Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide populationbased study
- Affiliations
-
- 1Department of Internal Medicine, Changhua Christian Hospital, Changhua, Taiwan. shuchenwei@ntu.edu.tw
- 2Department of Endoscopy Center, Changhua Christian Hospital, Changhua, Taiwan.
- 3Department of Internal Medicine, Far Eastern Memorial Hospital, New Taipei, Taiwan.
- 4Department of Integrated Diagnostics & Therapeutics, National Taiwan University Hospital, Taipei, Taiwan.
- 5Department of Medical Research, National Taiwan University Hospital, Taipei, Taiwan.
- 6Department of Public Health, National Taiwan University, Taipei, Taiwan.
- 7Department of Oncology, National Taiwan University Hospital, Taipei, Taiwan, Taiwan.
- 8Department of Internal Medicine, National Taiwan University Hospital, Taipei, Taiwan, Taiwan.
- 9Department of Inflammatory Bowel Disease Clinical and Study Integrated Center, National Taiwan University Hospital, Taipei, Taiwan.
- KMID: 2438443
- DOI: http://doi.org/10.5217/ir.2018.00096
Abstract
- BACKGROUND/AIMS
Incidences of inflammatory bowel disease (IBD), ulcerative colitis (UC), and Crohn's disease (CD), have been increasing in Asia. In this study, we report the relevant clinical characteristics and determined the epidemiological trend of IBD in Taiwan from 2001 to 2015.
METHODS
A retrospective study was conducted to analyze data recorded from January 2001 through December 2015 in the registered database compiled by the National Health Insurance and provided by the Ministry of Health and Welfare, Taiwan.
RESULTS
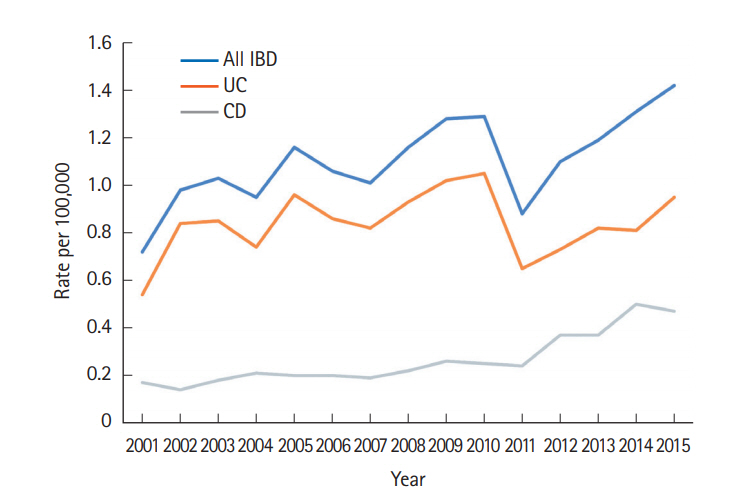
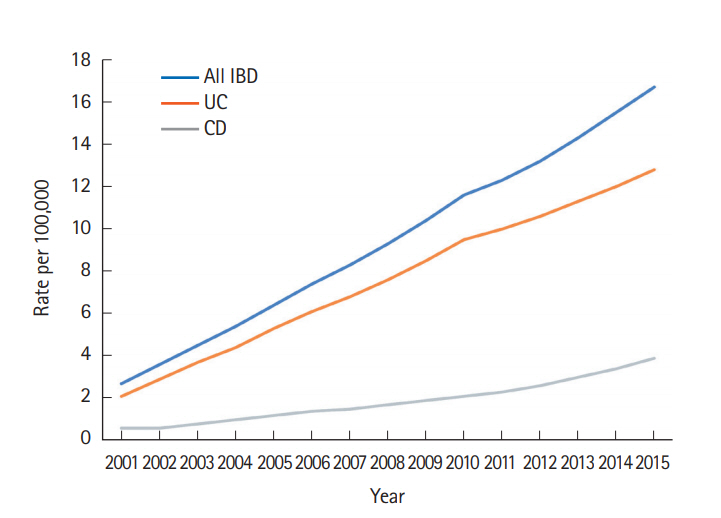
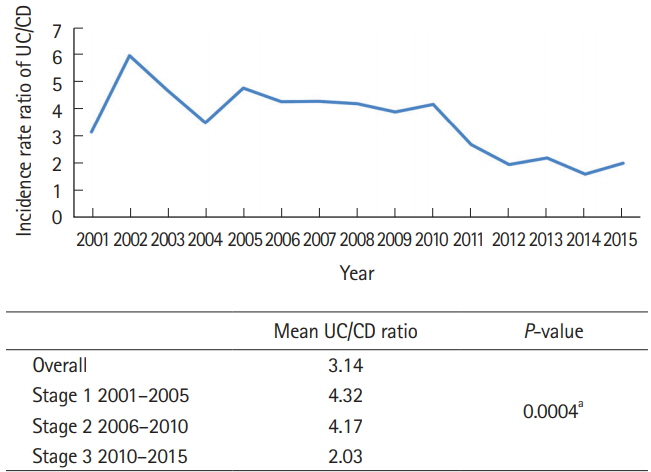
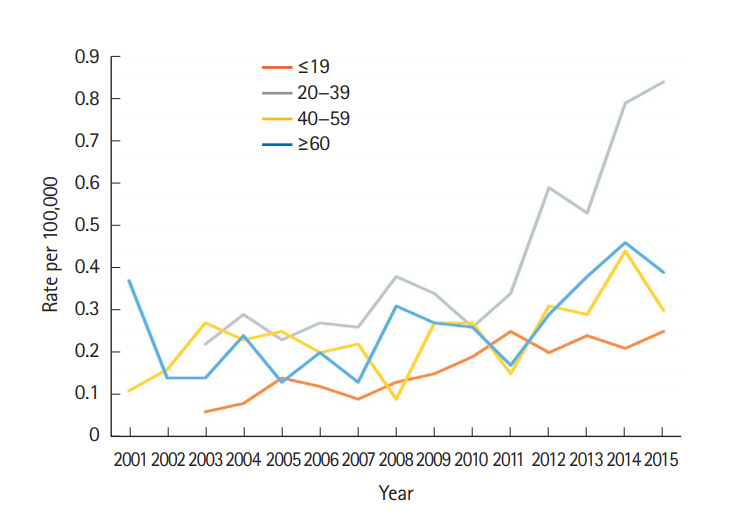
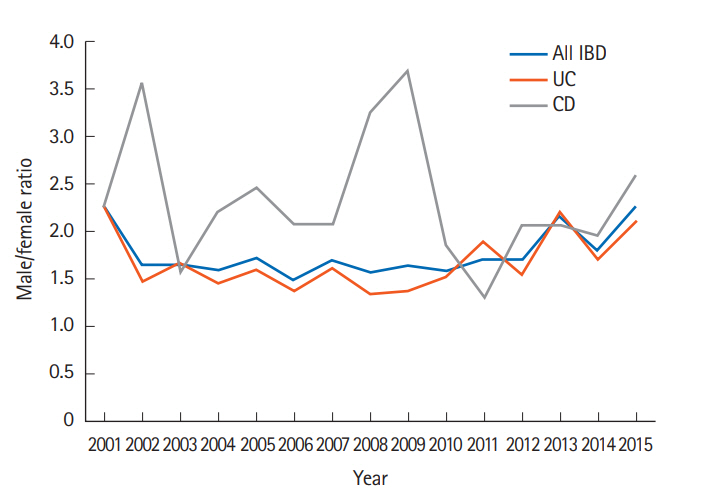
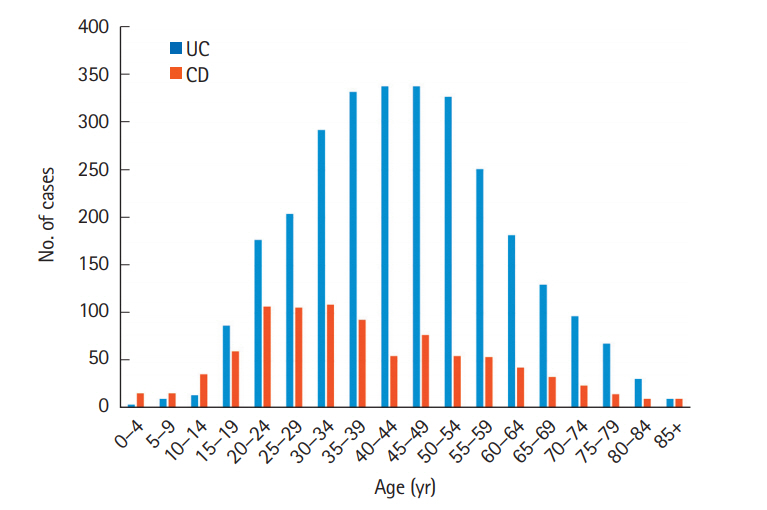
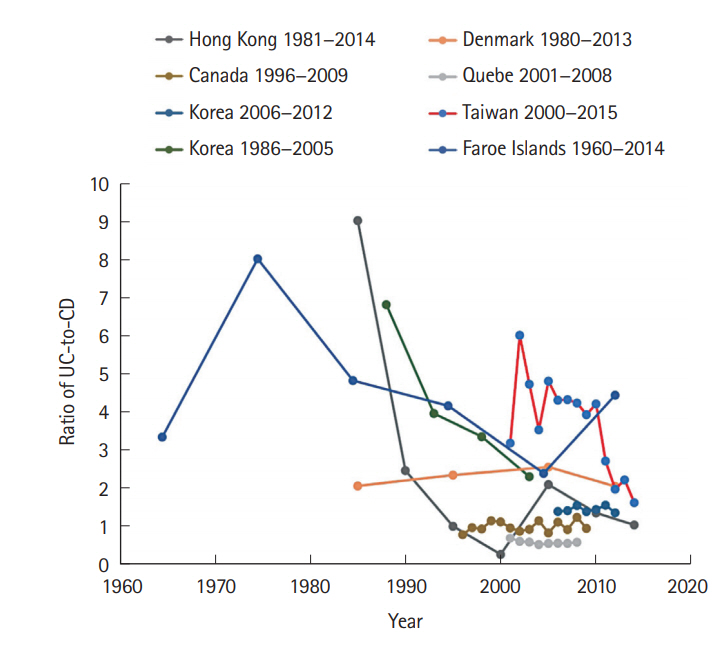
A total of 3,806 patients with catastrophic IBD illness were registered from 2001 to 2015 in Taiwan (CD, 919; UC, 2,887). The crude incidence of CD increased from 0.17/100,000 in 2001 to 0.47/100,000 in 2015, whereas that of UC increased from 0.54/100,000 in 2001 to 0.95/100,000 in 2015. The prevalence of CD increased from 0.6/100,000 in 2001 to 3.9/100,000 in 2015, whereas that of UC increased from 2.1/100,000 in 2001 to 12.8/100,000 in 2015. The male-to-female ratio in the study sample was 2.19 for CD and 1.62 for UC. The median age of those registered with CD was lower than that of those registered for UC: 38.86 and 44.86 years, respectively. A significantly greater increase in CD incidence rate was identified among 20 to 39-year-old compared with other age groups.
CONCLUSIONS
Using Taiwan's nationwide insurance database, we determined that the number of patients with CD increased more rapidly during the study period than the number of patients with UC, especially among age 20 to 39-year-old, resulting in a decreased UC-to-CD ratio.
