Ann Rehabil Med.
2019 Feb;43(1):96-105. 10.5535/arm.2019.43.1.96.
Combined Therapy With Functional Electrical Stimulation and Standing Frame in Stroke Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Dong-A University College of Medicine, Busan, Korea.
- 2Regional Cardiocerebrovascular Center, Dong-A University Medical Center, Busan, Korea.
- 3Department of Physical Medicine and Rehabilitation, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. lsj995414@hanmail.net
- KMID: 2440957
- DOI: http://doi.org/10.5535/arm.2019.43.1.96
Abstract
OBJECTIVE
To investigate the effects of combination functional electrical stimulation (FES) and standing frame training on standing balance in stroke patients.
METHODS
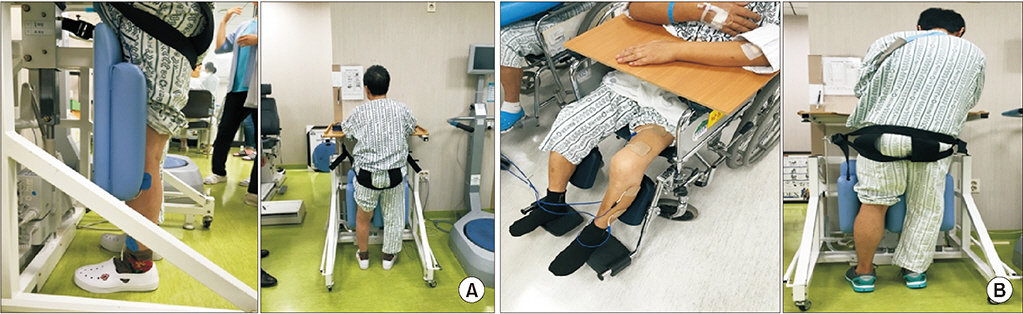
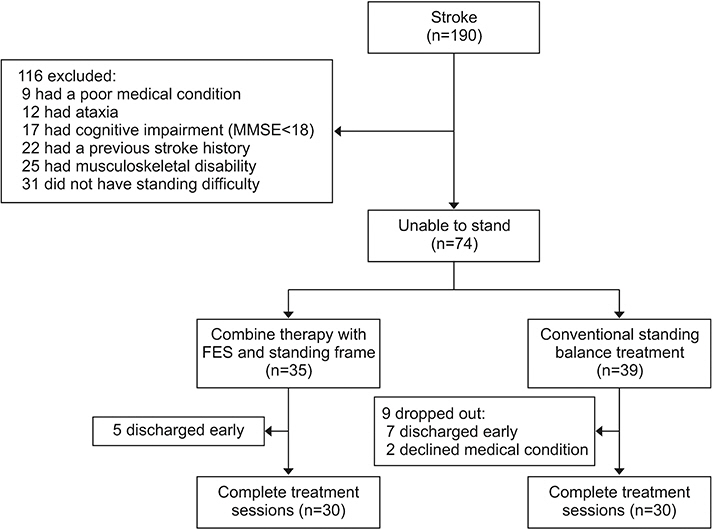
Patients who had hemiparesis and postural instability after stroke were randomly assigned to one of the two groups; study group underwent FES on the quadriceps and tibialis anterior muscle simultaneously with standing balance training. The control group received standing frame training and FES separately. Both the groups received their respective therapies for 3 weeks. Stability index in Biodex Balance master system, Berg Balance Scale (BBS), manual muscle test, the Korean version of Modified Barthel Index, and Korean version of Mini-Mental State Examination were used to evaluate the effects of the treatment.
RESULTS
In total, 30 patients were recruited to the study group and 30 to the control group. Three weeks after treatment, both the groups showed improvement in postural stability scores and physical and cognitive functions. When changes in postural stability were compared between the groups, the study group showed more significant improvement than the control group with regards to the scores of BBS and the stability indices.
CONCLUSION
In this study, we found the therapeutic effectiveness of combined therapy of FES and standing frame in subacute stroke patients. The presented protocol is proposed as time-saving and can be applied easily in the clinical setting. Thus, the proposed combined therapy could be a useful method for improving standing balance in subacute stroke patients.
Figure
Reference
-
1. Aze O, Odjardias E, Devillard X, Akplogan B, Calmels P, Giraux P. Structural and physiological muscle changes after post-stroke hemiplegia: a systematic review. Ann Phys Rehabil Med. 2016; 59 Suppl:e79.
Article2. Mohapatra S, Harrington R, Chan E, Dromerick AW, Breceda EY, Harris-Love M. Role of contralesional hemisphere in paretic arm reaching in patients with severe arm paresis due to stroke: a preliminary report. Neurosci Lett. 2016; 617:52–8.
