Investig Magn Reson Imaging.
2017 Dec;21(4):252-258. 10.13104/imri.2017.21.4.252.
The Magnetic Resonance (MR) Imaging Features of Myxoid Liposarcoma Arising from the Mesentery: a Case Report
- Affiliations
-
- 1Department of Radiology, Wonkwang University Hospital, Iksan, Korea. yjyh@wku.ac.kr
- 2Imaging Science Research Center, Wonkwang University Hospital, Iksan, Korea.
- KMID: 2400379
- DOI: http://doi.org/10.13104/imri.2017.21.4.252
Abstract
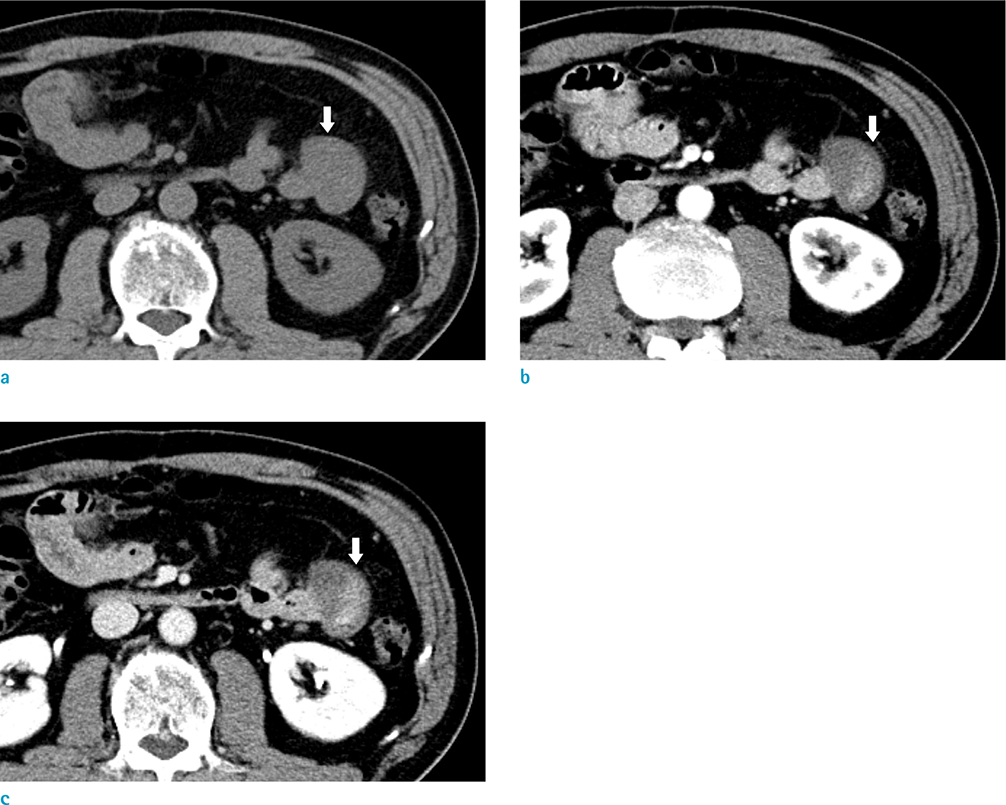
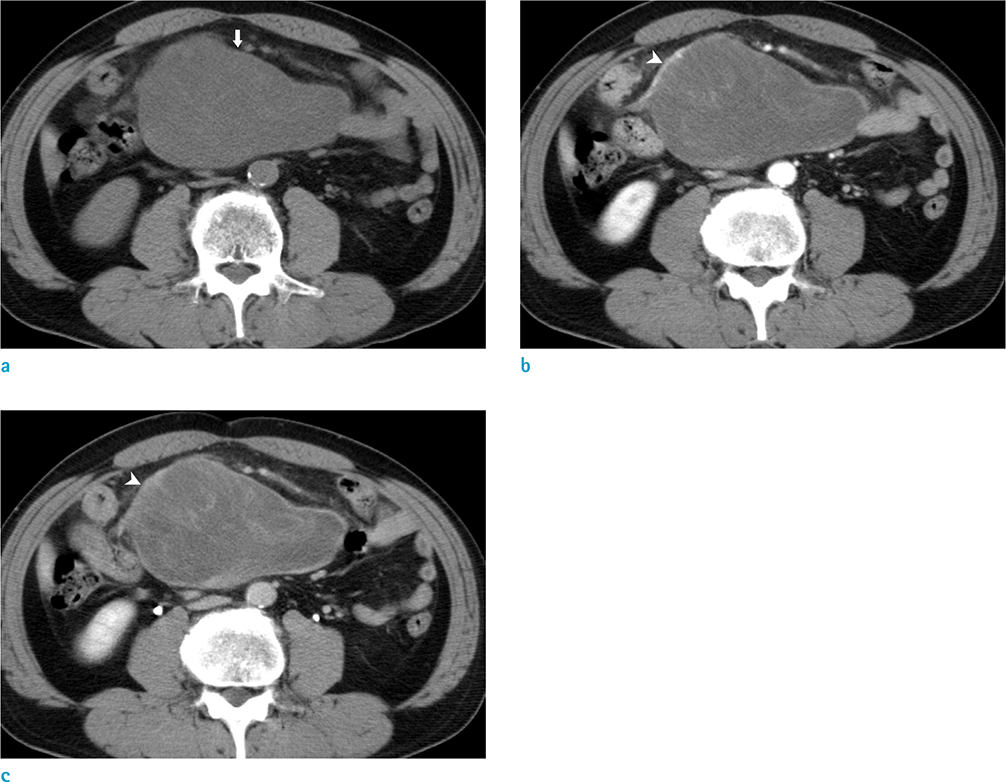
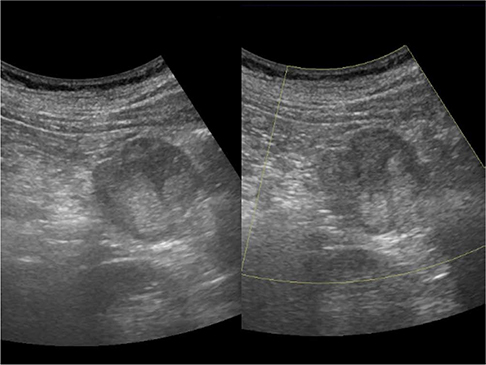
- Primary mesenteric liposarcoma is rare. It is difficult to make an accurate preoperative diagnosis of the myxoid type of liposarcoma by using imaging such as ultrasound or computed tomography (CT) due to the very small amount of fat that is located in the tumor. We report a case of primary myxoid liposarcoma of the mesentery which was difficult to differentiate from other solid mesenteric tumors with a myxoid component such as low grade fibromyxoid sarcoma, myxoid leiomyosarcoma or myxoma. Use of chemical shift magnetic resonance (MR) imaging to detect small fat components and its cystic appearance with solid components on the MR images can be useful to differentiate myxoid liposarcoma from the other mesenteric tumors with a myxoid component.
MeSH Terms
Figure
Reference
-
1. Fletcher CDM, Bridge JA, Hogendoorn P, Mertens F. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC;2013.2. Jain SK, Mitra A, Kaza RC, Malagi S. Primary mesenteric liposarcoma: an unusual presentation of a rare condition. J Gastrointest Oncol. 2012; 3:147–150.3. Dufay C, Abdelli A, Le Pennec V, Chiche L. Mesenteric tumors: diagnosis and treatment. J Visc Surg. 2012; 149:e239–e251.
