Korean J Radiol.
2019 Mar;20(3):429-437. 10.3348/kjr.2018.0260.
MRI T2-Weighted Imaging and Fat-Suppressed T2-Weighted Imaging Image Fusion Technology Improves Image Discriminability for the Evaluation of Anal Fistulas
- Affiliations
-
- 1Department of Radiology, The First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China. liziping163@163.com
- 2Faculty of Medicine and Dentistry, University of Western Australia, Perth, Australia.
- 3Department of Gastrointestinal Surgery, The First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China.
- KMID: 2438273
- DOI: http://doi.org/10.3348/kjr.2018.0260
Abstract
OBJECTIVE
To explore whether MRI fusion technology (combined T2-weighted imaging [T2WI] and fat-suppressed T2WI [T2WI-(FS)]) improves signal differences between anal fistulas and surrounding structures.
MATERIALS AND METHODS
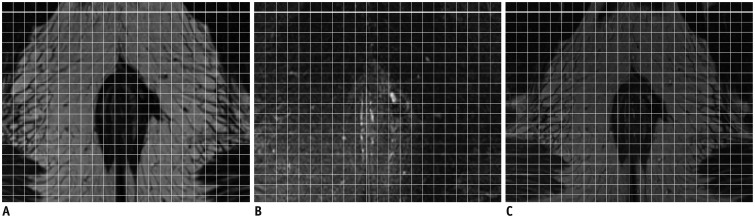
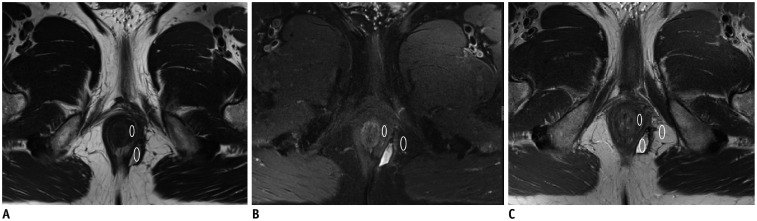
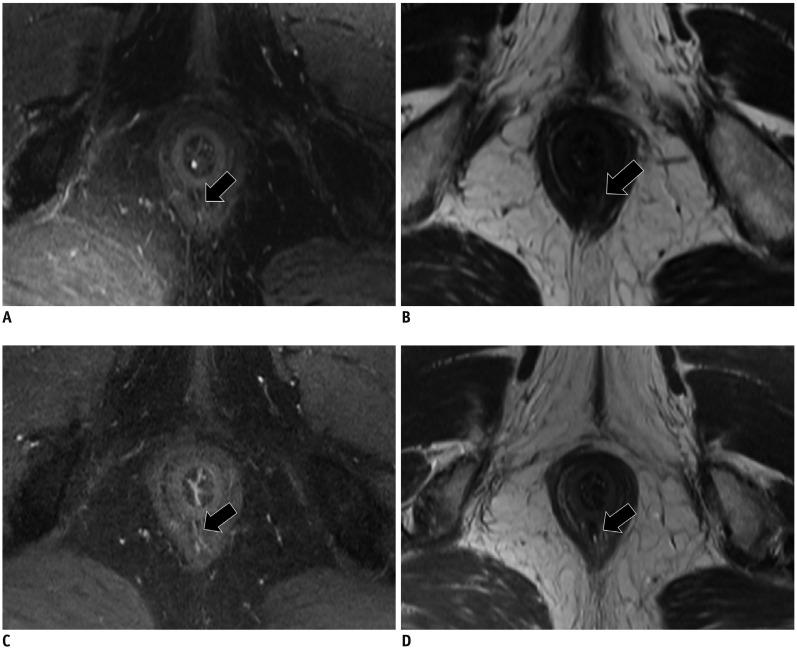
A total of 32 patients with confirmed diagnoses of anal fistula were retrospectively studied. All available T2WI and T2WI-(FS) images for each patient were used to generate fusion image (T2WI-(Fusion)) based on the addition of gray values obtained from each pixel via an MR post-processing work station. The discriminability of fistula, perianal sphincter, and perianal fat in T2WI, T2WI-(FS), and T2WI-(Fusion) images was quantified with Fisher's scoring algorithm. For subjective visual image assessment by researchers, five-point scale scores were determined using a modified double-stimulus continuous quality-scale test to evaluate T2WI-(FS), T2WI, enhanced axial three-dimensional-volumetric interpolated breath-hold examination (3D-VIBE), and T2WI-(Fusion) sequence images. The differences were subsequently compared.
RESULTS
Mean Fisher scores for fistulas vs. sphincters obtained from T2WI-(Fusion) (F(Fusion-fistula) = 6.56) were significantly higher than those from T2WI (F(T2WI-fistula) = 3.35) (p = 0.001). Mean Fisher scores for sphincters vs. fat from T2WI-(Fusion) (F(Fusion-sphincter) = 10.84) were significantly higher than those from T2WI-(FS) (FS(FS-sphincter) = 2.57) (p = 0.001). In human assessment, T2WI-(Fusion) showed the same fistula discriminability as T2WI-(FS), and better sphincter discriminability than T2WI. Overall, T2WI-(Fusion) showed better discriminability than T2WI, T2WI-(FS), and enhanced 3D-VIBE images.
CONCLUSION
T2WI and T2WI-(FS) fusion technology improves signal differences between anal fistulas and surrounding structures, and may facilitate better evaluation of anal fistulas and sphincters.
