Korean J Adult Nurs.
2019 Feb;31(1):78-88. 10.7475/kjan.2019.31.1.78.
A Prediction Model for Physical Activity Adherence for Secondary Prevention among Patients with Coronary Artery Disease
- Affiliations
-
- 1Assistant Professor, Department of Nursing, Wonkwang University, Ilsan, Korea. mihwon7729@wku.ac.kr
- 2Professor, College of Nursing, Ewha Womans University, Seoul, Korea.
- KMID: 2438763
- DOI: http://doi.org/10.7475/kjan.2019.31.1.78
Abstract
- PURPOSE
The purpose of this study was to construct and test a predictive model for physical activity adherence for secondary prevention among patients with coronary artery disease.
METHODS
Two hundred and eighty-two patients with coronary artery disease were recruited at cardiology outpatient clinics in four general hospitals and the data collection was conducted from September 1 to October 19, 2015.
RESULTS
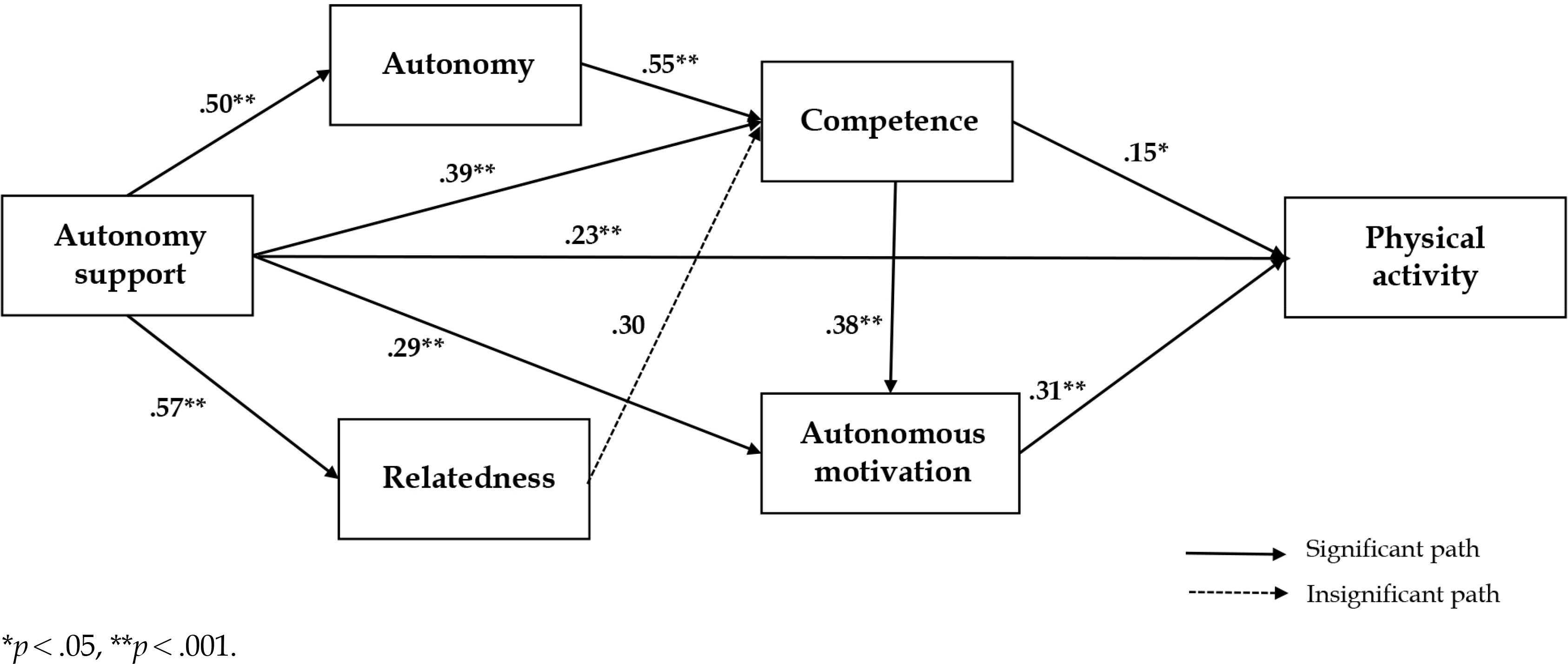
The model fit indices for the final hypothetical model satisfied the recommended levels: χ2/dF=0.77, adjusted goodness of fit index=.98, comparative fit index=1.00, normal fit index=1.00, incremental fit index=1.00, standardized root mean residual=.01, root mean square error of approximation=.03. Autonomy support (β=.50), competence (β=.27), and autonomous motivation (β=.31) had significant direct effects on physical activity adherence for secondary prevention among patients with coronary artery disease. This variable explained 35.1% of the variance in physical activity adherence.