Keyword
MeSH Terms
Figure
Cited by 12 articles
-
SARS-CoV-2 Vaccination for Adult Patients with Inflammatory Bowel Disease: Expert Consensus Statements by KASID
Yoo Jin Lee, Seong-Eun Kim, Yong Eun Park, Ji Young Chang, Hyun Joo Song, Duk Hwan Kim, Young Joo Yang, Byung Chang Kim, Jae Gon Lee, Hee Chan Yang, Miyoung Choi, Seung-Jae Myung
Korean J Gastroenterol. 2021;78(2):117-128. doi: 10.4166/kjg.2021.110.Comparison of Real-World Outcomes of Infliximab versus Adalimumab in Biologic-Naïve Korean Patients with Ulcerative Colitis: A Population-Based Study
Minkyung Han, Yoon Suk Jung, Jae Hee Cheon, Sohee Park
Yonsei Med J. 2020;61(1):48-55. doi: 10.3349/ymj.2020.61.1.48.Can vitamin D supplementation help control inflammation in inflammatory bowel disease beyond its classical role in bone health?
Sung Wook Hwang
Intest Res. 2019;17(2):157-159. doi: 10.5217/ir.2019.00038.Association of young age and male sex with primary sclerosing cholangitis in Taiwanese patients with inflammatory bowel disease
Meng-Tzu Weng, I-Lun Shih, Chien-Chih Tung, Yew-Loong Leong, Ming-Jium Shieh, Cheng-Yi Wang, Jau-Min Wong, Yen-Hsuan Ni, Shu-Chen Wei
Intest Res. 2022;20(2):224-230. doi: 10.5217/ir.2021.00042.SARS-CoV-2 vaccination for adult patients with inflammatory bowel disease: expert consensus statement by KASID
Yoo Jin Lee, Seong-Eun Kim, Yong Eun Park, Ji Young Chang, Hyun Joo Song, Duk Hwan Kim, Young Joo Yang, Byung Chang Kim, Jae Gon Lee, Hee Chan Yang, Miyoung Choi, Seung-Jae Myung
Intest Res. 2022;20(2):171-183. doi: 10.5217/ir.2021.00098.Update on the epidemiology of inflammatory bowel disease in Asia: where are we now?
Sang Hyoung Park
Intest Res. 2022;20(2):159-164. doi: 10.5217/ir.2021.00115.Clinical outcomes and predictors of response for adalimumab in patients with moderately to severely active ulcerative colitis: a KASID prospective multicenter cohort study
Seung Yong Shin, Soo Jung Park, Young Kim, Jong Pil Im, Hyo Jong Kim, Kang-Moon Lee, Ji Won Kim, Sung-Ae Jung, Jun Lee, Sang-Bum Kang, Sung Jae Shin, Eun Sun Kim, You Sun Kim, Tae Oh Kim, Hyun-Soo Kim, Dong Il Park, Hyung Kil Kim, Eun Soo Kim, Young-Ho Kim, Do Hyun Kim, Dennis Teng, Jong-Hwa Kim, Wonyong Kim, Chang Hwan Choi
Intest Res. 2022;20(3):350-360. doi: 10.5217/ir.2021.00049.Natural history of inflammatory bowel disease: a comparison between the East and the West
Eun Mi Song, Suk-Kyun Yang
Intest Res. 2022;20(4):418-430. doi: 10.5217/ir.2021.00104.Treatment of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Eun Mi Song, Soo-Young Na, Sung Noh Hong, Siew Chien Ng, Tadakazu Hisamatsu, Byong Duk Ye
Intest Res. 2023;21(3):339-352. doi: 10.5217/ir.2022.00135.The Prevalence and Risk Factors of
Clostridioides difficile Infection in Inflammatory Bowel Disease: 10-Year South Korean Experience Based on the National Database
Eun Mi Song, Arum Choi, Sukil Kim, Sung Hoon Jung
J Korean Med Sci. 2023;38(47):e359. doi: 10.3346/jkms.2023.38.e359.Management of ulcerative colitis in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease updated in 2023
