J Korean Soc Radiol.
2019 Jan;80(1):170-174. 10.3348/jksr.2019.80.1.170.
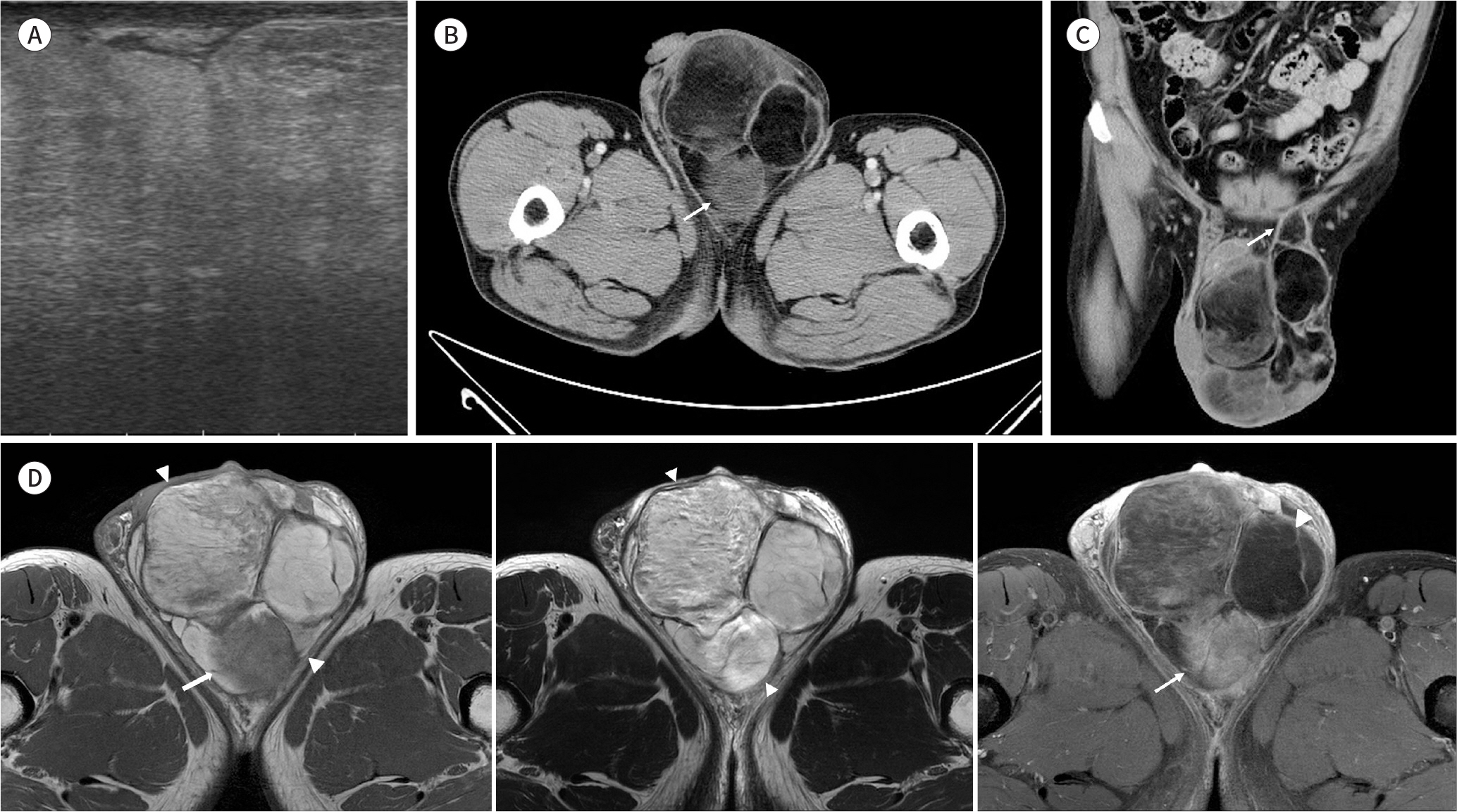
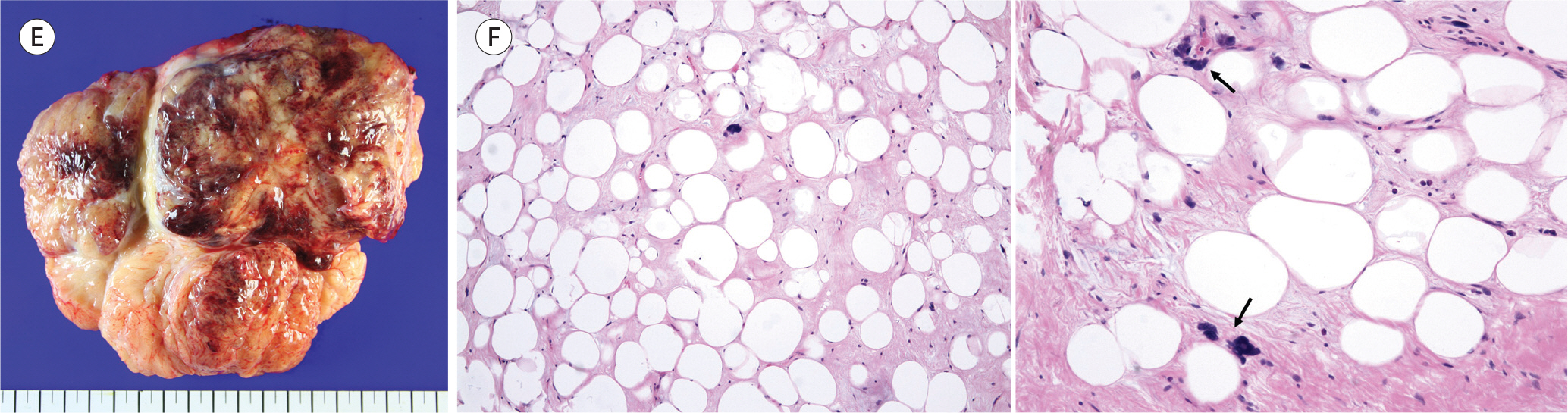
Imaging Findings of Scrotal Liposarcoma: A Case Report
- Affiliations
-
- 1Department of Radiology, Korea Cancer Center Hospital, Seoul, Korea. lcf0666@hanmail.net
- KMID: 2442479
- DOI: http://doi.org/10.3348/jksr.2019.80.1.170
Abstract
- Liposarcoma located in the scrotum is a very rare, and to our knowledge, only a few cases have been described in the radiologic literature. Clinically, scrotal liposarcoma manifests as a painless, slow-growing mass, which can be misdiagnosed as inguinal hernia, scrotal hydrocele or lipoma. Here, we present a case of scrotal liposarcoma. On CT and MRI, it manifested as a predominant fat-containing mass with heterogeneously enhancing soft tissue.
MeSH Terms
Figure
Reference
-
References
1. Beccia DJ, Krane RJ, Olsson CA. Clinical management of non-testicular intrascrotal tumors. J Urol. 1976; 116:476–479.
Article2. Wolfman DJ, Marko J, Gould CF, Sesterhenn IA, Lattin GE Jr. Mesenchymal extratesticular tumors and tumorlike conditions: from the radiologic pathology archives. Radiographics. 2015; 35:1943–1954.3. Enzinger FM, Weiss SW.Liposarcoma. In Enzinger FM, Weiss SW, eds. Soft Tissue Tumors. 