J Rheum Dis.
2019 Jan;26(1):74-78. 10.4078/jrd.2019.26.1.74.
Catastrophic Antiphospholipid Syndrome Associated with Systemic Lupus Erythematosus Successfully Treated with Rituximab: A Case Report
- Affiliations
-
- 1Department of Pediatrics, Hallym University Sacred Heart Hospital, Anyang, Korea. kwangnamkim@naver.com
- KMID: 2442037
- DOI: http://doi.org/10.4078/jrd.2019.26.1.74
Abstract
- The catastrophic variant of antiphospholipid syndrome (APS) is a very rare and life-threatening condition of APS. This condition is characterized by thrombosis in multiple organs within a short period of time in the presence of positive antiphospholipid antibodies (aPL). Over the past few decades, considerable progress has been made in the treatment of patients with catastrophic APS; however, the mortality rate still remains very high. Although some cases of rituximab treatment in patients with catastrophic APS have been reported, there is no clear treatment protocol. A 14-year-old girl with systemic lupus erythematosus was diagnosed with catastrophic APS. She received several medications: corticosteroids, intravenous immunoglobulin, and plasmapheresis with anticoagulants. Unfortunately, she did not improve, and rituximab was started with four courses. After the rituximab treatment, she did not experience further thrombotic events during the follow up. This paper reports a pediatric case of catastrophic APS treated successfully with rituximab in Korea.
MeSH Terms
-
Adolescent
Adrenal Cortex Hormones
Antibodies, Antiphospholipid
Anticoagulants
Antiphospholipid Syndrome*
Clinical Protocols
Female
Follow-Up Studies
Humans
Immunoglobulins
Korea
Lupus Erythematosus, Systemic*
Mortality
Plasmapheresis
Rituximab*
Thrombosis
Adrenal Cortex Hormones
Antibodies, Antiphospholipid
Anticoagulants
Immunoglobulins
Rituximab
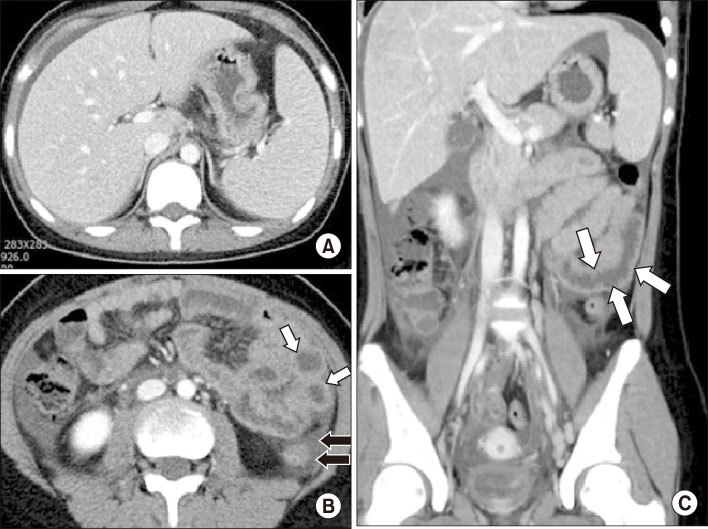
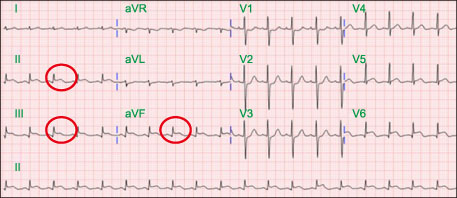
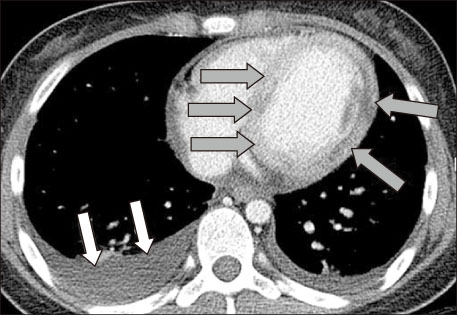
Figure
Cited by 1 articles
-
Initial Preserved Renal Function as a Predictor of Favorable Renal Response to Rituximab in Refractory or Relapsing Lupus Nephritis: A Single-center Cohort Study in Korea
Su Jin Choi, Soo Min Ahn, Ji Seon Oh, Seokchan Hong, Chang-Keun Lee, Bin Yoo, Yong-Gil Kim
J Rheum Dis. 2022;29(1):22-32. doi: 10.4078/jrd.2022.29.1.22.
