J Korean Soc Radiol.
2019 Mar;80(2):274-282. 10.3348/jksr.2019.80.2.274.
Pneumatosis Intestinalis Associated with Pulmonary Disorders
- Affiliations
-
- 1Department of Radiology, Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea. sinisim@ewha.ac.kr
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 2442518
- DOI: http://doi.org/10.3348/jksr.2019.80.2.274
Abstract
- PURPOSE
To determine the clinical features, imaging findings and possible causes of pneumatosis intestinalis (PI) in thoracic disorder patients.
MATERIALS AND METHODS
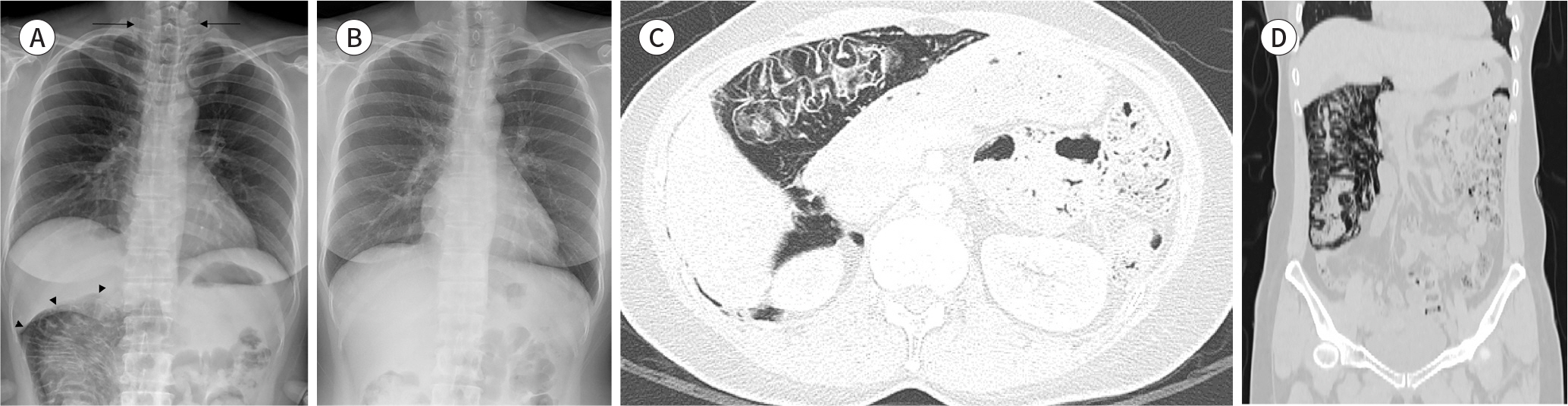
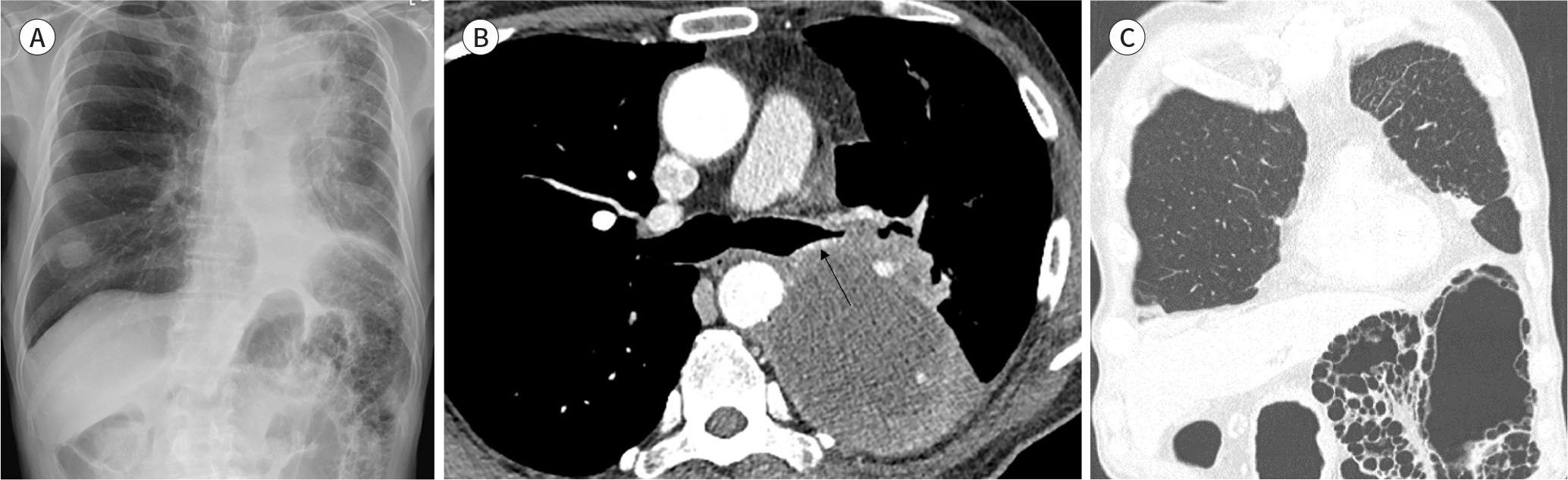
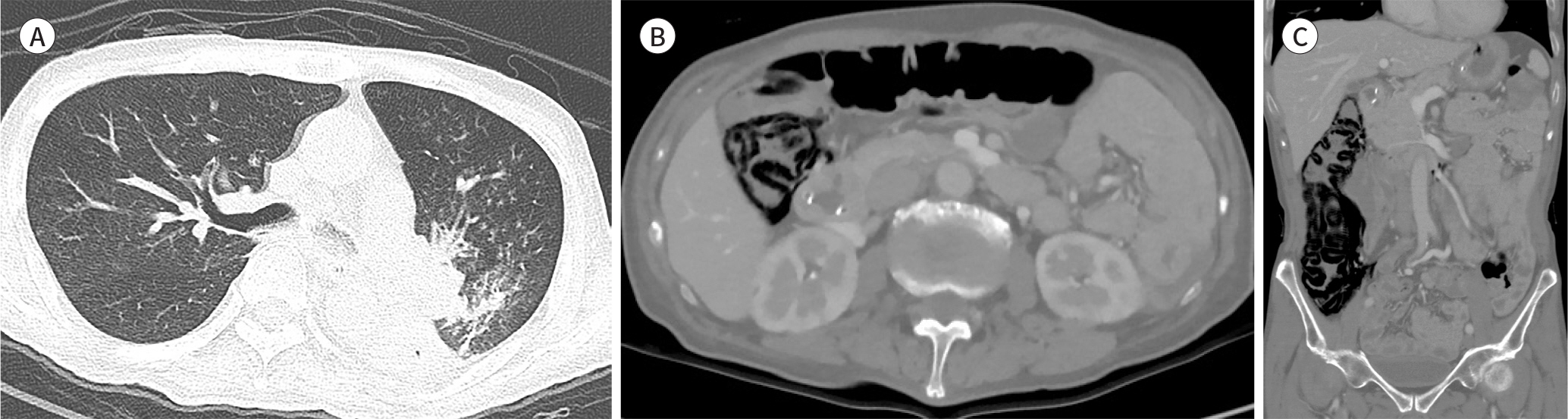
From 2005 to 2017, Among 62 PI patients, four of PI related with thoracic disease (6%) were identified. Medical records were reviewed to determine the clinical presentation, laboratory findings and treatment at the time of presentation of PI. Two experienced chest radiologists reviewed all imaging studies and recorded specific findings for each patient.
RESULTS
The causative thoracic diseases for each four patient were severe asthma, emphysema and airway obstruction. The imaging appearance of PI, including the involved bowel segment and pattern of the air, were divided into two mesenteric vascular territories; three of our cases showed linear pattern of PI located in the ascending & proximal transverse colon and the fourth case (lung cancer) had bubbly and cystic PI in the distal transverse and descending colon. All of the remaining 3 patients, except one patient who had not been followed up, improved within 1 month by conservative treatment.
CONCLUSION
Thoracic disorder with obstructive lung disease may result in the development of benign PI. Such PI in thoracic disease patients has a similar linear and cystic appearance with ischemic bowel disease, but can nevertheless be managed by conservative treatment.