Hsu-Heng Yen, Jia-Feng Wu, Horng-Yuan Wang, Ting-An Chang, Chung-Hsin Chang, Chen-Wang Chang, Te-Hsin Chao, Jen-Wei Chou, Yenn-Hwei Chou, Chiao-Hsiung Chuang, Wen-Hung Hsu, Tzu-Chi Hsu, Tien-Yu Huang, Tsung-I Hung, Puo-Hsien Le, Chun-Che Lin, Chun-Chi Lin, Ching-Pin Lin, Jen-Kou Lin, Wei-Chen Lin, Yen-Hsuan Ni, Ming-Jium Shieh, I-Lun Shih, Chia-Tung Shun, Tzung-Jiun Tsai, Cheng-Yi Wang, Meng-Tzu Weng, Jau-Min Wong, Deng-Chyang Wu, Shu-Chen Wei
Intest Res. 2024;22(3):213-249. doi: 10.5217/ir.2023.00050.Management of Crohn’s disease in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease updated in 2023
Jia-Feng Wu, Hsu-Heng Yen, Horng-Yuan Wang, Ting-An Chang, Chung-Hsin Chang, Chen-Wang Chang, Te-Hsin Chao, Jen-Wei Chou, Yenn-Hwei Chou, Chiao-Hsiung Chuang, Wen-Hung Hsu, Tzu-Chi Hsu, Tien-Yu Huang, Tsung-I Hung, Puo-Hsien Le, Chun-Che Lin, Chun-Chi Lin, Ching-Pin Lin, Jen-Kou Lin, Wei-Chen Lin, Yen-Hsuan Ni, Ming-Jium Shieh, I-Lun Shih, Chia-Tung Shun, Tzung-Jiun Tsai, Cheng-Yi Wang, Meng-Tzu Weng, Jau-Min Wong, Deng-Chyang Wu, Shu-Chen Wei
Intest Res. 2024;22(3):250-285. doi: 10.5217/ir.2024.00060.
Reference
-
1. Ng SC, Bernstein CN, Vatn MH, et al. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013; 62:630–649.
Article2. Chi KR. Epidemiology: rising in the east. Nature. 2016; 540:S100–S102.
Article3. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018; 390:2769–2778.
Article4. Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015; 12:720–727.
Article5. Wei SC, Lin MH, Tung CC, et al. A nationwide populationbased study of the inflammatory bowel diseases between 1998 and 2008 in Taiwan. BMC Gastroenterol. 2013; 13:166.
Article6. Ishige T, Tomomasa T, Hatori R, et al. Temporal trend of pediatric inflammatory bowel disease: analysis of national registry data 2004-2013 in Japan. J Pediatr Gastroenterol Nutr. 2017; 65:e80. –e82.7. Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016; 14:111–119.
Article8. Yang H, Li Y, Wu W, et al. The incidence of inflammatory bowel disease in Northern China: a prospective population-based study. PLoS One. 2014; 9:e101296.
Article9. Hammer T, Nielsen KR, Munkholm P, Burisch J, Lynge E. The Faroese IBD study: incidence of inflammatory bowel diseases across 54 years of population-based data. J Crohns Colitis. 2016; 10:934–942.
Article10. Fonager K, Sørensen HT, Olsen J. Change in incidence of Crohn’s disease and ulcerative colitis in Denmark: a study based on the national registry of patients, 1981-1992. Int J Epidemiol. 1997; 26:1003–1008.
Article11. Yoshida Y, Murata Y. Inflammatory bowel disease in Japan: studies of epidemiology and etiopathogenesis. Med Clin North Am. 1990; 74:67–90.
Article12. Ng SC, Leung WK, Shi HY, et al. Epidemiology of inflammatory bowel disease from 1981 to 2014: results from a territorywide population-based registry in Hong Kong. Inflamm Bowel Dis. 2016; 22:1954–1960.13. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549.
Article14. Hilmi I, Jaya F, Chua A, Heng WC, Singh H, Goh KL. A first study on the incidence and prevalence of IBD in Malaysia: results from the Kinta Valley IBD Epidemiology Study. J Crohns Colitis. 2015; 9:404–409.
