Cancer Res Treat.
2019 Jan;51(1):280-288. 10.4143/crt.2018.079.
Different Patterns of Risk Reducing Decisions in Affected or Unaffected BRCA Pathogenic Variant Carriers
- Affiliations
-
- 1Center for Breast Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea. eslee@ncc.re.kr
- 2Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea. ksy@ncc.re.kr
- 3Center for Uterine Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 4Cancer Healthcare Research Branch, Research Institute, National Cancer Center, Goyang, Korea.
- 5Common Cancer Branch, Research Institute, National Cancer Center, Goyang, Korea.
- 6Biometrics Research Branch, Division of Cancer Epidemiology and Management, Research Institute, National Cancer Center, Goyang, Korea.
- 7Department of Laboratory Medicine & Genetic Counselling Clinics, Hospital, National Cancer Center, Goyang, Korea.
- KMID: 2437619
- DOI: http://doi.org/10.4143/crt.2018.079
Abstract
- PURPOSE
The purpose of this study was to investigate decision patterns to reduce the risks of BRCArelated breast and gynecologic cancers in carriers of BRCA pathogenic variants. We found a change in risk-reducing (RR) management patterns after December 2012, when the National Health Insurance System (NHIS) of Korea began to pay for BRCA testing and riskreducing salpingo-oophorectomy (RRSO) in pathogenic-variant carriers.
MATERIALS AND METHODS
The study group consisted of 992 patients, including 705 with breast cancer (BC), 23 with ovarian cancer (OC), 10 with both, and 254 relatives of high-risk patients who underwent BRCA testing at the National Cancer Center of Korea from January 2008 to December 2016.We analyzed patterns of and factors in RR management.
RESULTS
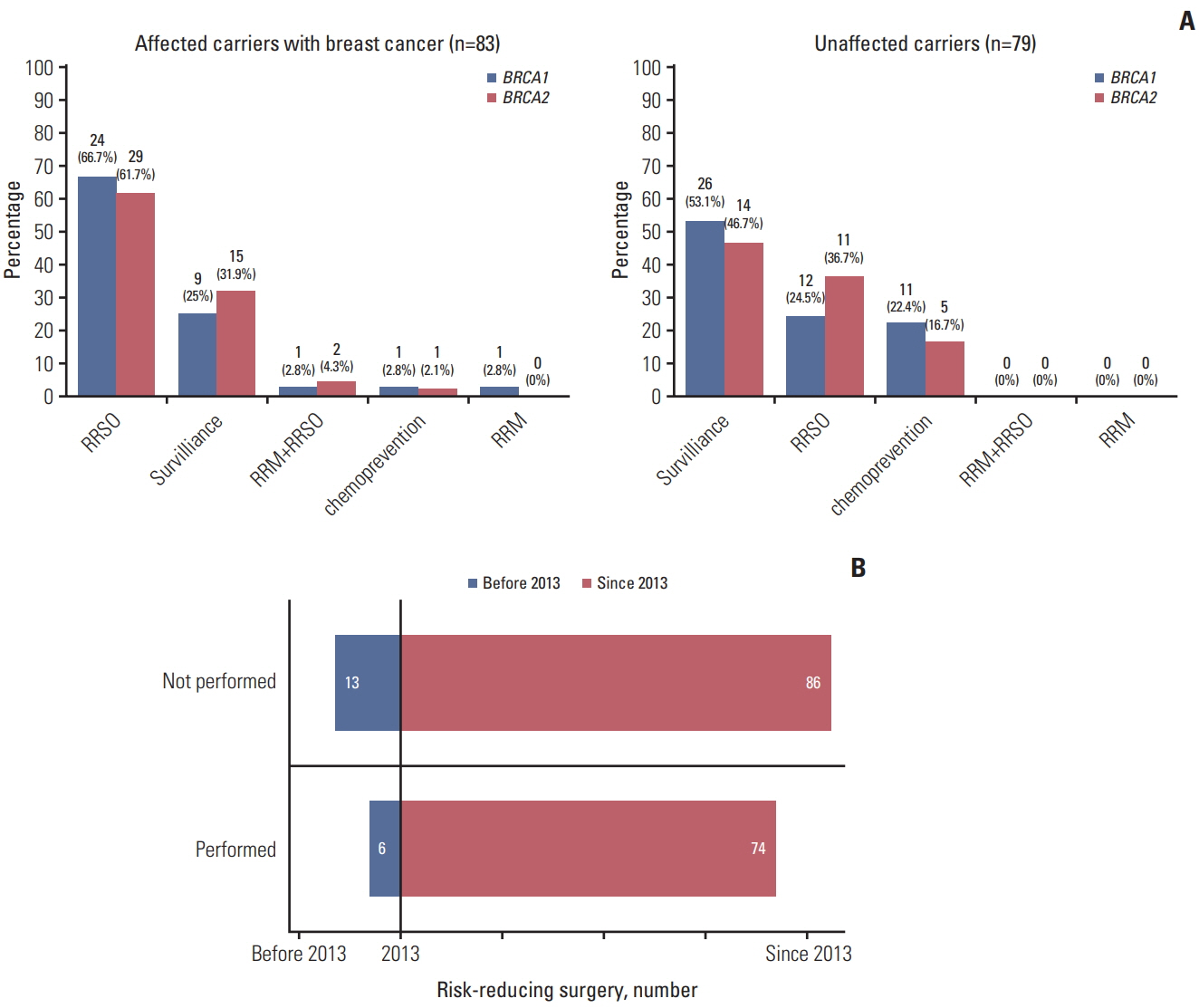
Of the 992 patients, 220 (22.2%) were carriers of BRCA pathogenic variants. About 92.3% (203/220) had a family history of BC and/or OC,which significantly differed between BRCA1 and BRCA2 carriers (p < 0.001). All 41 male carriers chose surveillance. Of the 179 female carriers, 59 of the 83 carriers (71.1%) with BC and the 39 of 79 unaffected carriers (49.4%) underwent RR management. None of the carriers affected with OC underwent RR management. Of the management types, RRSO had the highest rate (42.5%) of patient choice. The rate of RR surgery was significantly higher after 2013 than before 2013 (46.3% [74/160] vs. 31.6% [6/19], p < 0.001).
