Korean J Ophthalmol.
2019 Apr;33(2):173-180. 10.3341/kjo.2018.0084.
Development of Optic Disc Torsion in Children
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea. twkim7@snu.ac.kr
- KMID: 2442622
- DOI: http://doi.org/10.3341/kjo.2018.0084
Abstract
- PURPOSE
To document the development of disc torsion.
METHODS
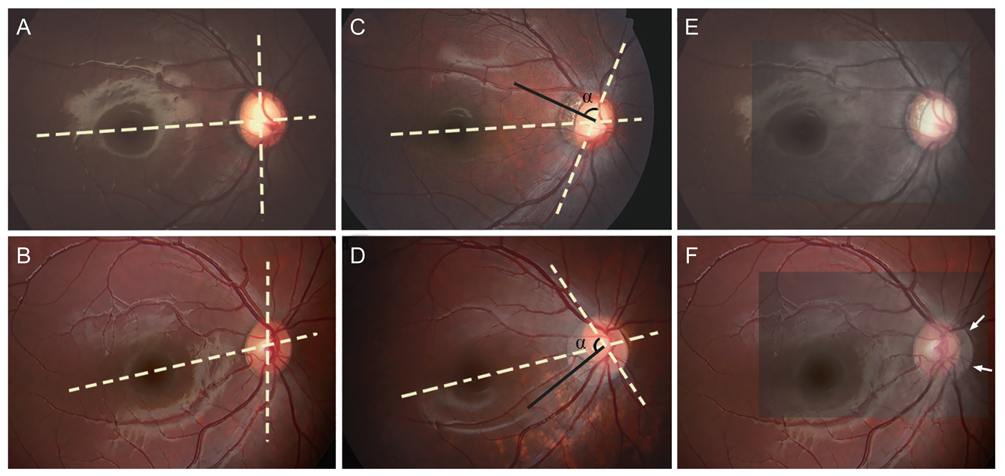
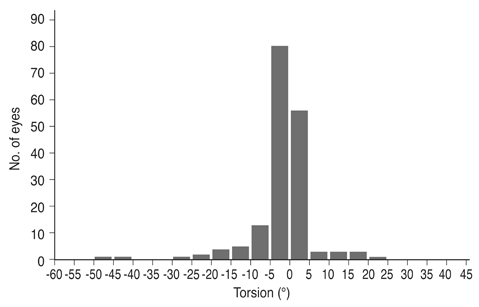
Consecutive disc photographs obtained at an interval of at least 1 year were reviewed retrospectively in 173 eyes of 173 Korean children. The angle of the vertical disc axis (AVDA) was measured in each fundus photograph with the fovea-disc center axis set at 0°. The associated change in the morphology of the optic disc was assessed by measuring the ratio of the horizontal to vertical disc diameters and the ratio of the maximum parapapillary atrophy width to vertical disc diameter. Eyes were divided into two groups with respect to the development of disc torsion: torsion and non-torsion group. Progressive torsion was defined as a change in AVDA between baseline and follow-up photographs beyond the coefficient of intraobserver repeatab ility. Factors associated with optic disc torsion were evaluated using logistic regression analysis.
RESULTS
Mean subject age and refractive error at the time of baseline fundus examination were 6.8 ± 1.7 (range, 2 to 11) years and 0.2 ± 2.6 (range, −6.0 to +5.5) diopters, respectively. Mean follow-up period was 44.8 ± 21.1 (range, 12 to 103) months. Forty-two eyes (24%) were classified as torsion group who showed changes in AVDA that were greater than the intraobserver measurement variability (4.5°) during the follow-up period. The development of optic disc torsion was associated with greater myopic shift, a decrease in horizontal to vertical disc diameters, and an increase in parapapillary atrophy width to vertical disc diameter.
CONCLUSIONS
Progressive optic disc torsion was a common phenomenon in the children included in this study. Torsion occurred as the result of optic disc tilt in an oblique axis in most cases. The findings provide a framework for understanding torsion-related glaucomatous optic nerve damage.
Keyword
MeSH Terms
Figure
Reference
-
1. Ito-Ohara M, Seko Y, Morita H, et al. Clinical course of newly developed or progressive patchy chorioretinal atrophy in pathological myopia. Ophthalmologica. 1998; 212:23–29.
Article2. Avila MP, Weiter JJ, Jalkh AE, et al. Natural history of choroidal neovascularization in degenerative myopia. Ophthalmology. 1984; 91:1573–1581.
Article3. Pierro L, Camesasca FI, Mischi M, Brancato R. Peripheral retinal changes and axial myopia. Retina. 1992; 12:12–17.