MeSH Terms
Figure
Reference
-
1. Liang C, Lu Y, Zhao B, Du Y, Wang C, Jiang W. Imaging of anal fistulas: comparison of computed tomographic fistulography and magnetic resonance imaging. Korean J Radiol. 2014; 15:712–723. PMID: 25469082.
Article2. Baskan O, Koplay M, Sivri M, Erol C. Our experience with MR imaging of perianal fistulas. Pol J Radiol. 2014; 79:490–497. PMID: 25550766.
Article3. de Miguel Criado J, del Salto LG, Rivas PF, del Hoyo LF, Velasco LG, de las Vacas MI, et al. MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics. 2012; 32:175–194. PMID: 22236900.
Article4. Lo Re G, Tudisca C, Vernuccio F, Picone D, Cappello M, Agnello F, et al. MR imaging of perianal fistulas in Crohn's disease: sensitivity and specificity of STIR sequences. Radiol Med. 2016; 121:243–251. PMID: 26643166.
Article5. Inoue HK, Nakajima A, Sato H, Noda SE, Saitoh J, Suzuki Y. Image fusion for radiosurgery, neurosurgery and hypofractionated radiotherapy. Cureus. 2015; 7:e252. PMID: 26180676.
Article6. Misaki M, Savitz J, Zotev V, Phillips R, Yuan H, Young KD, et al. Contrast enhancement by combining T1- and T2-weighted structural brain MR Images. Magn Reson Med. 2015; 74:1609–1620. PMID: 25533337.
Article7. Huo D, Salem KA, Jiang Y, Wilson DL. Optimization of spiral MRI using a perceptual difference model. Int J Biomed Imaging. 2006; 2006:35290. PMID: 23165025.
Article8. ITU Radiocommunication Assembly. Recommendation ITU-R BT.500-11. Methodology for the subjective assessment of the quality of television pictures. International Telecommunication Union;updated 2002. Accessed June, 2002. Available at: https://www.itu.int/dms_pubrec/itu-r/rec/bt/R-REC-BT.500-11-200206-S!!PDF-E.pdf.9. Singh K, Singh N, Thukral C, Singh KP, Bhalla V. Magnetic resonance imaging (MRI) evaluation of perianal fistulae with surgical correlation. J Clin Diagn Res. 2014; 8:RC01–RC04.
Article10. Ziech ML, Lavini C, Bipat S, Ponsioen CY, Spijkerboer AM, Stokkers PC, et al. Dynamic contrast-enhanced MRI in determining disease activity in perianal fistulizing Crohn disease: a pilot study. AJR Am J Roentgenol. 2013; 200:W170–W177. PMID: 23345381.
Article11. Hu D, Wang C, Langer M. [Comparison of MR-sequence in the diagnosis of anal fistula--the clinical value of 3D flash]. J Huazhong Univ Sci Technolog Med Sci. 2002; 22:241–245. PMID: 12658816.12. Yoshizako T, Kitagaki H. A pictorial review of the impact of adding diffusion-weighted MR imaging to other MR sequences for assessment of anal fistulae. Jpn J Radiol. 2013; 31:371–376. PMID: 23588593.
Article13. Yoshizako T, Wada A, Takahara T, Kwee TC, Nakamura M, Uchida K, et al. Diffusion-weighted MRI for evaluating perianal fistula activity: feasibility study. Eur J Radiol. 2012; 81:2049–2053. PMID: 21767926.
Article14. Cavusoglu M, Duran S, Sözmen Cılız D, Tufan G, Hatipoglu Çetin HG, Ozsoy A, et al. Added value of diffusion-weighted magnetic resonance imaging for the diagnosis of perianal fistula. Diagn Interv Imaging. 2017; 98:401–408. PMID: 27964847.
Article15. Szyszko TA, Bush J, Gishen P, Sellu D, Desouza NM. Endoanal magnetic resonance imaging of fistula-in-ano: a comparison of STIR with gadolinium-enhanced techniques. Acta Radiol. 2005; 46:3–8. PMID: 15841733.
Article16. Xiaoming L, Rongrong G, Shengpan J. The study on the diagnostic value with LAVA-FLEX sequence for diagnosing anal fistula. Chinese Journal of CT and MRI. 2015; (6):80–83.17. Antonica F, Asabella AN, Ferrari C, Rubini D, Notaristefano A, Nicoletti A, et al. Useful diagnostic biometabolic data obtained by PET/CT and MR fusion imaging using open source software. Hell J Nucl Med. 2014; 17(Suppl 1):50–55. PMID: 24392469.18. Loeffelbein DJ, Souvatzoglou M, Wankerl V, Dinges J, Ritschl LM, Mücke T, et al. Diagnostic value of retrospective PET-MRI fusion in head-and-neck cancer. BMC Cancer. 2014; 14:846. PMID: 25407100.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Abbreviated Breast Magnetic Resonance Imaging: Background, Evidence From Studies, and Future Considerations
- Improvement of Fat Suppression and Artifact Reduction Using IDEAL Technique in Head and Neck MRI at 3T
- MR imaging of oral cavity malignancy
- MRI Findings of Intracranial IVleningioma: Significance of Gd-DTPA Enhancernent
- Significance of Increased Signal Intensity on T2 Weighted MRI in Patients with Cervical Spondylosis