CONCLUSION
This study showed that autonomy support from healthcare providers plays a key role in promoting physical activity adherence for secondary prevention among patients with coronary artery disease. The findings suggest that developing intervention programs to increase feelings of competence and autonomous motivation through autonomy support from healthcare providers are needed to promote physical activity adherence for secondary prevention among patients with coronary artery disease.
MeSH Terms
Figure
Reference
-
1. Statistics Korea. 2014 annual report on the cause of death statistics [Internet]. Seoul: Statistics Korea;2015. [cited 2016 March 10]. Available from:. http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1012.2. Myerburg RJ, Junttila MJ. Sudden cardiac death caused by coronary heart disease. Circulation. 2012; 125(8):1043–52. https://doi.org/10.1161/CIRCULATIONAHA.111.023846.
Article3. Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology European Heart Journal. 2013; 34(38):2949–3003. https://doi.org/10.1093/eurheartj/eht296.4. Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Miller NH, Hub-bard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014; 63:2960–84. https://doi.org/10.1016/j.jacc.2013.11.003. https://doi.org/10.1016/j.jacc.2013.11.003.5. Aliabad HO, Vafaeinasab M, Morowatisharifabad MA, Afsha-ni SA, Firoozabadi MG, Forouzannia SK. Maintenance of physical activity and exercise capacity after rehabilitation in coronary heart disease: a randomized controlled trial. Global Journal of Health Science. 2014; 6(6):198–208. https://doi.org/10.5539/gjhs.v6n6p198.
Article6. Darden D, Richardson C, Jackson EA. Physical activity and exercise for secondary prevention among patients with cardiovascular disease. Current Cardiovascular Risk Reports. 2013; 7(6):411–6. https://doi.org/10.1007/s12170-013-0354-5.
Article7. Winzer EB, Woitek F, Linke A. Physical activity in the prevention and treatment of coronary artery disease. Journal of the American Heart Association. 2018; 7(4):e007725. https://doi.org/10.1161/JAHA.117.007725.
Article8. Goblirsch G, Bershow S, Cummings K, Hayes R, Kokoszka M, Lu Y, et al. Institute for clinical systems improvement. Stable coronary artery disease. [Internet]. Institute for Clinical Systems Improvement (ICSI): Bloomington;2013. [cited 2015, October, 16]. Available from:. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.658.3632&rep=rep1&type=pdf.9. Janssen V, De Gucht V, Dusseldorp E, Maes S. Lifestyle modification programmes for patients with coronary heart disease: a systematic review and metaanalysis of randomized controlled trials. European Journal of Preventive Cardiology. 2013; 20(4):620–40. https://doi.org/10.1177/2047487312462824.
Article10. Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of "ideal cardiovascular health" in a communitybased population: the heart strategies concentrating on risk evaluation (Heart SCORE) study. Circulation. 2011; 123(8):850–7. https://doi.org/10.1161/CIRCULATIONAHA.110.980151.11. Driscoll A, Beltrame J, Beauchamp A, Morgan C, Weekes A, Tonkin A. Reducing risk in coronary artery disease. Are Aus-tralian patients in general practice achieving targets? The coronary artery disease in general practice study (CADENCE). Internal Medicine Journal. 2013; 43(5):526–31. https://doi.org/10.1111/j.1445-5994.2012.02929.x.