Article4. Suzuki Y, Iwase A, Araie M, et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology. 2006; 113:1613–1617.5. Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999; 106:2010–2015.6. Kempen JH, Mitchell P, Lee KE, et al. The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol. 2004; 122:495–505.7. Guo K, Yang DY, Wang Y, et al. Prevalence of myopia in schoolchildren in Ejina: the Gobi Desert Children Eye Study. Invest Ophthalmol Vis Sci. 2015; 56:1769–1774.
Article8. Williams KM, Verhoeven VJ, Cumberland P, et al. Prevalence of refractive error in Europe: the European Eye Epidemiology (E(3)) Consortium. Eur J Epidemiol. 2015; 30:305–315.
Article9. Saxena R, Vashist P, Tandon R, et al. Prevalence of myopia and its risk factors in urban school children in Delhi: the North India Myopia Study (NIM Study). PLoS One. 2015; 10:e0117349.
Article10. Foster PJ, Jiang Y. Epidemiology of myopia. Eye (Lond). 2014; 28:202–208.
Article11. Seet B, Wong TY, Tan DT, et al. Myopia in Singapore: taking a public health approach. Br J Ophthalmol. 2001; 85:521–526.
Article12. Cahane M, Bartov E. Axial length and scleral thickness effect on susceptibility to glaucomatous damage: a theoretical model implementing Laplace's law. Ophthalmic Res. 1992; 24:280–284.
Article13. Quigley HA. Reappraisal of the mechanisms of glaucomatous optic nerve damage. Eye (Lond). 1987; 1:318–322.
Article14. Ren R, Wang N, Li B, et al. Lamina cribrosa and peripapillary sclera histomorphometry in normal and advanced glaucomatous Chinese eyes with various axial length. Invest Ophthalmol Vis Sci. 2009; 50:2175–2184.
Article15. Park HY, Lee K, Park CK. Optic disc torsion direction predicts the location of glaucomatous damage in normal-tension glaucoma patients with myopia. Ophthalmology. 2012; 119:1844–1851.
Article16. Lee KS, Lee JR, Kook MS. Optic disc torsion presenting as unilateral glaucomatous-appearing visual field defect in young myopic Korean eyes. Ophthalmology. 2014; 121:1013–1019.
Article17. Lee KM, Lee EJ, Kim TW. Lamina cribrosa configuration in tilted optic discs with different tilt axes: a new hypothesis regarding optic disc tilt and torsion. Invest Ophthalmol Vis Sci. 2015; 56:2958–2967.
Article18. Witmer MT, Margo CE, Drucker M. Tilted optic disks. Surv Ophthalmol. 2010; 55:403–428.
Article19. How AC, Tan GS, Chan YH, et al. Population prevalence of tilted and torted optic discs among an adult Chinese population in Singapore: the Tanjong Pagar Study. Arch Ophthalmol. 2009; 127:894–899.20. Kim TW, Kim M, Weinreb RN, et al. Optic disc change with incipient myopia of childhood. Ophthalmology. 2012; 119:21–26.
Article21. Moriyama M, Ohno-Matsui K, Hayashi K, et al. Topographic analyses of shape of eyes with pathologic myopia by high-resolution three-dimensional magnetic resonance imaging. Ophthalmology. 2011; 118:1626–1637.
Article22. Dandona L, Quigley HA, Brown AE, Enger C. Quantitative regional structure of the normal human lamina cribrosa. A racial comparison. Arch Ophthalmol. 1990; 108:393–398.23. Doshi A, Kreidl KO, Lombardi L, et al. Nonprogressive glaucomatous cupping and visual field abnormalities in young Chinese males. Ophthalmology. 2007; 114:472–479.
Article24. Park HY, Lee KI, Lee K, et al. Torsion of the optic nerve head is a prominent feature of normal-tension glaucoma. Invest Ophthalmol Vis Sci. 2014; 56:156–163.
Article25. Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002; 120:701–713.26. Araie M, Shirato S, Yamazaki Y, et al. Risk factors for progression of normal-tension glaucoma under β-blocker monotherapy. Acta Ophthalmol. 2012; 90:e337–e343.
Article27. Lee JY, Sung KR, Han S, Na JH. Effect of myopia on the progression of primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2015; 56:1775–1781.
Article28. Hyman L, Gwiazda J, Hussein M, et al. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005; 123:977–987.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison between Optic Disc Torsion of Fellow Eyes in Unilateral Normal-tension Glaucoma and Normal Eyes
- The Effect of Optic Disc Size or Age on Evaluation of Optic Disc Parameters
- A Case of Optic Disc Pit
- Comparison of Optic Disc Appearance in Anterior ischemic optic neuropathy and Optic neuritis
- The Range of Ocular Torsion in Mass Screening