Article3. Vistamehr A, Kautz SA, Bowden MG, Neptune RR. Correlations between measures of dynamic balance in individuals with post-stroke hemiparesis. J Biomech. 2016; 49:396–400.
Article4. de Haart M, Geurts AC, Huidekoper SC, Fasotti L, van Limbeek J. Recovery of standing balance in postacute stroke patients: a rehabilitation cohort study. Arch Phys Med Rehabil. 2004; 85:886–95.5. Geurts AC, de Haart M, van Nes IJ, Duysens J. A review of standing balance recovery from stroke. Gait Posture. 2005; 22:267–81.
Article6. Hokstad A, Indredavik B, Bernhardt J, Langhammer B, Gunnes M, Lundemo C, et al. Upright activity within the first week after stroke is associated with better functional outcome and health-related quality of life: a Norwegian multi-site study. J Rehabil Med. 2016; 48:280–6.
Article7. Cabanas-Valdes R, Bagur-Calafat C, Girabent-Farres M, Caballero-Gomez FM, Hernandez-Valino M, Urrutia Cuchi G. The effect of additional core stability exercises on improving dynamic sitting balance and trunk control for subacute stroke patients: a randomized controlled trial. Clin Rehabil. 2016; 30:1024–33.
Article8. Liu M, Chen J, Fan W, Mu J, Zhang J, Wang L, et al. Effects of modified sit-to-stand training on balance control in hemiplegic stroke patients: a randomized controlled trial. Clin Rehabil. 2016; 30:627–36.
Article9. Hugues A, Di Marco J, Janiaud P, Xue Y, Pires J, Khademi H, et al. Efficiency of physical therapy on postural imbalance after stroke: study protocol for a systematic review and meta-analysis. BMJ Open. 2017; 7:e013348.
Article10. Beyaert C, Vasa R, Frykberg GE. Gait post-stroke: pathophysiology and rehabilitation strategies. Neurophysiol Clin. 2015; 45:335–55.
Article11. Zhang D, Zhu K. Simulation study of FES-assisted standing up with neural network control. Conf Proc IEEE Eng Med Biol Soc. 2004; 7:4877–80.
Article12. Bagley P, Hudson M, Forster A, Smith J, Young J. A randomized trial evaluation of the Oswestry Standing Frame for patients after stroke. Clin Rehabil. 2005; 19:354–64.
Article13. Hendrie WA, Watson MJ, McArthur MA. A pilot mixed methods investigation of the use of Oswestry Standing Frames in the homes of nine people with severe multiple sclerosis. Disabil Rehabil. 2015; 37:1178–85.
Article14. Nadeau SM, Boukadida A, Piotte F, Mesure S. Weightbearing perception during standing and sit-to-stand tasks in subacute post-stroke individuals undergoing intensive rehabilitation. Ann Phys Rehabil Med. 2016; 59 Suppl:e71–e72.
Article15. Kim K, Kim YM, Kang DY. Repetitive sit-to-stand training with the step-foot position on the non-paretic side, and its effects on the balance and foot pressure of chronic stroke subjects. J Phys Ther Sci. 2015; 27:2621–4.
Article16. Raja B, Neptune RR, Kautz SA. Quantifiable patterns of limb loading and unloading during hemiparetic gait: Relation to kinetic and kinematic parameters. J Rehabil Res Dev. 2012; 49:1293–304.
Article17. Montastruc J, Amarantini D, Lambert V, Castel-Lacanal E, Marque P, Gasq D. Main determinants of weight-bearing asymmetry in hemiplegic stroke patients. Ann Phys Rehabil Med. 2016; 59 Suppl:e69.
Article18. De Nunzio A, Zucchella C, Spicciato F, Tortola P, Vecchione C, Pierelli F, et al. Biofeedback rehabilitation of posture and weightbearing distribution in stroke: a center of foot pressure analysis. Funct Neurol. 2014; 29:127–34.19. Messier S, Bourbonnais D, Desrosiers J, Roy Y. Weightbearing on the lower limbs in a sitting position during bilateral movement of the upper limbs in post-stroke hemiparetic subjects. J Rehabil Med. 2005; 37:242–6.
Article20. Gervasoni E, Parelli R, Uszynski M, Crippa A, Marzegan A, Montesano A, et al. Effects of functional electrical stimulation on reducing falls and improving gait parameters in multiple sclerosis and stroke. PM R. 2017; 9:339–47.
Article21. Tan ZM, Jiang WW, Yan TB, Wu W, Song R. Effects of functional electrical stimulation based on normal gait pattern on walking function in subjects with recovery of stroke. Zhonghua Yi Xue Za Zhi. 2016; 96:2342–6.22. Bustamante C, Brevis F, Canales S, Millon S, Pascual R. Effect of functional electrical stimulation on the proprioception, motor function of the paretic upper limb, and patient quality of life: a case report. J Hand Ther. 2016; 29:507–14.
