Korean J Gastroenterol.
2019 Feb;73(2):77-83. 10.4166/kjg.2019.73.2.77.
Functional Dyspepsia
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, Korea. kwonjg@cu.ac.kr
- KMID: 2438706
- DOI: http://doi.org/10.4166/kjg.2019.73.2.77
Abstract
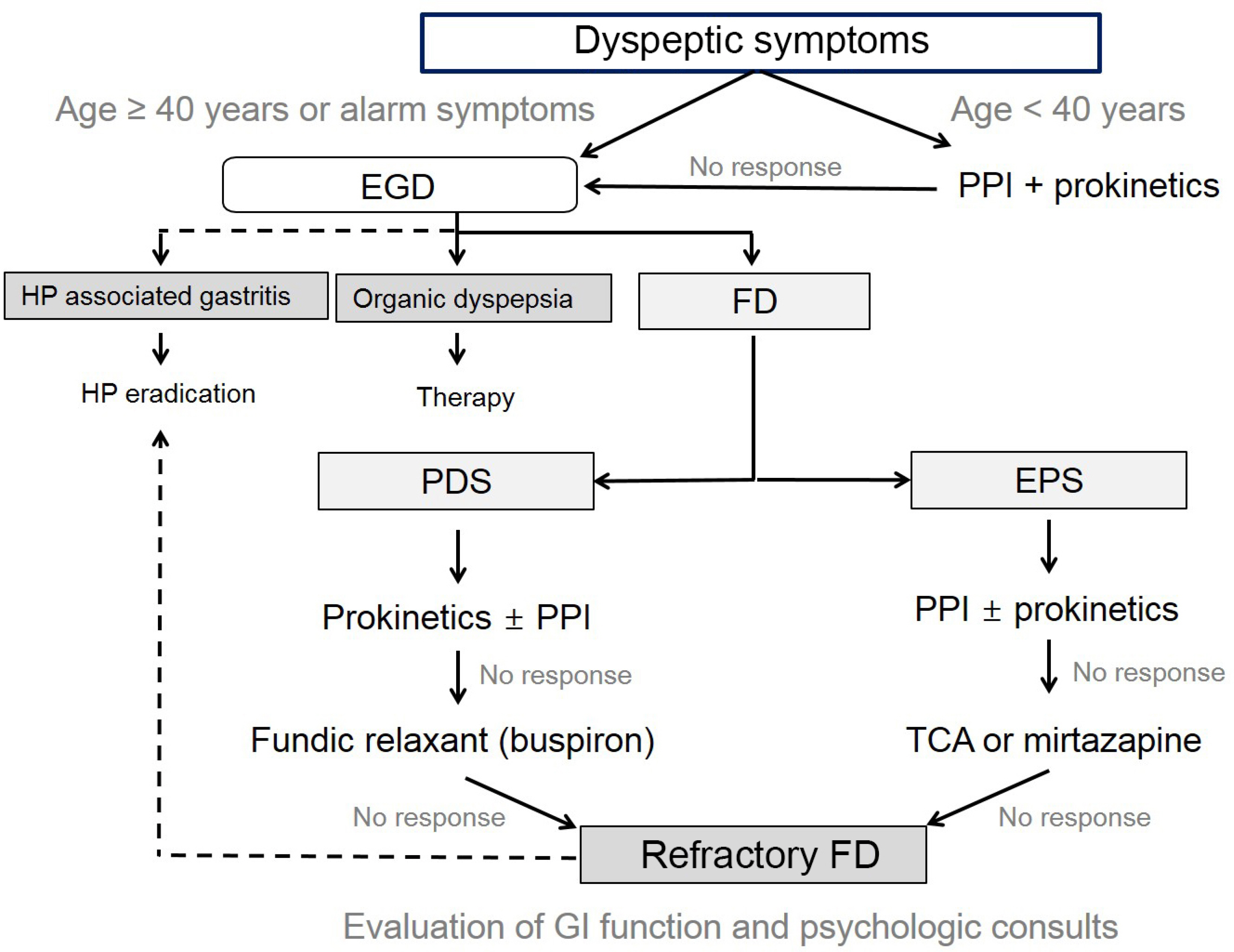
- Dyspepsia is a common problem, and when dyspeptic symptoms develop within a short period of time, organic diseases such as gastroesophageal reflux disease, peptic ulcer diseases, pancreatoduodenal diseases, and gastrointestinal cancers should be suspected. Furthermore, functional dyspepsia (FD) should be considered if chronic or recurrent symptoms persist after eliminating underlying disease. FD is classified as epigastric pain syndrome (EPS) or postprandial distress syndrome (PDS), but these two conditions may overlap. Patients with the EPS subtype can be treated with proton pump inhibitors (PPIs), whereas patients with the PDS subtype may be managed primarily with prokinetics, and patients with EPS and PDS can be co-administered PPIs and prokinetics. Helicobacter pylori eradication therapy can be administered on a test-and-treat basis when PPIs and prokinetics are ineffective or to younger patients with chronic dyspepsia, and tricyclic antidepressants can be used as a secondary treatment because they are effective in patients with the EPS subtype. In addition, because the pathophysiology of FD is diverse, dietary education and stress management are required in addition to medical therapy, and should substantially aid treatment and long-term management. Here, we introduce and summarize recently published guidelines for the treatment of FD.