Article12. Dullaghan L, Lusk L, McGeough M, Donnelly P, Herity N, Fitzsimons D. 'I am still a bit unsure how much of a heart at-tack it really was!' Patients presenting with non ST elevation myocardial infarction lack understanding about their illness and have less motivation for secondary prevention. European Journal of Cardiovascular Nursing. 2014; 13(3):270–6. https://doi.org/10.1177/1474515113491649.
Article13. Won MH, Son Y-J. Perceived social support and physical activity among patients with coronary artery disease. Western Journal of Nursing Research. 2017; 39(12):1606–23. https://doi.org/10.1177/0193945916678374.
Article14. Shane N, Fortier MS, Strachan SM, Blanchard CM. Testing and integrating self- determination theory and self-efficacy theory in a physical activity context. Canadian Psychology/Psychologie Canadienne. 2012; 53(4):319–27. https://doi.org/10.1037/a0030280.15. Michall M, Simon P, Gori T, König J, Wild PS, Wiltink J, et al. Psychodymanic motivation and training program (PMT) for the secondary prevention in patients with stable coronary heart disease: study protocol for randomized controlled trial of feasibility and effects. Trials. 2013; 14(1):314. https://doi.org/10.1186/1745-6215-14-314.16. Yates BC, Kosloski K, Kercher K, Dizona P. Testing a model of physical and psychological recovery after a cardiac event. Western Journal of Nursing Research. 2010; 32(7):871–93. https://doi.org/10.1177/0193945910362067.
Article17. Petosa RL, Holtz B. Flow for exercise adherence: testing an in-trinsic model of health behavior. American Journal of Health Education. 2013; 44(5):273–7. https://doi.org/10.1080/19325037.2013.811364.
Article18. Slovinec D'Angelo ME, Pelletier LG, Reid RD, Huta V. The roles of self-efficacy and motivation in the prediction of short- and longterm adherence to exercise among patients with coronary heart disease. Health Psychology. 2014; 33(11):1344–53. https://doi.org/10.1037/hea0000094.19. Deci EL, Ryan RM. The "what" and the "why" of goal pursuits: human needs and the self-determination of behavior. Psychological Inquiry. 2000; 11(4):227–68. https://doi.org/10.1207/S15327965PLI1104_01.20. Fortier MS, Williams GC, Sweet SN, Patrick H. Self-determi-nation theory: process models for health behavior change. DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research. San Fran-cisco, CA: Jossey-Bass;;2009. p. 157–83.21. Sweet SN, Tulloch H, Fortier MS, Pipe AL, Reid RD. Patterns of motivation and ongoing exercise activity in cardiac rehabilitation settings: a 24-month exploration from the TEACH Study. Annals of Behavioral Medicine. 2011; 42(1):55–63. https://doi.org/10.1007/s12160-011-9264-2.
Article22. Koponen AM, Simonsen N, Suominen S. Success in increasing physical activity (PA) among patients with type 2 diabetes: a self-determination theory perspective. Health Psychology and Behavioral Medicine. 2018; 6(1):104–19. https://doi.org/10.1080/21642850.2018.1462707. https://doi.org/10.1080/21642850.2018.1462707.
Article23. Xu L, Ryu S, Goong H. Gender differences in predictors of health behaviors modification among patients with cardiovascular disease. The Journal of the Korea Contents Association. 2015; 15(3):280–9. https://doi.org/10.5392/JKCA.2015.15.03.280.
Article24. Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2012; 9(1):78. https://doi.org/10.1186/1479-5868-9-78.
Article25. Karimi A, Ahmadi H, Davoodi S, Movahedi N, Marzban M, Abbasi K, et al. Factors affecting postoperative morbidity and mortality in isolated coronary artery bypass graft surgery. Surgical Today. 2008; 38(10):890–8. https://doi.org/10.1007/s00595-007-3733-z.
Article26. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987; 40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8. https://doi.org/10.1016/0021-9681(87)90171-8.
