J Korean Med Sci.
2017 Aug;32(8):1351-1359. 10.3346/jkms.2017.32.8.1351.
Sebaceous Carcinoma: Clinicopathologic Analysis of 29 Cases in a Tertiary Hospital in Korea
- Affiliations
-
- 1Department of Dermatology, Chonbuk National University Hospital, Jeonju, Korea. dermayun@jbnu.ac.kr
- 2Research Institute of Clinical Medicine of Chonbuk National University, Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2439471
- DOI: http://doi.org/10.3346/jkms.2017.32.8.1351
Abstract
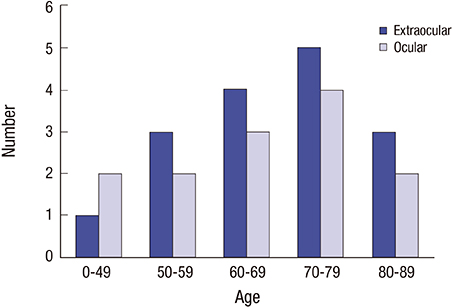
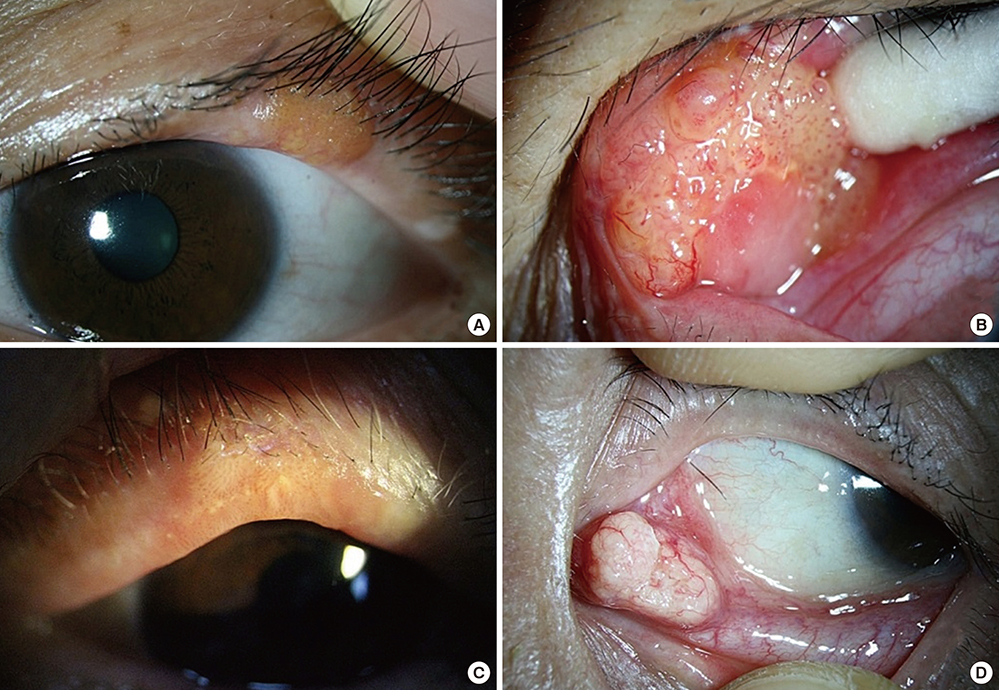
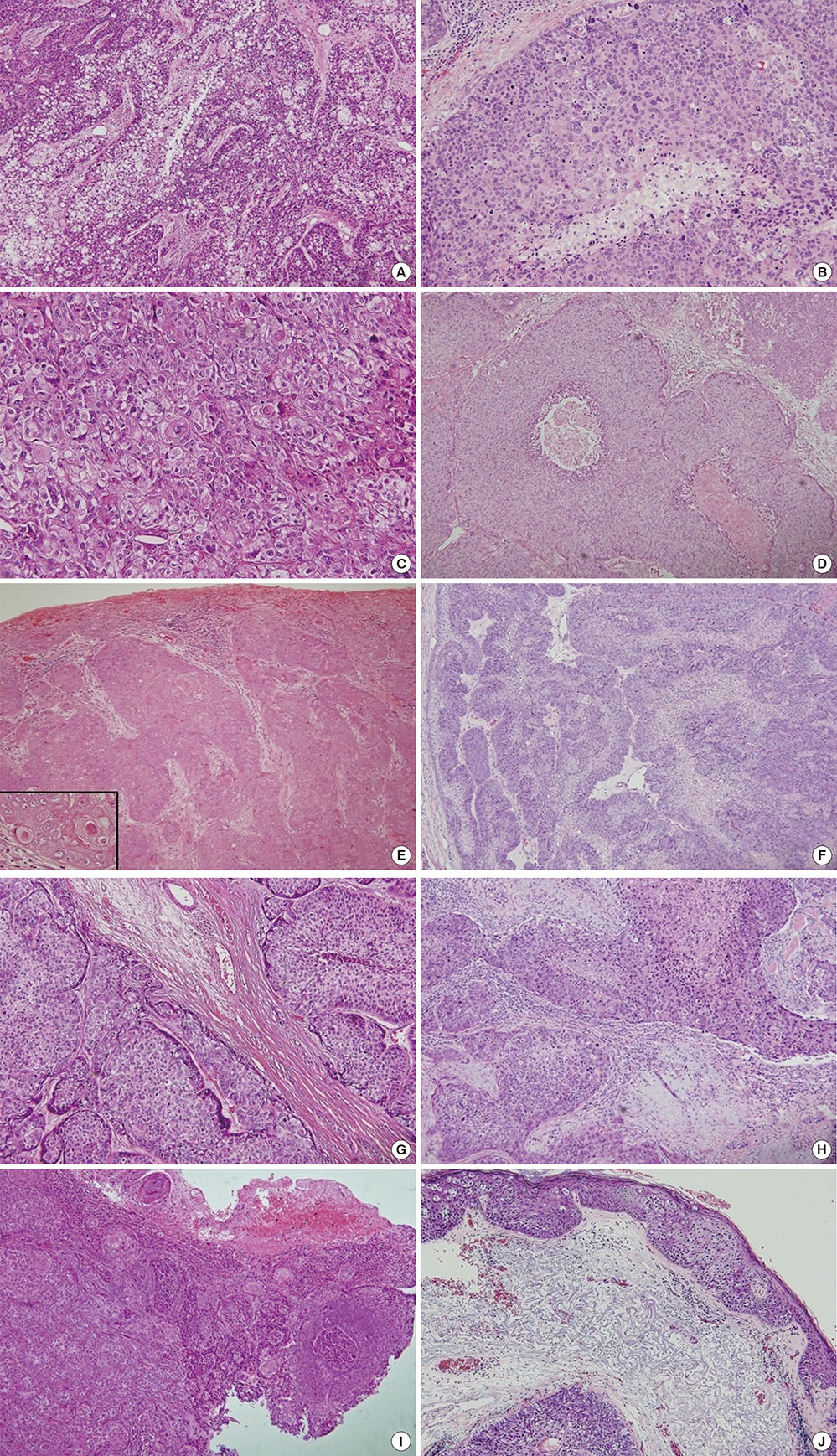
- Sebaceous carcinoma (SC) is a neoplasm derived from the adnexal epithelium of the sebaceous glands, and most studies on this neoplasm have been conducted in Caucasians. We retrospectively reviewed the records of 29 patients with SC (16 extraocular and 13 ocular lesions) who were diagnosed from 2001 to 2014 to analyze the clinical and histopathological features of SC in the Korean population. Sixteen of the patients were women and 13 were men. There was an equal sex distribution for extraocular lesions, and a female predilection (M:F = 1:1.6) for ocular lesions. The mean ages at presentation of extraocular and ocular lesions were 69.19 ± 37.19 (range, 32-87) and 67.46 ± 24.46 (range, 43-85) years, respectively. Most lesions occurred in the eyelid (13/29, 44.83%), and most extraocular lesions occurred in the head and neck area (13/16, 81.25%). There was no recurrence or death during the follow-up period. Most lesions were poorly differentiated (extraocular, 43.75%; ocular, 38.46%), had a lobular infiltrative growth pattern (extraocular, 68.75%; ocular, 76.92%), and were basaloid (extraocular, 56.25%; ocular, 61.54%). Only 5 cases (2 extraocular and 3 ocular lesions) showed pagetoid spread. Extraocular lesions were marginally more common than the ocular form. There were higher incidences in elderly patients, who also had the highest incidence of eyelid lesions. The proportion of cells with sebaceous differentiation and prominent growth patterns were variable. Our results show that SC may not be very aggressive in Koreans.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Features and Association with Visceral Malignancy in 80 Patients with Sebaceous Neoplasms
Jee Eun Kim, Jong Hoon Kim, Kee-Yang Chung, Jin Sook Yoon, Mi Ryung Roh
Ann Dermatol. 2019;31(1):14-21. doi: 10.5021/ad.2019.31.1.14.