Article4. Sung MS, Kang HS, Suh JS, et al. Myxoid liposarcoma: appearance at MR imaging with histologic correlation. Radiographics. 2000; 20:1007–1019.
Article5. Shin NY, Kim MJ, Chung JJ, Chung YE, Choi JY, Park YN. The differential imaging features of fat-containing tumors in the peritoneal cavity and retroperitoneum: the radiologic-pathologic correlation. Korean J Radiol. 2010; 11:333–345.
Article6. Murphey MD, Arcara LK, Fanburg-Smith J. From the archives of the AFIP: imaging of musculoskeletal liposarcoma with radiologic-pathologic correlation. Radiographics. 2005; 25:1371–1395.7. Alatise OI, Oke OA, Olaofe OO, Omoniyi-Esan GO, Adesunkanmi AR. A huge low-grade fibromyxoid sarcoma of small bowel mesentery simulating hyper immune splenomegaly syndrome: a case report and review of literature. Afr Health Sci. 2013; 13:736–740.
Article8. Petscavage-Thomas JM, Walker EA, Logie CI, Clarke LE, Duryea DM, Murphey MD. Soft-tissue myxomatous lesions: review of salient imaging features with pathologic comparison. Radiographics. 2014; 34:964–980.
Article9. Sheth S, Horton KM, Garland MR, Fishman EK. Mesenteric neoplasms: CT appearances of primary and secondary tumors and differential diagnosis. Radiographics. 2003; 23:457–473.
Article10. Ishiguro S, Yamamoto S, Chuman H, Moriya Y. A case of resected huge ileocolonic mesenteric liposarcoma which responded to pre-operative chemotherapy using doxorubicin, cisplatin and ifosfamide. Jpn J Clin Oncol. 2006; 36:735–738.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Liposarcoma Arising in the Mesentery
- Identification of Fat in Myxoid Matrix-Rich Mesenteric Lipoblastoma Using In-Phase and Opposed-Phase MRI: A Case Report
- Myxoid Liposarcoma of Spermatic Cord Misdiagnosed for Hemangioma
- Liposarcoma: MR Findings in the Histologic Subtypes
- Primary Multiple Mesenteric Liposarcoma of the Transverse Mesocolon