Pediatr Gastroenterol Hepatol Nutr.
2019 Mar;22(2):181-188. 10.5223/pghn.2019.22.2.181.
Micronutrients Are Not Deficient in Children with Nonorganic Failure to Thrive
- Affiliations
-
- 1Department of Pediatrics, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Division of Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Severance Pediatric IBD Research Group, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. PEDKS@yuhs.ac
- KMID: 2440592
- DOI: http://doi.org/10.5223/pghn.2019.22.2.181
Abstract
- PURPOSE
Inadequate calorie intake is one of the most important causes of nonorganic failure to thrive (NOFTT) and is thought to lead to multiple micronutrient deficiencies. However, there have been few studies on NOFTT and micronutrients. The aim of this study was to evaluate the micronutrient status of children with NOFTT.
METHODS
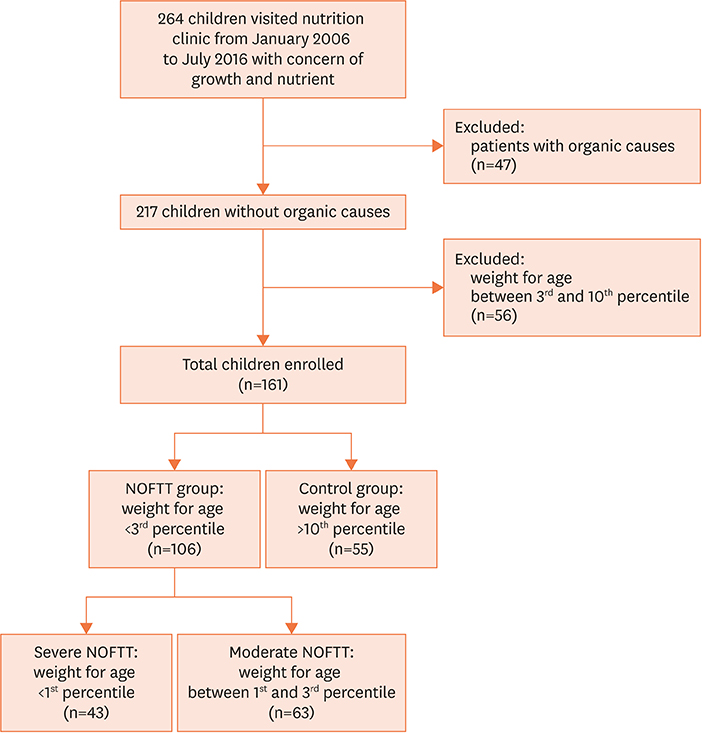
We conducted a retrospective cohort study in 161 children (106 with NOFTT and 55 health controls) at a single institution. Data on weight for age, height for age, body mass index, and biochemical parameters, indicating the children's nutritional and micronutrient status were reviewed via electronic medical records, and the two groups were compared.
RESULTS
Except inorganic phosphate levels, no statistically significant differences were seen in the laboratory findings indicating the children's nutritional and micronutrient status; notably, the inorganic phosphate levels were within the normal range in both groups. We then compared the severe NOFTT (weight for age below the first percentile) and control groups; however, no statistically significant differences were seen for any of the measured parameters.
CONCLUSION
Most children with NOFTT in this study had normal micronutrient levels and other laboratory findings. Therefore, element deficiencies should not be considered a natural consequence of NOFTT or in healthy children. Close monitoring and additional evaluations are needed.
Keyword
MeSH Terms
Figure
Reference
-
1. Zenel JA Jr. Failure to thrive: a general pediatrician's perspective. Pediatr Rev. 1997; 18:371–378.
Article2. Olsen EM. Failure to thrive: still a problem of definition. Clin Pediatr (Phila). 2006; 45:1–6.
Article3. Rudolf MC, Logan S. What is the long term outcome for children who fail to thrive? A systematic review. Arch Dis Child. 2005; 90:925–931.
Article4. Reif S, Beler B, Villa Y, Spirer Z. Long-term follow-up and outcome of infants with non-organic failure to thrive. Isr J Med Sci. 1995; 31:483–489.5. Jaffe AC. Failure to thrive: current clinical concepts. Pediatr Rev. 2011; 32:100–107.
Article6. Moon JH, Beck NS, Kim JY. Clinical manifestation of children with failure to thrive. Korean J Pediatr Gastroenterol Nutr. 2000; 3:68–74.
Article7. Jeong SJ. Nutritional approach to failure to thrive. Korean J Pediatr. 2011; 54:277–281.
Article8. Gernand AD, Schulze KJ, Stewart CP, West KP Jr, Christian P. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat Rev Endocrinol. 2016; 12:274–289.
Article9. Shenkin A. Micronutrients in health and disease. Postgrad Med J. 2006; 82:559–567.
Article10. Black MM. Micronutrient deficiencies and cognitive functioning. J Nutr. 2003; 133:3927S–31S.
Article11. Bhan MK, Sommerfelt H, Strand T. Micronutrient deficiency in children. Br J Nutr. 2001; 85:Suppl 2. S199–203.
Article12. Tulchinsky TH. Micronutrient deficiency conditions: global health issues. Public Health Rev. 2010; 32:BF03391600.
Article13. Cole SZ, Lanham JS. Failure to thrive: an update. Am Fam Physician. 2011; 83:829–834.14. Saper RB, Rash R. Zinc: an essential micronutrient. Am Fam Physician. 2009; 79:768–772.15. Salgueiro MJ, Zubillaga M, Lysionek A, Sarabia MI, Caro R, De Paoli T, et al. Zinc as an essential micronutrient: a review. Nutr Res. 2000; 20:737–755.
Article16. World Health Organization. The world health report 2002: reducing risks, promoting healthy life. Geneva: World Health Organization;2002.17. Aburto NJ, Ramirez-Zea M, Neufeld LM, Flores-Ayala R. Some indicators of nutritional status are associated with activity and exploration in infants at risk for vitamin and mineral deficiencies. J Nutr. 2009; 139:1751–1757.
Article18. Berkovitch M, Heyman E, Afriat R, Matz-Khromchenko I, Avgil M, Greenberg R, et al. Copper and zinc blood levels among children with nonorganic failure to thrive. Clin Nutr. 2003; 22:183–186.
Article19. Kanis JA. Primer on the metabolic bone diseases and disorders of mineral metabolism. Clin Endocrinol (Oxf). 2000; 52:526.
Article20. Holick MF. Vitamin D deficiency. N Engl J Med. 2007; 357:266–281.
Article21. Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006; 84:18–28.
Article22. Lee JH. Micronutrient deficiency syndrome: zinc, copper and selenium. Pediatr Gastroenterol Hepatol Nutr. 2012; 15:145–150.
Article23. Kang DS, Lee KS. The status of dietary supplements intake in Korean preschool children: data from the Korea national health and nutrition examination survey 2010–2012. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:178–185.
Article24. Kim YH, Lee SG, Kim SH, Song YJ, Chung JY, Park MJ. Nutritional status of Korean toddlers: from the Korean national health and nutrition examination survey 2007~2009. Korean J Pediatr Gastroenterol Nutr. 2011; 14:161–170.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Management of Failure to Thrive
- Clinical Characteristics of Failure to Thrive in Infant and Toddler: Organic vs. Nonorganic
- A Clinical Observation on Failure to Thrive
- Failure to Thrive
- Essential micronutrients in children and adolescents with a focus on growth and development: a narrative review