MeSH Terms
Figure
Cited by 1 articles
-
The Effect of Proton Pump Inhibitor and Prokinetics Combination Therapy for Functional Dyspepsia
Ju Yup Lee
Korean J Gastroenterol. 2021;77(4):149-150. doi: 10.4166/kjg.2021.060.
Reference
-
References
1. Lee H, Jung HK, Huh KC. Functional Dyspepsia Study Group in the Korean Society of Neurogastroenterology and Motility. Current status of functional dyspepsia in Korea. Korean J Intern Med. 2014; 29:156–165.
Article2. Jung HK, Keum BR, Jo YJ, et al. Diagnosis of functional dyspepsia: a systematic review. Korean J Gastroenterol. 2010; 55:296–307.
Article3. Stanghellini V, Chan FK, Hasler WL, et al. Gastroduodenal disorders. Gastroenterology. 2016; 150:1380–1392.
Article4. Jung KW. Understanding the Rome IV: gastroduodenal disorders. Korean J Med. 2017; 92:362–365.
Article5. Moayyedi PM, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N. ACG and CAG clinical guideline: management of dyspepsia. Am J Gastroenterol. 2017; 112:988–1013.
Article6. Li XB, Liu WZ, Ge ZZ, Chen XY, Shi Y, Xiao SD. Helicobacter pylori "test-and-treat" strategy is not suitable for the management of patients with uninvestigated dyspepsia in Shanghai. Scand J Gastroenterol. 2005; 40:1028–1031.7. Liou JM, Lin JT, Wang HP, et al. The optimal age threshold for screening upper endoscopy for uninvestigated dyspepsia in Taiwan, an area with a higher prevalence of gastric cancer in young adults. Gastrointest Endosc. 2005; 61:819–825.
Article8. Chen SL, Gwee KA, Lee JS, et al. Systematic review with metaanalysis: prompt endoscopy as the initial management strategy for uninvestigated dyspepsia in Asia. Aliment Pharmacol Ther. 2015; 41:239–252.
Article9. Miwa H, Kusano M, Arisawa T, et al. Evidence-based clinical practice guidelines for functional dyspepsia. J Gastroenterol. 2015; 50:125–139.
Article10. Miwa H, Ghoshal UC, Fock KM, et al. Asian consensus report on functional dyspepsia. J Gastroenterol Hepatol. 2012; 27:626–641.
Article11. Jee SR, Jung HK, Min BH, et al. Guidelines for the treatment of functional dyspepsia. Korean J Gastroenterol. 2011; 57:67–81.
Article12. Shin CM. Diet and nutritional management in functional gastrointestinal disorder: functional dyspepsia. Korean J Med. 2016; 90:98–104.
Article13. Pinto-Sanchez MI, Yuan Y, Hassan A, Bercik P, Moayyedi P. Proton pump inhibitors for functional dyspepsia. Cochrane Database Syst Rev. 2017; 11:CD011194.
Article14. Lee HH, Jung HK, Choi MG. Guideline recommendation for endpoints used in clinical trials for functional dyspepsia. Korean J Gastroenterol. 2018; 72:170–178.
Article15. Lacy BE, Talley NJ, Locke GR 3rd, et al. Review article: current treatment options and management of functional dyspepsia. Aliment Pharmacol Ther. 2012; 36:3–15.
Article16. Park KH, Pai J, Song DG, et al. Ranitidine-induced anaphylaxis: clinical features, cross-reactivity, and skin testing. Clin Exp Allergy. 2016; 46:631–639.
Article17. Regan LA, Hoffman RS, Nelson LS. Slower infusion of metoclopramide decreases the rate of akathisia. Am J Emerg Med. 2009; 27:475–480.
Article18. Tura P, Erdur B, Aydin B, Turkcuer I, Parlak I. Slow infusion metoclopramide does not affect the improvement rate of nausea while reducing akathisia and sedation incidence. Emerg Med J. 2012; 29:108–112.
Article19. Shin HW, Kim MJ, Kim JS, Lee MC, Chung SJ. Levosulpiride-induced movement disorders. Mov Disord. 2009; 24:2249–2253.
Article20. Bang CS, Kim JH, Baik GH, et al. Mosapride treatment for functional dyspepsia: a metaanalysis. J Gastroenterol Hepatol. 2015; 30:28–42.
Article21. Yoon H, Lee DH, Lee YH, et al. Efficacy and safety of UI05MSP015CT in functional dyspepsia: a randomized, controlled trial. Gut Liver. 2018; 12:516–522.
