Ann Rehabil Med.
2018 Feb;42(1):85-91. 10.5535/arm.2018.42.1.85.
Carpal Tunnel Syndrome Assessment With Ultrasonography: A Comparison Between Non-diabetic and Diabetic Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Korea University Guro Hospital, Seoul, Korea. caprock8@daum.net
- KMID: 2440973
- DOI: http://doi.org/10.5535/arm.2018.42.1.85
Abstract
OBJECTIVE
To investigate the diagnostic value of cross-sectional area (CSA) and wrist to forearm ratio (WFR) in patients with electro-diagnosed carpal tunnel syndrome (CTS) with or without diabetes mellitus (DM).
METHODS
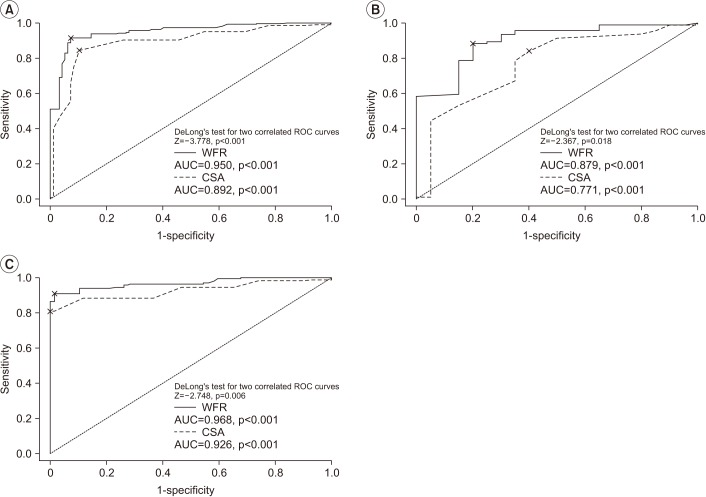
We retrospectively studied 256 CTS wrists and 77 healthy wrists in a single center between January 1, 2008 and January 1, 2013. The CSA and WFR were calculated for each wrist. Patients were classified into four groups according to the presence of DM and CTS: group 1, non-DM and non-CTS patients; group 2, non-DM and CTS patients; group 3, DM and non-CTS patients; and group 4, DM and CTS patients. To determine the optimal cut-off value, receiver operating characteristic (ROC) curve analysis was performed.
RESULTS
The CSA and WFR were significantly different among the groups (p < 0.001). The ROC curve analysis of non-DM patients revealed CSA ≥10.0 mm2 and WFR ≥1.52 as the most powerful diagnostic values of CTS. The ROC curve analysis revealed CSA ≥12.5 mm2 and WFR ≥1.87 as the most powerful diagnostic values of CTS.
CONCLUSION
Ultrasonographic assessment for the diagnosis of CTS requires a particular cut-off value for diabetic patients. Based on the ROC analysis results, improved accurate diagnosis is possible if WFR can be applied regardless of presence or absence of DM.
MeSH Terms
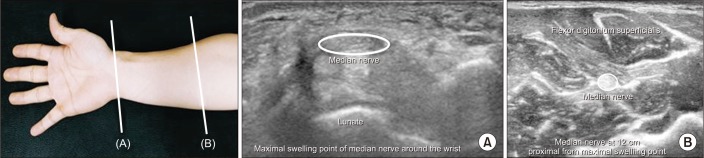
Figure
Reference
-
1. Werner RA, Andary M. Carpal tunnel syndrome: pathophysiology and clinical neurophysiology. Clin Neurophysiol. 2002; 113:1373–1381. PMID: 12169318.
Article2. Wong SM, Griffith JF, Hui AC, Lo SK, Fu M, Wong KS. Carpal tunnel syndrome: diagnostic usefulness of sonography. Radiology. 2004; 232:93–99. PMID: 15155897.
Article3. Jeong JS, Yoon JS, Kim SJ, Park BK, Won SJ, Cho JM, et al. Usefulness of ultrasonography to predict response to injection therapy in carpal tunnel syndrome. Ann Rehabil Med. 2011; 35:388–394. PMID: 22506149.
Article4. Pourmemari MH, Shiri R. Diabetes as a risk factor for carpal tunnel syndrome: a systematic review and meta-analysis. Diabet Med. 2016; 33:10–16. PMID: 26173490.
Article5. Breiner A, Qrimli M, Ebadi H, Alabdali M, Lovblom LE, Abraham A, et al. Peripheral nerve high-resolution ultrasound in diabetes. Muscle Nerve. 2017; 55:171–178. PMID: 27312883.
Article6. Moon HI, Kwon HK, Kim L, Lee HJ, Lee HJ. Ultrasonography of palm to elbow segment of median nerve in different degrees of diabetic polyneuropathy. Clin Neurophysiol. 2014; 125:844–848. PMID: 24269093.
Article7. Zaidman CM, Al-Lozi M, Pestronk A. Peripheral nerve size in normals and patients with polyneuropathy: an ultrasound study. Muscle Nerve. 2009; 40:960–966. PMID: 19697380.
Article8. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011; 34(Suppl 1):S62–S69. PMID: 21193628.9. Kang S, Kwon HK, Kim KH, Yun HS. Ultrasonography of median nerve and electrophysiologic severity in carpal tunnel syndrome. Ann Rehabil Med. 2012; 36:72–79. PMID: 22506238.
Article10. Kotevoglu N, Gülbahce-Saglam S. Ultrasound imaging in the diagnosis of carpal tunnel syndrome and its relevance to clinical evaluation. Joint Bone Spine. 2005; 72:142–145. PMID: 15797494.
Article11. Rempel D, Dahlin L, Lundborg G. Pathophysiology of nerve compression syndromes: response of peripheral nerves to loading. J Bone Joint Surg Am. 1999; 81:1600–1610. PMID: 10565653.12. Yayama T, Kobayashi S, Nakanishi Y, Uchida K, Kokubo Y, Miyazaki T, et al. Effects of graded mechanical compression of rabbit sciatic nerve on nerve blood flow and electrophysiological properties. J Clin Neurosci. 2010; 17:501–505. PMID: 20122834.
Article13. Sandireddy R, Yerra VG, Areti A, Komirishetty P, Kumar A. Neuroinflammation and oxidative stress in diabetic neuropathy: futuristic strategies based on these targets. Int J Endocrinol. 2014; 2014:674987. PMID: 24883061.
Article14. Yagihashi S. Recent advances in clinical practice and in basic research on diabetic neuropathy. Brain Nerve. 2011; 63:571–582. PMID: 21613660.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Local Steroid Injection in Carpal Tunnel Syndrome
- Outcomes of Carpal Tunnel Release in Diabetic and Non-Diabetic Patients
- Diabetic neuropathy with concurrent carpal tunnel syndrome
- Prevalence and Risk Factors of Carpal Tunnel Syndrome in Diabetic Patients
- Electrodiagnosis of Carpal Tunnel Syndrome in Patients with Diabetic Neuropathy