CONCLUSION
RRSO was the preferred management for carriers of BRCA pathogenic variants. The most important factors in treatment choice were NHIS reimbursement and/or the severity of illness.
MeSH Terms
Figure
Cited by 2 articles
-
Disparities between Uptake of Germline
BRCA1/2 Gene Tests and Implementation of Post-test Management Strategies in Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer Patients
Young Min Hur, Jaehee Mun, Mi-Kyung Kim, Maria Lee, Yun Hwan Kim, Seung-Cheol Kim
J Korean Med Sci. 2021;36(38):e241. doi: 10.3346/jkms.2021.36.e241.Implementation of BRCA Test among Young Breast Cancer Patients in South Korea: A Nationwide Cohort Study
Yung-Huyn Hwang, Tae-Kyung Yoo, Sae Byul Lee, Jisun Kim, Beom Seok Ko, Hee Jeong Kim, Jong Won Lee, Byung Ho Son, Il Yong Chung
Cancer Res Treat. 2024;56(3):802-808. doi: 10.4143/crt.2023.1186.
Reference
-
References
1. Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996; 77:2318–24.
Article2. Easton DF. How many more breast cancer predisposition genes are there? Breast Cancer Res. 1999; 1:14–7.
Article3. Beattie MS, Crawford B, Lin F, Vittinghoff E, Ziegler J. Uptake, time course, and predictors of risk-reducing surgeries in BRCA carriers. Genet Test Mol Biomarkers. 2009; 13:51–6.4. Campeau PM, Foulkes WD, Tischkowitz MD. Hereditary breast cancer: new genetic developments, new therapeutic avenues. Hum Genet. 2008; 124:31–42.
Article5. Pal T, Permuth-Wey J, Betts JA, Krischer JP, Fiorica J, Arango H, et al. BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer. 2005; 104:2807–16.6. Friedenson B. BRCA1 and BRCA2 pathways and the risk of cancers other than breast or ovarian. MedGenMed. 2005; 7:60.7. Meijers-Heijboer H, van Geel B, van Putten WL, Henzen-Logmans SC, Seynaeve C, Menke-Pluymers MB, et al. Breast cancer after prophylactic bilateral mastectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2001; 345:159–64.8. Greene MH, Mai PL, Schwartz PE. Does bilateral salpingectomy with ovarian retention warrant consideration as a temporary bridge to risk-reducing bilateral oophorectomy in BRCA1/2 mutation carriers? Am J Obstet Gynecol. 2011; 204:19.9. Morris JL, Gordon OK. Positive results: making the best decisions when you're at high risk for breast or ovarian cancer. Amherst, NY: Prometheus Books;2010.10. Daly MB, Pilarski R, Axilbund JE, Berry M, Buys SS, Crawford B, et al. Genetic/familial high-risk assessment: breast and ovarian, version 2.2015. J Natl Compr Canc Netw. 2016; 14:153–62.
