Pediatr Gastroenterol Hepatol Nutr.
2013 Dec;16(4):261-268.
Clinical Characteristics of Failure to Thrive in Infant and Toddler: Organic vs. Nonorganic
- Affiliations
-
- 1Department of Pediatrics, Pusan National University School of Medicine, Yangsan, Korea. jhongpark@pusan.ac.kr
Abstract
- PURPOSE
To investigate the clinical characteristics and outcomes among infants and toddlers with failure to thrive (FTT).
METHODS
This retrospective study was done with 123 patients who had visited Pusan National University Children's Hospital during their first two years of life and had received an FTT diagnosis. We compared the clinical characteristics of the patients based on the causes of their FTT and their ages at the time of first hospital visit. We investigated triggering factors, feeding practices, and outcomes in 25 patients with nonorganic FTT (NOFTT).
RESULTS
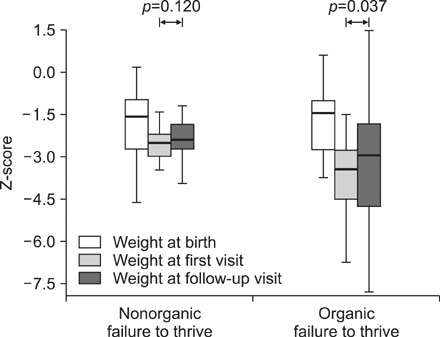
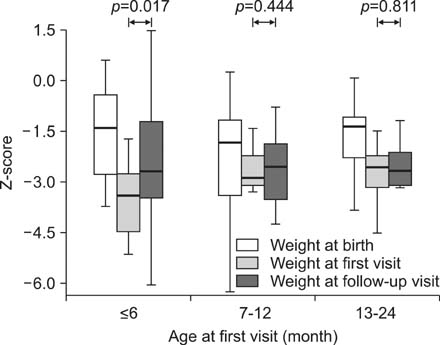
Eighty cases (65.0%) were NOFTT. The gestational ages, birth weights, and weights at the first visits were significantly lower in patients with organic FTT (OFTT) (p<0.05). Infants who had first visited the clinic at age <6 months had the least z-score. The percentage of patients with severe weight decline was higher in OFTT than in NOFTT (60.0% vs. 17.3%). The z-scores at the follow-up visits were improved after treatment in both of the groups. Preceding infection was the most common triggering factor of NOFTT and persecutory feeding as abnormal behavior of caregiver was observed in 22 cases (88.0%). After treatment with feeding method modification, all patients with NOFTT showed normal growth.
CONCLUSION
Weight decline is more severe in OFTT patients and in younger patients at the first visit. Infants with FTT can attain normal weight gain growth by treating organic diseases and supplying proper nutrition in OFTT, and by correcting abnormal dietary behavior of caregiver in NOFTT.
Keyword
MeSH Terms
Figure
Reference
-
1. Cole SZ, Lanham JS. Failure to thrive: an update. Am Fam Physician. 2011; 83:829–834.2. Olsen EM. Failure to thrive: still a problem of definition. Clin Pediatr (Phila). 2006; 45:1–6.
Article3. Olsen EM, Petersen J, Skovgaard AM, Weile B, Jørgensen T, Wright CM. Failure to thrive: the prevalence and concurrence of anthropometric criteria in a general infant population. Arch Dis Child. 2007; 92:109–114.
Article4. Zenel JA Jr. Failure to thrive: a general pediatrician's perspective. Pediatr Rev. 1997; 18:371–378.
Article5. Emond A, Drewett R, Blair P, Emmett P. Postnatal factors associated with failure to thrive in term infants in the Avon Longitudinal Study of Parents and Children. Arch Dis Child. 2007; 92:115–119.
Article6. Homer C, Ludwig S. Categorization of etiology of failure to thrive. Am J Dis Child. 1981; 135:848–851.
Article7. Bauchner H. Failure to thrive. In : Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson textbook of pediatrics. 18th ed. Philadelphia: Elsevier Saunders;2007. p. 184–187.8. Schwartz ID. Failure to thrive: an old nemesis in the new millennium. Pediatr Rev. 2000; 21:257–264.
Article9. Powell GF. Nonorganic failure to thrive in infancy: an update on nutrition, behavior, and growth. J Am Coll Nutr. 1988; 7:345–353.
