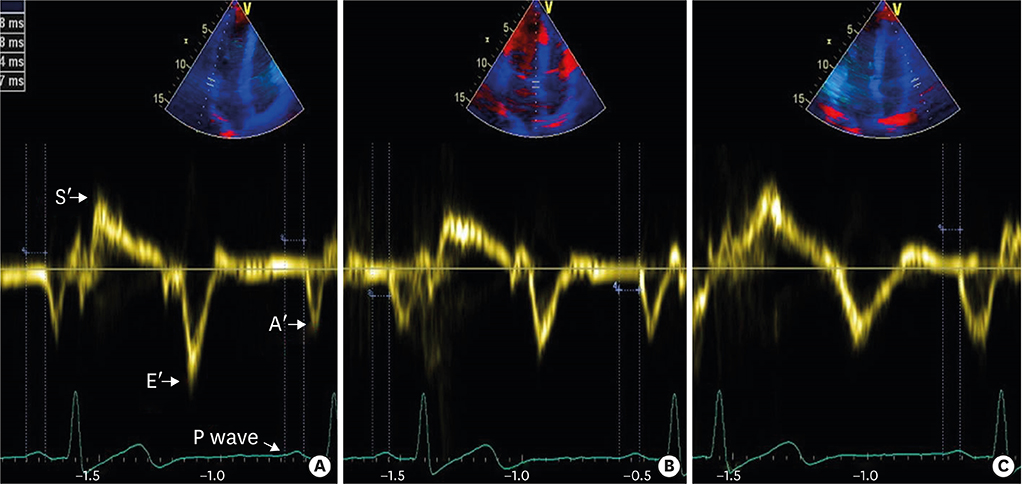
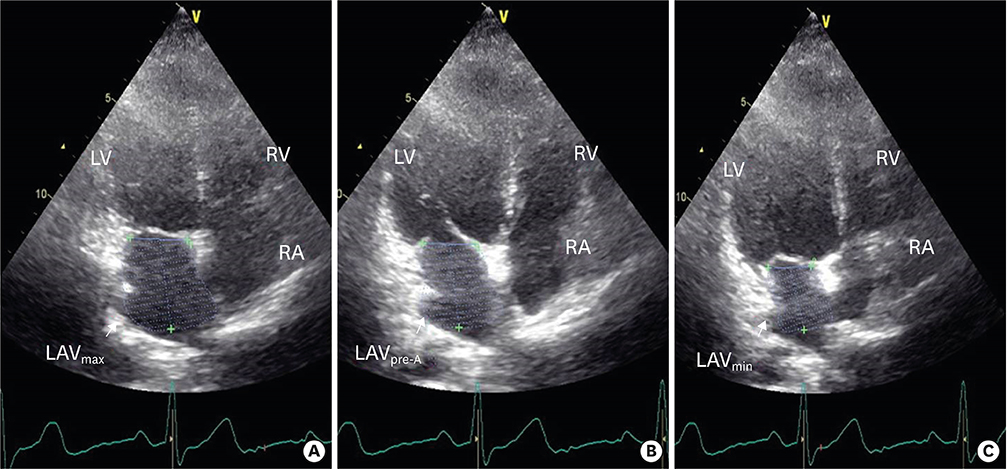
A total of 62 patients were included in the study: 33 patients with surgical early menopause and 29 age- and sex-matched healthy controls. The duration distance from the start of the P wave to the beginning of the A wave for the lateral mitral annulus, septal mitral annulus, and lateral tricuspid annulus was assessed by tissue Doppler echocardiography. The differences in these durations were used to calculate the inter- and intra-atrial mechanical delays. LA volumes were evaluated using the biplane area-length technique, and LA mechanical function values were measured.
RESULTS
The baseline laboratory and clinical characteristics were similar between the two groups. Surgical early menopause patients displayed increased static atrial electromechanical connection (PA"²) times for the septal mitral annulus and lateral tricuspid annulus compared to the controls. However, the lateral mitral annulus, the inter-atrial, the intra-LA, and the right atrial EMD PA"² times were not significantly altered in surgical early menopause patients compared to controls. Importantly, the LA volume index (28.1 ± 8.17 vs. 24.89 ± 7.96 mL/m², p = 0.019), the maximal LA volume (49.6 ± 14.1 vs. 42.9 ± 16.1 mL, p = 0.004), the minimal LA volume (18.4 ± 7.0 vs. 15.2 ± 9.0 mL, p = 0.022), and the atrial precontraction LA volume (31.0 ± 10.9 vs. 24.9 ± 10.1 mL, p = 0.006) were higher in the patients with surgical early menopause compared to the controls. The LA reservoir, conduit and pumping functions and the total, passive, and active emptying volumes were all comparable between the two groups (p = 0.09; 0.06; 0.68; 0.06; 0.48; 0.07, respectively).
CONCLUSIONS
Patients with surgical early menopause demonstrated impaired atrial electrical delay and electromechanical functions.
Figure
Cited by 1 articles
-
Searching for Risk of Atrial Fibrillation in Surgical Early Menopause: Assessment of the Electromechanical Property and Function of the Left Atrium
Ran Heo
J Cardiovasc Imaging. 2019;27(2):147-149. doi: 10.4250/jcvi.2019.27.e25.
Reference
-
1. Siniscalchi M, De Franciscis P, Palomba S, et al. Effects of surgical menopause and estrogen replacement therapy on atrio-ventricular conduction and ventricular repolarization. Maturitas. 2001; 40:47–51.
Article2. Cabrera-Rego JO, Navarro-Despaigne D, Staroushik-Morel L, Díaz-Reyes K, Lima-Martínez MM, Iacobellis G. Association between endothelial dysfunction, epicardial fat and subclinical atherosclerosis during menopause. Clin Investig Arterioscler. 2018; 30:21–27.