Reference
-
1. Nelson BR, Hamlet KR, Gillard M, Railan D, Johnson TM. Sebaceous carcinoma. J Am Acad Dermatol. 1995; 33:1–15.2. Srivastava D, Taylor RS. Appendage tumors and hamartomas of the skin. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's Dermatology in General Medicine. 8th ed. New York, NY: McGraw-Hill;2012. p. 1341–1342.3. Kyllo RL, Brady KL, Hurst EA. Sebaceous carcinoma: review of the literature. Dermatol Surg. 2015; 41:1–15.4. Zürcher M, Hintschich CR, Garner A, Bunce C, Collin JR. Sebaceous carcinoma of the eyelid: a clinicopathological study. Br J Ophthalmol. 1998; 82:1049–1055.5. Dasgupta T, Wilson LD, Yu JB. A retrospective review of 1349 cases of sebaceous carcinoma. Cancer. 2009; 115:158–165.6. Kang SK, Bae GY, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. A case of well-differentiated sebaceous carcinoma. Korean J Dermatol. 2002; 40:586–589.7. Lee GC, Kim YG, Yoon TY. Sebaceous carcinoma arising from nevus sebaceus. Korean J Dermatol. 2005; 43:840–842.8. Kim JE, Lee JD, Cho SH. A case of sebaceous carcinoma and basal cell carcinoma arising in nevus sebaceus. Korean J Dermatol. 2004; 42:205–207.9. Nam JH, Choi YJ, Kim TH, Lee GY, Kim WS, Kim KJ. A case of extraocular sebaceous carcinoma arising from nevus sebaceus. Korean J Dermatol. 2009; 47:326–329.10. Lee BJ, Kim YC, Kang HY. A case of sebaceous carcinoma arising from Bowen’s disease. Korean J Dermatol. 2003; 41:1072–1075.11. Chang DS, Seo SJ, Hong CK. Two cases of sebaceous carcinoma developed on the unusual site: a case of Muir-Torre syndrome. Korean J Dermatol. 2001; 39:587–591.12. Hur SG, Kim JS, Lee SC, Chun IK, Kim YP. A case of sebaceous carcinoma arising from nevus sebaceus of Jadassohn. Korean J Dermatol. 1991; 29:104–108.13. Lee HT, Jang HS, Kwon KS, Choi HY, Myung KB. A case of multiple sebaceous carcinomas on the frontal region. Korean J Dermatol. 1997; 35:824–829.14. Seo BF, Jung HW, Choi IK, Rhie JW. Sebaceous carcinoma of the suprapubic area in a liver transplant recipient. Ann Dermatol. 2014; 26:395–398.15. Jang KA, Ahn SJ, Choi JH, Koh JK. Sebaceous carcinoma and basal cell epithelioma developed in organoid nevus. Ann Dermatol. 1999; 11:59–61.16. Park YT, Yoo SJ, Park TH, Yoo JH, Kim KJ. Extraocular sebaceous carcinoma. Ann Dermatol. 2004; 16:13–15.17. Byeon JH, Yum WS, Rhie JW, Lee CK, Lim P. A clinical review of eyelid sebaceous carcinoma. J Korean Soc Plast Reconstr Surg. 1998; 25:446–452.18. Lee JJ, Won YH, Chun IK, Kim YP. A case of sebaceous gland carcinoma of the eyelid with huge mass. Korean J Dermatol. 1989; 27:338–342.19. Shields JA, Demirci H, Marr BP, Eagle RC Jr, Shields CL. Sebaceous carcinoma of the eyelids: personal experience with 60 cases. Ophthalmology. 2004; 111:2151–2157.20. Shields JA, Demirci H, Marr BP, Eagle RC Jr, Shields CL. Sebaceous carcinoma of the ocular region: a review. Surv Ophthalmol. 2005; 50:103–122.21. Deprez M, Uffer S. Clinicopathological features of eyelid skin tumors. A retrospective study of 5504 cases and review of literature. Am J Dermatopathol. 2009; 31:256–262.22. Stewart CL, Novoa RA, Seykora JT. Tumors of the epidermal appendages. In : Elder DE, Elenitsas R, Rosenbach M, Murphy GF, Rubin AI, Xu X, editors. Lever's Histopathology of the Skin. 11th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2014. p. 1040–1115.23. Kim MS, Park OJ, Won CH, Chang SE, Lee MW, Choi JH, Moon KC. A case of Muir-Torre syndrome: extra-ocular sebaceous carcinoma in a patient with breast cancer. Korean J Dermatol. 