Article27. Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998; 21(10):1644–51. https://doi.org/10.2337/diacare.21.10.1644.
Article28. Lee M, Kim A. Development and construct validation of the basic psychological needs scale for Korean adolescents: based on the self-determination theory. Korean Journal of Social and Personality Psychology. 2008; 22(4):157–74. https://doi.org/10.21193/kjspp.2008.22.4.010.29. Oh JY, Yang YJ, Kim BS, Kang JH. Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. Korean Journal of Family Medicine. 2007; 28(7):532–41.30. Schmitt TA. Current methodological considerations in exploratory and confirmatory factor analysis. Journal of Psycho-educational Assessment. 2011; 29(4):304–21. https://doi.org/10.1177/0734282911406653.
Article31. Bae BR. Structural equation modeling with Amos 21: principles and practice. Seoul: Cheong-Ram Publishing;2014.32. Russell KL, Bray SR. Promoting self-determined motivation for exercise in cardiac rehabilitation: the role of autonomy support. Rehabilitation Psychology. 2010; 55(1):74–80. https://doi.org/10.1037/a0018416.
Article33. Schmidt K, Gensichen J, Petersen JJ, Szecsenyi J, Walther M, Williams G, et al. Autonomy support in primary care-validation of the German version of the Health Care Climate Questionnaire. Journal of Clinical Epidemiology. 2012; 65(2):206–11. https://doi.org/10.1016/j.jclinepi.2011.06.003.
Article34. Sylvester BD, Standage M, Dowd AJ, Martin LJ, Sweet SN, Beauchamp MR. Perceived variety, psychological needs satisfaction and exercise-related well-being. Psychology & Health. 2014; 29(9):1044–61. https://doi.org/10.1080/08870446.2014.907900.
Article35. Rahman RJ, Hudson J, Th⊘gersen-Ntoumani C, Doust JH. Moti-vational processes and well-being in cardiac rehabilitation: a self-determination theory perspective. Psychology, Health & Medicine. 2015; 20(5):518–29. https://doi.org/10.1080/13548506.2015.1017509.
Article36. Duda JL, Williams GC, Ntoumanis N, Daley A, Eves FF, Mutrie N, et al. Effects of a standard provision versus an autonomy supportive exercise referral programme on physical activity, quality of life and well-being indicators: a cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity. 2014; 11(10):1–15. https://doi.org/10.1186/1479-5868-11-10.
Article37. Janssen I, Dugan SA, Karavolos K, Lynch EB, Powell LH. Cor-relates of 15-year maintenance of physical activity in middle- aged women. International Journal of Behavioral Medicine. 2014; 21(3):511–8. https://doi.org/10.1007/s12529-013-9324-z.38. Lee E-H, Park J-W. A structural equation model on health behavior adherence for elders with prehypertension: based on self-determination theory. Journal of Korean Academy of Fundamentals of Nursing. 2012; 19(3):343–52. https://doi.org/10.7739/jkafn.2012.19.3.343.
Article39. Ng JYY, Ntoumanis N, Th⊘gersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, et al. Self-determination theory applied to health contexts: a metaanalysis. Perspectives on Psychological Science. 2012; 7(4):325–40. https://doi.org/10.1177/1745691612447309.40. Visser PL, Hirsch JK. Health behaviors among college students: the influence of future time perspective and basic psychological need satisfaction. Health Psychology and Behavioral Medicine. 2014; 2(1):88–99. https://doi.org/10.1080/21642850.2013.872992.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Research on Adherence for Secondary Prevention in Patients with Coronary Artery Disease in Korea
- Cardiac rehabilitation for patients with coronary artery disease
- Current Progress of Studies of Coronary CT for Risk Prediction of Major Adverse Cardiovascular Event (MACE)
- Mediating Effect of Physical Activity in the Relationship between Depressive Symptoms and Health-related Quality of Life in Patients with Coronary Artery Disease: The 2016 Nationwide Community Health Survey in Korea
- Antiplatelet Agents in High-Risk Patients with Coronary Artery Disease