Article15. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280.
Article16. Ng SC, Tsoi KK, Kamm MA, et al. Genetics of inflammatory bowel disease in Asia: systematic review and meta-analysis. Inflamm Bowel Dis. 2012; 18:1164–1176.
Article17. Bernstein CN, Shanahan F. Disorders of a modern lifestyle: reconciling the epidemiology of inflammatory bowel diseases. Gut. 2008; 57:1185–1191.
Article18. Wei SC, Shieh MJ, Chang MC, Chang YT, Wang CY, Wong JM. Long-term follow-up of ulcerative colitis in Taiwan. J Chin Med Assoc. 2012; 75:151–155.
Article19. Kim HJ, Hann HJ, Hong SN, et al. Incidence and natural course of inflammatory bowel disease in Korea, 2006-2012: a nationwide population-based study. Inflamm Bowel Dis. 2015; 21:623–630.
Article20. Wei SC, Chang TA, Chao TH, et al. Management of ulcerative colitis in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease. Intest Res. 2017; 15:266–284.
Article21. Wei SC, Chang TA, Chao TH, et al. Management of Crohn’s disease in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease. Intest Res. 2017; 15:285–310.
Article22. Leddin D, Tamim H, Levy AR. Decreasing incidence of inflammatory bowel disease in eastern Canada: a population database study. BMC Gastroenterol. 2014; 14:140.
Article23. Lophaven SN, Lynge E, Burisch J. The incidence of inflammatory bowel disease in Denmark 1980-2013: a nationwide cohort study. Aliment Pharmacol Ther. 2017; 45:961–972.
Article24. Bitton A, Vutcovici M, Patenaude V, Sewitch M, Suissa S, Brassard P. Epidemiology of inflammatory bowel disease in Québec: recent trends. Inflamm Bowel Dis. 2014; 20:1770–1776.25. Yen HH, Chang CW, Chou JW, Wei SC. Balloon-assisted enteroscopy and capsule endoscopy in suspected small bowel Crohn’s disease. Clin Endosc. 2017; 50:417–423.
Article26. Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017; 152:313–321.
Article27. Chiang TH, Lee YC, Liao WC, et al. Timing and risk factors for a positive fecal immunochemical test in subsequent screening for colorectal neoplasms. PLoS One. 2015; 10:e0136890.
Article28. van der Valk ME, Mangen MJ, Leenders M, et al. Healthcare costs of inflammatory bowel disease have shifted from hospitalisation and surgery towards anti-TNFalpha therapy: results from the COIN study. Gut. 2014; 63:72–79.
Article29. Wei SC. Differences in the public medical insurance systems for inflammatory bowel disease treatment in Asian countries. Intest Res. 2016; 14:218–223.
Article30. Chang CW, Wei SC, Chou JW, et al. Safety and efficacy of adalimumab for patients with moderate to severe Crohn’s disease: the Taiwan Society of Inflammatory Bowel Disease (TSIBD) Study. Intest Res. 2014; 12:287–292.
Article31. Lin WC, Chou JW, Yen HH, et al. Outcomes of limited period of adalimumab treatment in moderate to severe Crohn’s disease patients: Taiwan Society of Inflammatory Bowel Disease Study. Intest Res. 2017; 15:487–494.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Seminar Report From the 2014 Taiwan Society of Inflammatory Bowel Disease (TSIBD) Spring Forum (May 24th, 2014): Crohn's Disease Versus Intestinal Tuberculosis Infection
- Should Asian inflammatory bowel disease patients need routine thromboprophylaxis?
- Could fecal calprotectin enter mainstream use for diagnosing and monitoring inflammatory bowel disease?
- Chemoprevention of Colitis-Associated Dysplasia or Cancer in Inflammatory Bowel Disease
- Inflammatory Bowel Disease and the Risk of Herpes Zoster