J Korean Med Sci.
2017 Aug;32(8):1288-1294. 10.3346/jkms.2017.32.8.1288.
Prophylactic versus Early Rescue Surfactant Treatment in Preterm Infants Born at Less than 30 Weeks Gestation or with Birth Weight Less than or Equal 1,250 Grams
- Affiliations
-
- 1Department of Pediatrics, Hallym University Kangnam Sacred Heart Hospital, Hallym University School of Medicine, Seoul, Korea.
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wonspark@skku.edu
- 3Department of Pediatrics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University School of Medicine, Bucheon, Korea.
- 4Department of Pediatrics, Chungbuk National University Hospital, Cheongju, Korea.
- KMID: 2439463
- DOI: http://doi.org/10.3346/jkms.2017.32.8.1288
Abstract
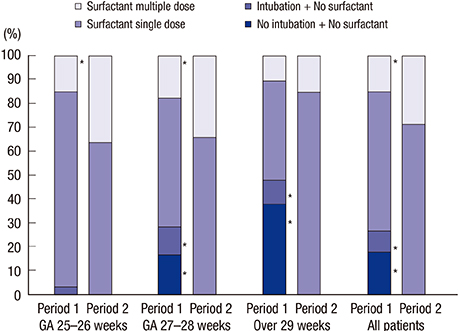
- Prophylactic surfactant is known to be effective to reduce chronic lung disease in preterm infants compared with rescue surfactant treatment. In Korea, early prophylactic surfactant therapy was introduced in 2011. However, recently, the increased utilization of antenatal steroids and early stabilization through continuous positive airway pressure (CPAP) in the delivery room may have changed the risks and benefits of prophylactic surfactant therapy of infants at high risk of respiratory distress syndrome (RDS). We compared the effects and safety of prophylactic surfactant therapy (within 30 minutes after birth) and early selective surfactant therapy (within 3 hours after birth) in preterm infants born at < 30 weeks gestation or with birth weight ≤ 1,250 g. The clinical data of 193 infants in period 1 (from 2008 to 2010, early selective surfactant therapy group) were collected retrospectively; those of 191 infants in period 2 (from 2012 to 2014, prophylactic surfactant therapy group) were collected prospectively. Compared to period 1, the rate of intubation and surfactant use were significantly increased in period 2. The use of multiple doses of surfactant in period 2 was significantly increased compared with period 1. Despite more invasive and aggressive management in period 2, there was no difference in the duration of mechanical ventilation, the incidence of bronchopulmonary dysplasia (BPD) or death, and the risk of other adverse neonatal outcomes between the 2 groups. In conclusion, the benefit of prophylactic surfactant therapy in infants treated under current practices is no longer clear compared to early selective surfactant therapy.
MeSH Terms
Figure
Reference
-
1. Polin RA, Carlo WA; Committee on Fetus and Newborn. American Academy of Pediatrics. Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics. 2014; 133:156–163.2. Halliday HL. Surfactants: past, present and future. J Perinatol. 2008; 28:Suppl 1. S47–S56.3. Engle WA; American Academy of Pediatrics Committee on Fetus and Newborn. Surfactant-replacement therapy for respiratory distress in the preterm and term neonate. Pediatrics. 2008; 121:419–432.4. Bahadue FL, Soll R. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev. 2012; 11:CD001456.5. Stevens TP, Harrington EW, Blennow M, Soll RF. Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev. 2007; CD003063.6. Soll RF, Morley CJ. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2001; CD000510.7. Kresch MJ, Clive JM. Meta-analyses of surfactant replacement therapy of infants with birth weights less than 2000 grams. J Perinatol. 1998; 18:276–283.8. Kendig JW, Notter RH, Cox C, Reubens LJ, Davis JM, Maniscalco WM, Sinkin RA, Bartoletti A, Dweck HS, Horgan MJ, et al. A comparison of surfactant as immediate prophylaxis and as rescue therapy in newborns of less than 30 weeks’ gestation. N Engl J Med. 1991; 324:865–871.9. Rojas-Reyes MX, Morley CJ, Soll R. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2012; CD000510.10. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–1729.11. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92:529–534.12. The Committee for the Classification of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. Arch Ophthalmol. 1984; 102:1130–1134.13. Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986; 33:179–201.14. Sandri F, Plavka R, Ancora G, Simeoni U, Stranak Z, Martinelli S, Mosca F, Nona J, Thomson M, Verder H, et al. Prophylactic or early selective surfactant combined with nCPAP in very preterm infants. Pediatrics. 2010; 125:e1402–e1409.15. St John EB, Carlo WA. Respiratory distress syndrome in VLBW infants: changes in management and outcomes observed by the NICHD Neonatal Research Network. Semin Perinatol. 2003; 27:288–292.16. Chang LY, McCurnin D, Yoder B, Shaul PW, Clyman RI. Ductus arteriosus ligation and alveolar growth in preterm baboons with a patent ductus arteriosus. Pediatr Res. 2008; 63:299–302.17. Clyman R, Cassady G, Kirklin JK, Collins M, Philips JB 3rd. The role of patent ductus arteriosus ligation in bronchopulmonary dysplasia: reexamining a randomized controlled trial. J Pediatr. 2009; 154:873–876.18. Mirea L, Sankaran K, Seshia M, Ohlsson A, Allen AC, Aziz K, Lee SK, Shah PS; Canadian Neonatal Network. Treatment of patent ductus arteriosus and neonatal mortality/morbidities: adjustment for treatment selection bias. J Pediatr. 2012; 161:689–694.e1.19. Sakonidou S, Dhaliwal J. The management of neonatal respiratory distress syndrome in preterm infants (European Consensus Guidelines--2013 update). Arch Dis Child Educ Pract Ed. 2015; 100:257–259.20. Kim SM, Park YJ, Chung SH, Choi YS, Kim CH, Bae CW. Early prophylactic versus late selective use of surfactant for respiratory distress syndrome in very preterm infants: a collaborative study of 53 multi-center trials in Korea. J Korean Med Sci. 2014; 29:1126–1131.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prophylactic Administration of Surfactant with Nasal Continuous Positive Airway Pressure in Preterm Infants with Gestational Age Less than 30 Weeks
- Is Less Invasive Surfactant Administration Better than INtubation-SURfactant-Extubation for Prophylactic Surfactant Replacement Therapy?
- Comparison of Outcomes between Prophylactic and Rescue Therapy of Surfactant in Premature Infants
- Factors associated with the growth of preterm infants
- Comparative observational study of aminophylline with prophylactic and therapeutic uses for clinical outcomes in preterm infants