Article23. Malesevic J, Strbac M, Isakovic M, Kojic V, Konstantinovic L, Vidakovic A, et al. Evolution of surface motor activation zones in hemiplegic patients during 20 sessions of FES therapy with multi-pad electrodes. Eur J Transl Myol. 2016; 26:6059.
Article24. Maeda N, Urabe Y, Murakami M, Itotani K, Kato J. Discriminant analysis for predictor of falls in stroke patients by using the Berg Balance Scale. Singapore Med J. 2015; 56:280–3.
Article25. Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008; 88:559–66.
Article26. Palm HG, Lang P, Strobel J, Riesner HJ, Friemert B. Computerized dynamic posturography: the influence of platform stability on postural control. Am J Phys Med Rehabil. 2014; 93:49–55.27. Chen HX, Yang ZJ, Pan RH, Guo YH, Zhan LC, He MF, et al. Effect of comprehensive protocol of integrative medicine on motor function, activity of daily living and quality of life in hemiplegia patients after stroke. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2016; 36:395–8.28. Haruyama K, Kawakami M, Otsuka T. Effect of core stability training on trunk function, standing balance, and mobility in stroke patients. Neurorehabil Neural Repair. 2017; 31:240–9.
Article29. Grainger KP, Masterson S, Jennings M. ‘Things aren’t the same, are they?’: the management of bad news delivery in the discourse of stroke care. Commun Med. 2005; 2:35–44.
Article30. Matjacic Z, Zadravec M, Oblak J. Sit-to-stand trainer: an apparatus for training “normal-like” sit to stand movement. IEEE Trans Neural Syst Rehabil Eng. 2016; 24:639–49.
Article31. Braun T, Marks D, Thiel C, Zietz D, Zutter D, Gruneberg C. Effects of additional, dynamic supported standing practice on functional recovery in patients with sub-acute stroke: a randomized pilot and feasibility trial. Clin Rehabil. 2016; 30:374–82.
Article32. Bishop L, Khan M, Martelli D, Quinn L, Stein J, Agrawal S. Exploration of two training paradigms using forced induced weight shifting with the tethered pelvic assist device to reduce asymmetry in individuals after stroke: case reports. Am J Phys Med Rehabil. 2017; 96(10 Suppl 1):S135–40.33. Chen D, Yan T, Li G, Li F, Liang Q. Functional electrical stimulation based on a working pattern influences function of lower extremity in subjects with early stroke and effects on diffusion tensor imaging: a randomized controlled trial. Zhonghua Yi Xue Za Zhi. 2014; 94:2886–92.34. Thibaut A, Moissenet F, Di Perri C, Schreiber C, Remacle A, Kolanowski E, et al. Brain plasticity after implanted peroneal nerve electrical stimulation to improve gait in chronic stroke patients: Two case reports. NeuroRehabilitation. 2017; 40:251–8.
Article35. Palmer JA, Hsiao H, Wright T, Binder-Macleod SA. Single session of functional electrical stimulationassisted walking produces corticomotor symmetry changes related to changes in poststroke walking mechanics. Phys Ther. 2017; 97:550–60.
Article36. van Bloemendaal M, Bus SA, de Boer CE, Nollet F, Geurts AC, Beelen A. Gait training assisted by multichannel functional electrical stimulation early after stroke: study protocol for a randomized controlled trial. Trials. 2016; 17:477.
Article37. Ferrante S, Chia Bejarano N, Ambrosini E, Nardone A, Turcato AM, Monticone M, et al. A personalized multi-channel FES controller based on muscle synergies to support gait rehabilitation after stroke. Front Neurosci. 2016; 10:425.
Article38. Khaslavskaia S, Sinkjaer T. Motor cortex excitability following repetitive electrical stimulation of the common peroneal nerve depends on the voluntary drive. Exp Brain Res. 2005; 162:497–502.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rewiring the Lesioned Brain: Electrical Stimulation for Post-Stroke Motor Restoration
- Effects of Electrical Stimulation for Dysphagia Caused by Stroke
- The Effect of an Abdominal Drawing-In Maneuver Combined with Low·High Frequency Neuromuscular Electrical Stimulation on Trunk Muscle Activity, Muscle Fatigue, and Balance in Stroke Patients
- The Changes of Motor Evoked Potential and Silent Period after Electrical Stimulation in Stroke Patients
- The Effect of Functional Electrical Stimulation on Swallowing Function in Stroke Patients with Dysphagia