Reference
-
1. Rodríguez-Pintó I, Moitinho M, Santacreu I, Shoenfeld Y, Erkan D, Espinosa G, et al. Catastrophic antiphospholipid syndrome (CAPS): Descriptive analysis of 500 patients from the International CAPS Registry. Autoimmun Rev. 2016; 15:1120–1124.
Article2. Erre GL, Pardini S, Faedda R, Passiu G. Effect of rituximab on clinical and laboratory features of APS; a case report and a review of literature. Lupus. 2008; 17:50–55.3. Whitaker KL. Antiphospholipid antibody syndrome: The difficulties of diagnosis. JAAPA. 2017; 30:10–14.4. Asherson RA, Cervera R, de Groot PG, Erkan D, Boffa MC, Piette JC, et al. Catastrophic antiphospholipid syndrome: international consensus statement on classification criteria and treatment guidelines. Lupus. 2003; 12:530–534.5. Cervera R, Font J, Gómez-Puerta JA, Espinosa G, Cucho M, Bucciarelli S, et al. Validation of the preliminary criteria for the classification of catastrophic antiphospholipid syndrome. Ann Rheum Dis. 2005; 64:1205–1209.6. Bucciarelli S, Espinosa G, Cervera R, Erkan D, Gómez-Puerta JA, Ramos-Casals M, et al. Mortality in the catastrophic antiphospholipid syndrome: causes of death and prognostic factors in a series of 250 patients. Arthritis Rheum. 2006; 54:2568–2576.
Article7. Sukara G, Baresic M, Sentic M, Brcic L, Anic B. Catastrophic antiphospholipid syndrome associated with systemic lupus erythematosus treated with rituximab: case report and a review of the literature. Acta Reumatol Port. 2015; 40:169–175.8. Ortel TL, Erkan D, Kitchens CS. How I treat catastrophic thrombotic syndromes. Blood. 2015; 126:1285–1293.
Article9. Monagle P, Chalmers E, Chan A, deVeber G, Kirkham F, Massicotte P, et al. Antithrombotic therapy in neonates and children: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133:6 Suppl. 887S–968S.10. Thomas O, Lybeck E, Strandberg K, Tynngård N, Schött U. Monitoring low molecular weight heparins at therapeutic levels: dose-responses of, and correlations and differences between aPTT, anti-factor Xa and thrombin generation assays. PLoS One. 2015; 10:e0116835.
Article11. Doğru A, Ugan Y, Şahin M, Karahan N, Tunç ŞE. Catastrophic antiphospholipid syndrome treated with rituximab: A case report. Eur J Rheumatol. 2017; 4:145–147.
Article12. Haskin O, Amir J, Schwarz M, Schonfeld T, Nahum E, Ling G, et al. Severe abdominal pain as a presenting symptom of probable catastrophic antiphospholipid syndrome. Pediatrics. 2012; 130:e230–e235.
Article13. Mok CC. Current role of rituximab in systemic lupus erythematosus. Int J Rheum Dis. 2015; 18:154–163.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Systemic Lupus Erythematosus and Secondary AntiphospholipidSyndrome Presenting as Livedo Reticularis
- A Case of Leg Ulcer with SLE and Antiphospholipid Syndrome
- A case of Limited Scleroderma Associated with Antiphospholipid Syndrome
- A Case of Systemic Lupus Erythematosus with Chorea as an Initial Manifestation
- A Case of Rituximab Therapy in Diffuse Alveolar Hemorrhage of Systemic Lupus Erythematosus Refractory to Steroid Pulse Therapy