Article11. Schwartz MD, Isaacs C, Graves KD, Poggi E, Peshkin BN, Gell C, et al. Long-term outcomes of BRCA1/BRCA2 testing: risk reduction and surveillance. Cancer. 2012; 118:510–7.12. Kim SI, Lim MC, Lee DO, Kong SY, Seo SS, Kang S, et al. Uptake of risk-reducing salpingo-oophorectomy among female BRCA mutation carriers: experience at the National Cancer Center of Korea. J Cancer Res Clin Oncol. 2016; 142:333–40.13. Fu R, Harris EL, Helfand M, Nelson HD. Estimating risk of breast cancer in carriers of BRCA1 and BRCA2 mutations: a meta-analytic approach. Stat Med. 2007; 26:1775–87.14. Garcia C, Wendt J, Lyon L, Jones J, Littell RD, Armstrong MA, et al. Risk management options elected by women after testing positive for a BRCA mutation. Gynecol Oncol. 2014; 132:428–33.15. Choi MC, Lim MC, Lee M, Kim MK, Suh DH, Song YJ, et al. Practice patterns of hereditary ovarian cancer management in Korea. Int J Gynecol Cancer. 2017; 27:895–9.
Article16. Lim MC, Moon EK, Shin A, Jung KW, Won YJ, Seo SS, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea, 1999-2010. J Gynecol Oncol. 2013; 24:298–302.
Article17. Watson M, Foster C, Eeles R, Eccles D, Ashley S, Davidson R, et al. Psychosocial impact of breast/ovarian (BRCA1/2) cancer-predictive genetic testing in a UK multi-centre clinical cohort. Br J Cancer. 2004; 91:1787–94.18. Del Corral GA, Wes AM, Fischer JP, Serletti JM, Wu LC. Outcomes and cost analysis in high-risk patients undergoing simultaneous free flap breast reconstruction and gynecologic procedures. Ann Plast Surg. 2015; 75:534–8.
Article19. Hagen AI, Maehle L, Veda N, Vetti HH, Stormorken A, Ludvigsen T, et al. Risk reducing mastectomy, breast reconstruction and patient satisfaction in Norwegian BRCA1/2 mutation carriers. Breast. 2014; 23:38–43.20. Hooker GW, King L, Vanhusen L, Graves K, Peshkin BN, Isaacs C, et al. Long-term satisfaction and quality of life following risk reducing surgery in BRCA1/2 mutation carriers. Hered Cancer Clin Pract. 2014; 12:9.
Article21. Gamble C, Havrilesky LJ, Myers ER, Chino JP, Hollenbeck S, Plichta JK, et al. Cost effectiveness of risk-reducing mastectomy versus surveillance in BRCA mutation carriers with a history of ovarian cancer. Ann Surg Oncol. 2017; 24:3116–23.22. Evans DG, Barwell J, Eccles DM, Collins A, Izatt L, Jacobs C, et al. The Angelina Jolie effect: how high celebrity profile can have a major impact on provision of cancer related services. Breast Cancer Res. 2014; 16:442.
Article23. Freedman R, Mountain H, Karina D, Schofield L. A retrospective exploration of the impact of the 'Angelina Jolie Effect' on the single state-wide familial cancer program in Perth, Western Australia. J Genet Couns. 2017; 26:52–62.
Article24. Evans DG, Wisely J, Clancy T, Lalloo F, Wilson M, Johnson R, et al. Longer term effects of the Angelina Jolie effect: increased risk-reducing mastectomy rates in BRCA carriers and other high-risk women. Breast Cancer Res. 2015; 17:143.
Article25. Lim MC, Kim TJ, Kang S, Bae DS, Park SY, Seo SS. Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for adnexal tumors. Surg Endosc. 2009; 23:2445–9.
Article26. Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of risk reduction estimates associated with risk-reducing salpingooophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst. 2009; 101:80–7.27. Bando H. Issues of concern in risk assessment, genetic counseling, and genetic testing of younger breast cancer patients in Japan. Breast Cancer. 2014; 21:656–63.
Article28. Eitan R, Michaelson-Cohen R, Levavi H, Beller U. The counseling and management of young healthy BRCA mutation carriers. Int J Gynecol Cancer. 2009; 19:1156–9.29. Kauff ND, Scheuer L, Robson ME, Glogowski E, Kelly B, Barakat R, et al. Insurance reimbursement for risk-reducing mastectomy and oophorectomy in women with BRCA1 or BRCA2 mutations. Genet Med. 2001; 3:422–5.30. Guillem JG, Wood WC, Moley JF, Berchuck A, Karlan BY, Mutch DG, et al. ASCO/SSO review of current role of riskreducing surgery in common hereditary cancer syndromes. Ann Surg Oncol. 2006; 13:1296–321.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usage Patterns of Surveillance, Chemoprevention and Risk-Reducing Surgery in Korean BRCA Mutation Carriers: 5 Years of Experience at a Single Institution
- BRCA1/BRCA2 Pathogenic Variant Breast Cancer: Treatment and Prevention Strategies
- The Incidence of Occult Malignancy in Contralateral Risk Reducing Mastectomy Among Affected Breast Cancer Gene Mutation Carriers in South Korea
- Experience with Bilateral Risk-Reducing Mastectomy for an Unaffected BRCA Mutation Carrier
- Differences in age at diagnosis of ovarian cancer for each BRCA mutation type in Japan: optimal timing to carry out risk-reducing salpingo-oophorectomy