Article22. Yang YJ, Bang CS, Baik GH, et al. Prokinetics for the treatment of functional dyspepsia: bayesian network metaanalysis. BMC Gastroenterol. 2017; 17:83.
Article23. Jung HK, Lee KJ, Choi MG, et al. Efficacy of DA-9701 (Motilitone) in functional dyspepsia compared to pantoprazole: a multicenter, randomized, double-blind, non-inferiority study. J Neurogastroenterol Motil. 2016; 22:254–263.
Article24. Pittayanon R, Yuan Y, Bollegala NP, et al. Prokinetics for functional dyspepsia: a systematic review and metaanalysis of randomized control trials. Am J Gastroenterol. 2019; 114:233–243.
Article25. Suzuki H, Moayyedi P. Helicobacter pylori infection in functional dyspepsia. Nat Rev Gastroenterol Hepatol. 2013; 10:168–174.
Article26. Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015; 64:1353–1367.27. Liu WZ, Xie Y, Lu H, et al. Fifth Chinese national consensus report on the management of Helicobacter pylori infection. Helicobacter. 2018; 23:e12475.28. Mahachai V, Vilaichone RK, Pittayanon R, et al. Helicobacter pylori management in ASEAN: the Bangkok consensus report. J Gastroenterol Hepatol. 2018; 33:37–56.29. Mazzoleni LE, Sander GB, Francesconi CF, et al. Helicobacter pylori eradication in functional dyspepsia: HEROES trial. Arch Intern Med. 2011; 171:1929–1936.30. Lee SY. Endoscopic gastritis, serum pepsinogen assay, and Helicobacter pylori infection. Korean J Intern Med. 2016; 31:835–844.
Article31. Lan L, Yu J, Chen YL, et al. Symptom-based tendencies of Helicobacter pylori eradication in patients with functional dyspepsia. World J Gastroenterol. 2011; 17:3242–3247.32. Hooi JKY, Lai WY, Ng WK, et al. Global prevalence of Helicobacter pylori infection: systematic review and metaanalysis. Gastroenterology. 2017; 153:420–429.
Article33. Talley NJ, Locke GR, Saito YA, et al. Effect of amitriptyline and escitalopram on functional dyspepsia: a multicenter, randomized controlled study. Gastroenterology. 2015; 149:340–349.e2.
Article34. Lu Y, Chen M, Huang Z, Tang C. Antidepressants in the treatment of functional dyspepsia: a systematic review and metaanalysis. PLoS One. 2016; 11:e0157798.
Article35. Tack J, Ly HG, Carbone F, et al. Efficacy of mirtazapine in patients with functional dyspepsia and weight loss. Clin Gastroenterol Hepatol. 2016; 14:385–392.e4.
Article36. Tack J, Janssen P, Masaoka T, Farré R, Van Oudenhove L. Efficacy of buspirone, a fundus-relaxing drug, in patients with functional dyspepsia. Clin Gastroenterol Hepatol. 2012; 10:1239–1245.
Article37. Matsueda K, Hongo M, Tack J, Saito Y, Kato H. A placebo-controlled trial of acotiamide for meal-related symptoms of functional dyspepsia. Gut. 2012; 61:821–828.
Article38. Jaafar MH, Safi SZ, Tan MP, Rampal S, Mahadeva S. Efficacy of rebamipide in organic and functional dyspepsia: a systematic review and metaanalysis. Dig Dis Sci. 2018; 63:1250–1260.
Article39. Holtmann G, Gschossmann J, Karaus M, et al. Randomised double-blind comparison of simethicone with cisapride in functional dyspepsia. Aliment Pharmacol Ther. 1999; 13:1459–1465.
Article40. Holtmann G, Gschossmann J, Mayr P, Talley NJ. A randomized placebo-controlled trial of simethicone and cisapride for the treatment of patients with functional dyspepsia. Aliment Pharmacol Ther. 2002; 16:1641–1648.
Article41. Gudjónsson H, Oddsson E, Björnsson S, et al. Efficacy of sucralfate in treatment of non-ulcer dyspepsia. A double-blind placebo-controlled study. Scand J Gastroenterol. 1993; 28:969–972.
Article42. Kairaluoma MI, Hentilae R, Alavaikko M, et al. Sucralfate versus placebo in treatment of non-ulcer dyspepsia. Am J Med. 1987; 83:51–55.
Article43. Moayyedi P, Soo S, Deeks J, et al. Systematic review: antacids, H2-receptor antagonists, prokinetics, bismuth and sucralfate therapy for non-ulcer dyspepsia. Aliment Pharmacol Ther. 2003; 17:1215–1227.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Helicobacter pylori infection in functional dyspepsia
- The relationship between functional dyspepsia and family function
- The Relationship between Obstructive Sleep Apnea and Functional Dyspepsia
- Duodenal Microbiome and Its Clinical Implications in Functional Dyspepsia
- What Is the Difference Between Helicobacter pylori-Associated Dyspepsia and Functional Dyspepsia?