Article10. Moon JH, Beck NS, Kim JY. Clinical manifestation of children with failure to thrive. Korean J Pediatr Gastroenterol Nutr. 2000; 3:68–74.
Article11. Lee BC, Kim HR, Sohn CL, Kam S, Hwang JB. Clinical outcomes of infants with failure to gain weight among out-patients. Korean J Pediatr. 2004; 47:604–610.12. Nam HK, Lee MI, Ahn DH, Sohn KC. Study on the clinical aspect of failure to thrive. J Korean Pediatr Soc. 1989; 32:303–310.13. Lim YT, Kim CY. A clinical observation on failure to thrive. J Korean Pediatr Soc. 1987; 30:259–265.14. Lee K. A study on non-organic failure to thrive infants. J Korean Pediatr Soc. 1994; 37:464–471.15. Dykman RA, Casey PH, Ackerman PT, McPherson WB. Behavioral and cognitive status in school-aged children with a history of failure to thrive during early childhood. Clin Pediatr (Phila). 2001; 40:63–70.
Article16. Kristiansson B, Fällström SP. Growth at the age of 4 years subsequent to early failure to thrive. Child Abuse Negl. 1987; 11:35–40.
Article17. Drewett RF, Corbett SS, Wright CM. Cognitive and educational attainments at school age of children who failed to thrive in infancy: a population-based study. J Child Psychol Psychiatry. 1999; 40:551–561.
Article18. Black MM, Dubowitz H, Krishnakumar A, Starr RH Jr. Early intervention and recovery among children with failure to thrive: follow-up at age 8. Pediatrics. 2007; 120:59–69.
Article19. Levy Y, Levy A, Zangen T, Kornfeld L, Dalal I, Samuel E, et al. Diagnostic clues for identification of nonorganic vs organic causes of food refusal and poor feeding. J Pediatr Gastroenterol Nutr. 2009; 48:355–362.
Article20. Korea Center for Disease Control and Prevention. The Korean Pediatric Society. The Committee for the Development of Growth Standard for Korean Children and Adolescents. 2007 Korean Children and Adolescents Growth Standard (commentary for the development of 2007 growth chart) [Government report online]. Seoul: Division of Chronic Disease Surveillance;2007. cited 2007 Nov. Available from: http://www.cdc.go.kr/.21. Waterlow JC. Note on the assessment and classification of protein-energy malnutrition in children. Lancet. 1973; 2:87–89.
Article22. Hosseini F, Borzouei B, Vahabian M. Failure to thrive severity determination by new design curves in standard growth charts. Acta Med Iran. 2011; 49:795–800.23. Daniel M, Kleis L, Cemeroglu AP. Etiology of failure to thrive in infants and toddlers referred to a pediatric endocrinology outpatient clinic. Clin Pediatr (Phila). 2008; 47:762–765.
Article24. Olsen EM, Skovgaard AM, Weile B, Jørgensen T. Risk factors for failure to thrive in infancy depend on the anthropometric definitions used: the Copenhagen County Child Cohort. Paediatr Perinat Epidemiol. 2007; 21:418–431.
Article25. McDougall P, Drewett RF, Hungin AP, Wright CM. The detection of early weight faltering at the 6-8-week check and its association with family factors, feeding and behavioural development. Arch Dis Child. 2009; 94:549–552.
Article26. Tolia V. Very early onset nonorganic failure to thrive in infants. J Pediatr Gastroenterol Nutr. 1995; 20:73–80.
Article27. Rudolf MC, Logan S. What is the long term outcome for children who fail to thrive? A systematic review. Arch Dis Child. 2005; 90:925–931.
Article28. Schmitt BD, Mauro RD. Nonorganic failure to thrive: an outpatient approach. Child Abuse Negl. 1989; 13:235–248.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical approaches to failure to thrive of infants and toddlers: a new paradigm
- A Study on Non-Organic Failure to Thrive Infants
- Clinical Characteristics of Neurocognitive Function in Patients with Traumatic Brain Injury Referred for Mental Disability Evaluation
- A Clinical Observation on Failure to Thrive
- Transient Pseudohypoaldosteronism in a 5-Month-old Infant Manifested as a Failure to Thrive