3rd ed. St. Louis: Mosby;2006. p. 431–466.4. Patel NG, Rajagopalan A, Shrotri NS. Scrotal liposarcoma – a rare extratesticular tumour.JRSM Short Rep. 2011; 2:93.5. Woodward PJ, Schwab CM, Sesterhenn IA. From the archives of the AFIP: extratesticular scrotal masses: radiologic-pathologic correlation. Radiographics. 2003; 23:215–240.6. Alyousef H, Osman EM, Gomha MA. Paratesticular liposarcoma: a case report and review of the literature. Case Rep Urol. 2013; 2013:806289.
Article7. May M, Seehafer M, Helke C, Gunia S, Hoschke B. [Liposarcoma of the spermatic cord–report of one new case and review of the literature].Aktuelle Urol. 2004; 35:130–133.8. Cardenosa G, Papanicolaou N, Fung CY, Tung GA, Yoder IC, Althausen AF, et al. Spermatic cord sarcomas: sonographic and CT features. Urol Radiol. 1990; 12:163–167.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Myxoid Liposarcoma of Spermatic Cord Misdiagnosed for Hemangioma
- Paratesticular Liposarcoma with Atypical Image Findings: a Case Report
- Liposarcoma of Spermatic Cord: Report of A Case
- Recurrent Primary Pleomorphic Liposarcoma of the Breast: A Case Report with Imaging Findings
- The Magnetic Resonance (MR) Imaging Features of Myxoid Liposarcoma Arising from the Mesentery: a Case Report