Article3. Sari N, Engin-Üstün Y, Kiyak Çağlayan E, Göçmen AY, Polat MF. Evaluation of cardiovascular disease risk in women with surgically induced menopause. Gynecol Endocrinol. 2016; 32:498–501.
Article4. Blume GG, Mcleod CJ, Barnes ME, et al. Left atrial function: physiology, assessment, and clinical implications. Eur J Echocardiogr. 2011; 12:421–430.
Article5. Akıl MA, Akıl E, Bilik MZ, et al. The relationship between atrial electromechanical delay and left atrial mechanical function in stroke patients. Anatol J Cardiol. 2015; 15:565–570.
Article6. Wong JA, Rexrode KM, Sandhu RK, Moorthy MV, Conen D, Albert CM. Menopausal age, postmenopausal hormone therapy and incident atrial fibrillation. Heart. 2017; 103:1954–1961.
Article7. Deniz A, Sahiner L, Aytemir K, et al. Tissue Doppler echocardiography can be a useful technique to evaluate atrial conduction time. Cardiol J. 2012; 19:487–493.
Article8. Deniz A, Yavuz B, Aytemir K, et al. Intra-left atrial mechanical delay detected by tissue Doppler echocardiography can be a useful marker for paroxysmal atrial fibrillation. Echocardiography. 2009; 26:779–784.
Article9. Rein AJ, O'Donnell CP, Colan SD, Marx GR. Tissue velocity Doppler assessment of atrial and ventricular electromechanical coupling and atrioventricular time intervals in normal subjects. Am J Cardiol. 2003; 92:1347–1350.
Article10. Ozer N, Yavuz B, Can I, et al. Doppler tissue evaluation of intra-atrial and interatrial electromechanical delay and comparison with P-wave dispersion in patients with mitral stenosis. J Am Soc Echocardiogr. 2005; 18:945–948.11. Cui QQ, Zhang W, Wang H, et al. Assessment of atrial electromechanical coupling and influential factors in nonrheumatic paroxysmal atrial fibrillation. Clin Cardiol. 2008; 31:74–78.
Article12. Nar G, Ergul B, Aksan G, Inci S. Assessment of atrial electromechanical delay and left atrial mechanical functions in patients with ulcerative colitis. Echocardiography. 2016; 33:970–976.
Article13. Dogan U, Dogan NU, Basarir AO, et al. P-wave parameters and cardiac repolarization indices: does menopausal status matter? J Cardiol. 2012; 60:333–337.
Article14. Rocca WA, Gazzuola-Rocca L, Smith CY, et al. Accelerated accumulation of multimorbidity after bilateral oophorectomy: a population-based cohort study. Mayo Clin Proc. 2016; 91:1577–1589.
Article15. Magnani JW, Moser CB, Murabito JM, et al. Age of natural menopause and atrial fibrillation: the Framingham Heart Study. Am Heart J. 2012; 163:729–734.
Article16. Laughlin-Tommaso SK, Khan Z, Weaver AL, Smith CY, Rocca WA, Stewart EA. Cardiovascular and metabolic morbidity after hysterectomy with ovarian conservation: a cohort study. Menopause. 2018; 25:483–492.
Article17. Aktoz M, Yilmaztepe M, Tatli E, Turan FN, Umit EG, Altun A. Assessment of ventricular and left atrial mechanical functions, atrial electromechanical delay and P wave dispersion in patients with scleroderma. Cardiol J. 2011; 18:261–269.18. Karabag T, Aydin M, Dogan SM, et al. Investigation of the atrial electromechanical delay duration in Behcet patients by tissue Doppler echocardiography. Eur Heart J Cardiovasc Imaging. 2012; 13:251–256.
Article19. Taşolar H, Mete T, Ballı M, et al. Assessment of atrial electromechanical delay in patients with polycystic ovary syndrome in both lean and obese subjects. J Obstet Gynaecol Res. 2014; 40:1059–1066.
Article20. Yaman M, Arslan U, Beton O, Asarcıklı LD, Aksakal A, Dogdu O. Atrial electromechanical coupling in patients with lichen planus. Korean Circ J. 2016; 46:530–535.
Article21. Pinar M, Gulel O, Kucuksu Z, Meric M, Sahin M, Yilmaz O. Evaluation of biatrial size and functions by different echocardiographic parameters in patients with acute coronary syndromes. Int J Cardiovasc Imaging. 2013; 29:1725–1732.
Article22. Acar G, Sayarlioğlu M, Akçay A, et al. Evaluation of atrial electromechanical delay and left atrial mechanical functions in patients with rheumatoid arthritis. Turk Kardiyol Dern Ars. 2009; 37:447–453.23. Asinger RW. Role of transthoracic echocardiography in atrial fibrillation. Echocardiography. 2000; 17:357–364.
Article24. Aydin M, Özeren A, Bilge M, Dursun A, Cam F, Elbey MA. Effects of dipper and non-dipper status of essential hypertension on left atrial mechanical functions. Int J Cardiol. 2004; 96:419–424.
Article25. Choi JO, Han H, Cho SJ, et al. Reduced peak atrial systolic mitral annular velocity predicts the development of nonvalvular atrial fibrillation. Echocardiography. 2009; 26:645–650.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Searching for Risk of Atrial Fibrillation in Surgical Early Menopause: Assessment of the Electromechanical Property and Function of the Left Atrium
- Atrial conduction times and left atrial mechanical functions and their relation with diastolic function in prediabetic patients
- Plain chest PA evaluation of left atrial thrombosis in mitral valvular disease
- Atrial Electromechanical Coupling in Patients with Lichen Planus
- Atrial Rhythms in Patients with Left Atrial Isomerism