MeSH Terms
Figure
Reference
-
References
1. Keene JG. Pneumatosis cystoides intestinalis and intramural intestinal gas.J Emerg Med. 1989; 7:645–650.2. Thompson WM, Ho L, Marroquin C. Pneumatosis intestinalis and pneumoperitoneum after bilateral lung transplantation in adults.AJR Am J Roentgenol. 2011; 196:W273–W279.3. Greenstein AJ, Nguyen SQ, Berlin A, Corona J, Lee J, Wong E, et al. Pneumatosis intestinalis in adults: management, surgical indications, and risk factors for mortality.J Gastrointest Surg. 2007; 11:1268–1274.4. Hawn MT, Canon CL, Lockhart ME, Gonzalez QH, Shore G, Bondora A, et al. Serum lactic acid determines the outcomes of CT diagnosis of pneumatosis of the gastrointestinal tract.Am Surg. 2004; 70:19–23. ; discussion 23–24.5. Doumit M, Saloojee N, Seppala R. Pneumatosis intestinalis in a patient with chronic bronchiectasis.Can J Gastroenterol. 2008; 22:847–850.6. Pear BL. Pneumatosis intestinalis: a review.Radiology. 1998; 207:13–19.7. Choi JY, Cho SB, Kim HH, Lee IH, Lee HY, Kang HS, et al. Pneumatosis intestinalis complicated by pneumoperitoneum in a patient with asthma.Tuberc Respir Dis (Seoul). 2014; 77:219–222.8. Ling FY, Zafar AM, Angel LF, Mumbower AL. Benign pneumatosis intestinalis after bilateral lung transplantation. BMJ Case Rep. 2015; 2015:bcr2015210701.
Article9. Faria LD, Anjos CH, Fernandes GD, Carvalho IF. Pneumatosis intestinalis after etoposide-based chemotherapy in a patient with metastatic small cell lung cancer: successful conservative management of a rare condition. Einstein (Sao Paulo). 2016; 14:420–422.
Article10. Iwasaku M, Yoshioka H, Korogi Y, Kunimasa K, Nishiyama A, Nagai H, et al. Pneumatosis cystoides intestinalis after gefitinib therapy for pulmonary adenocarcinoma.J Thorac Oncol. 2012; 7:257.11. Maeda A, Nakata M, Shimizu K, Yukawa T, Saisho S, Okita R. Pneumatosis intestinalis after gefitinib therapy for pulmonary adenocarcinoma: a case report. World J Surg Oncol. 2016; 14:175.
Article12. Hsueh KC, Tsou SS, Tan KT. Pneumatosis intestinalis and pneumoperitoneum on computed tomography: beware of non-therapeutic laparotomy. World J Gastrointest Surg. 2011; 3:86–88.
Article13. St Peter SD, Abbas MA, Kelly KA. The spectrum of pneumatosis intestinalis.Arch Surg. 2003; 138:68–75.14. Gagliardi G, Thompson IW, Hershman MJ, Forbes A, Hawley PR, Talbot IC. Pneumatosis coli: a proposed pathogenesis based on study of 25 cases and review of the literature. Int J Colorectal Dis. 1996; 11:111–118.
Article15. Ezuka A, Kawana K, Nagase H, Takahashi H, Nakajima A. Improvement of pneumatosis cystoides intestinalis after steroid tapering in a patient with bronchial asthma: a case report. J Med Case Rep. 2013; 7:163.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pneumatosis Cystoides Intestinalis in a Patient with Systemic Lupus Erythematosus
- A Case of Nonspecific Interstitial Pneumonia Complicated with Spontaneous Pneumomediastinum, Subcutaneous Emphysema and Pneumatosis Interstinalis
- A Case of Primary Pneumatosis Cystoides Intestinalis in a Patient with Chronic Abdominal Pain
- A Case of Recurrent Pneumatosis Cystoides Intestinalis Associated with Recurrent Pneumoperitoneum
- A case of pneumatosis cystoides intestinalis complicated by pneumoperitoneum in a post-tuberculosis destroyed lung