2010; 48:696–699.24. Lee JH, Yun SJ, Kim SJ, Lee SC, Won YH, Lee JB. A case of sebaceous carcinoma on the extraocular area associated with B-cell lymphoma, esophageal cancer and gastric cancer: a case of Muir-Torre syndrome. Korean J Dermatol. 2007; 45:702–705.25. Rao NA, Hidayat AA, McLean IW, Zimmerman LE. Sebaceous carcinomas of the ocular adnexa: a clinicopathologic study of 104 cases, with five-year follow-up data. Hum Pathol. 1982; 13:113–122.26. Calonje JE, Brenn T, Lazar A, McKee PH. Mckee's Pathology of the Skin. 4th ed. Edinburgh: Elsevier/Saunders;2012.27. Mulay K, Aggarwal E, White VA. Periocular sebaceous gland carcinoma: a comprehensive review. Saudi J Ophthalmol. 2013; 27:159–165.28. Kuzel P, Metelitsa AI, Dover DC, Salopek TG. Epidemiology of sebaceous carcinoma in Alberta, Canada, from 1988 to 2007. J Cutan Med Surg. 2012; 16:417–423.29. Blake PW, Bradford PT, Devesa SS, Toro JR. Cutaneous appendageal carcinoma incidence and survival patterns in the United States: a population-based study. Arch Dermatol. 2010; 146:625–632.30. Bailet JW, Zimmerman MC, Arnstein DP, Wollman JS, Mickel RA. Sebaceous carcinoma of the head and neck. Case report and literature review. Arch Otolaryngol Head Neck Surg. 1992; 118:1245–1249.31. Saito A, Tsutsumida A, Furukawa H, Saito N, Yamamoto Y. Sebaceous carcinoma of the eyelids: a review of 21 cases. J Plast Reconstr Aesthet Surg. 2008; 61:1328–1331.32. Edge SB. American Joint Committee on Cancer. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer;2010.33. Esmaeli B, Nasser QJ, Cruz H, Fellman M, Warneke CL, Ivan D. American Joint Committee on Cancer T category for eyelid sebaceous carcinoma correlates with nodal metastasis and survival. Ophthalmology. 2012; 119:1078–1082.34. Font RL. Eyelids and lacrimal drainage system. In : Spencer WH, editor. Ophthalmic Pathology: an Atlas and Textbook. 3rd ed. Philadelphia, PA: WB Saunders;1985. p. 2169–2214.35. Jakobiec FA, Mendoza PR. Eyelid sebaceous carcinoma: clinicopathologic and multiparametric immunohistochemical analysis that includes adipophilin. Am J Ophthalmol. 2014; 157:186–208.e2.36. Pereira PR, Odashiro AN, Rodrigues-Reyes AA, Correa ZM, de Souza Filho JP, Burnier MN Jr. Histopathological review of sebaceous carcinoma of the eyelid. J Cutan Pathol. 2005; 32:496–501.37. Mulay K, White VA, Shah SJ, Honavar SG. Sebaceous carcinoma: clinicopathologic features and diagnostic role of immunohistochemistry (including androgen receptor). Can J Ophthalmol. 2014; 49:326–332.38. Sinard JH. Immunohistochemical distinction of ocular sebaceous carcinoma from basal cell and squamous cell carcinoma. Arch Ophthalmol. 1999; 117:776–783.39. Hou JL, Killian JM, Baum CL, Otley CC, Roenigk RK, Arpey CJ, Weaver AL, Brewer JD. Characteristics of sebaceous carcinoma and early outcomes of treatment using Mohs micrographic surgery versus wide local excision: an update of the Mayo Clinic experience over the past 2 decades. Dermatol Surg. 2014; 40:241–246.40. Berlin AL, Amin SP, Goldberg DJ. Extraocular sebaceous carcinoma treated with Mohs micrographic surgery: report of a case and review of literature. Dermatol Surg. 2008; 34:254–257.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extraocular Sebaceous Carcinoma
- Sebaceous carcinoma of the eyelids: frequent expression of c-erbB-2 oncoprotein
- A Case of Well-differentiated Sebaceous Carcinoma
- A Case of Sebaceous Carcinoma of the Submandibular Gland
- Two Cases of Sebaceous Carcinoma Developed on the Unusual Site: A Case of Muir-Torre Syndrome