Clin Exp Otorhinolaryngol.
2019 Feb;12(1):40-49. 10.21053/ceo.2018.00185.
In Vivo Vibration Measurement of Middle Ear Structure Using Doppler Optical Coherence Tomography: Preliminary Study
- Affiliations
-
- 1School of Electronics Engineering, College of IT Engineering, Kyungpook National University, Daegu, Korea.
- 2Department of Otology and Laryngology, Harvard Medical School, Boston, MA, USA.
- 3Eaton-Peabody Laboratories, Massachusetts Eye and Ear Infirmary (MEEI), Boston, MA, USA.
- 4Department of Otolaryngology, Ajou University School of Medicine, Suwon, Korea. jhj@ajou.ac.kr
- KMID: 2437490
- DOI: http://doi.org/10.21053/ceo.2018.00185
Abstract
OBJECTIVES
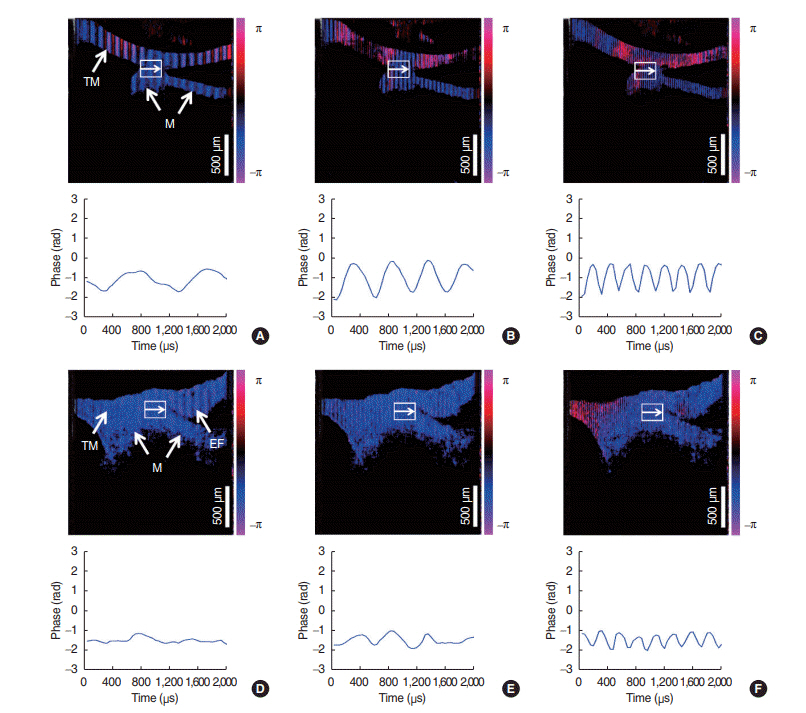
Doppler optical coherence tomography (DOCT) is useful for both, the spatially resolved measurement of the tympanic membrane (TM) oscillation and high-resolution imaging. We demonstrated a new technique capable of providing real-time two-dimensional Doppler OCT image of rapidly oscillatory latex mini-drum and in vivo rat TM and ossicles.
METHODS
Using DOCT system, the oscillation of sample was measured at frequency range of 1-4 kHz at an output of 15 W. After the sensitivity of the DOCT system was verified using a latex mini-drum consisting of a 100 μm-thick latex membrane, changes in displacement of the umbo and contacted area between TM and malleus in normal and pathologic conditions.
RESULTS
The oscillation cycles of the mini-drum for stimulus frequencies were 1.006 kHz for 1 kHz, 2.012 kHz for 2kHz, and 3.912 kHz for 4 kHz, which means that the oscillation cycle of the mini-drum become short in proportional to the frequency of stimuli. The oscillation cycles of umbo area and the junction area in normal TM for frequencies of the stimuli showed similar integer ratio with the data of latex mini-drum for stimuli less than 4 kHz. In the case of middle ear effusion condition, the Doppler signal showed a tendency of attenuation in all frequencies, which was prominent at 1 kHz and 2 kHz.
CONCLUSION
The TM vibration under sound stimulation with frequencies from 1 kHz to 4 kHz in normal and pathologic conditions was demonstrated using signal demodulation method in in vivo condition. The OCT technology could be helpful for functional and structural assessment as an optional modality.
MeSH Terms
Figure
Reference
-
1. Nuttall AL, Dolan DF, Avinash G. Laser Doppler velocimetry of basilar membrane vibration. Hear Res. 1991; Feb. 51(2):203–13.
Article2. Chang EW, Cheng JT, Roosli C, Kobler JB, Rosowski JJ, Yun SH. Simultaneous 3D imaging of sound-induced motions of the tympanic membrane and middle ear ossicles. Hear Res. 2013; Oct. 304:49–56.
Article3. Lee HY, Raphael PD, Park J, Ellerbee AK, Applegate BE, Oghalai JS. Noninvasive in vivo imaging reveals differences between tectorial membrane and basilar membrane traveling waves in the mouse cochlea. Proc Natl Acad Sci U S A. 2015; Mar. 112(10):3128–33.
Article4. MacDougall D, Farrell J, Brown J, Bance M, Adamson R. Long-range, wide-field swept-source optical coherence tomography with GPU accelerated digital lock-in Doppler vibrography for real-time, in vivo middle ear diagnostics. Biomed Opt Express. 2016; Oct. 7(11):4621–35.
Article5. Hong SS, Freeman DM. Doppler optical coherence microscopy for studies of cochlear mechanics. J Biomed Opt. 2006; Sep-Oct. 11(5):054014.
Article6. Seidman MD, Standring RT, Ahsan S, Marzo S, Shohet J, Lumley C, et al. Normative data of incus and stapes displacement during middle ear surgery using laser Doppler vibrometry. Otol Neurotol. 2013; Dec. 34(9):1719–24.
Article7. Aarnisalo AA, Cheng JT, Ravicz ME, Hulli N, Harrington EJ, Hernandez-Montes MS, et al. Middle ear mechanics of cartilage tympanoplasty evaluated by laser holography and vibrometry. Otol Neurotol. 2009; Dec. 30(8):1209–14.
Article8. Ball GR, Huber A, Goode RL. Scanning laser Doppler vibrometry of the middle ear ossicles. Ear Nose Throat J. 1997; Apr. 76(4):213–8.
Article9. Dong W, Varavva P, Olson ES. Sound transmission along the ossicular chain in common wild-type laboratory mice. Hear Res. 2013; Jul. 301:27–34.
Article10. Kunimoto Y, Hasegawa K, Arii S, Kataoka H, Yazama H, Kuya J, et al. Sequential multipoint motion of the tympanic membrane measured by laser Doppler vibrometry: preliminary results for normal tympanic membrane. Otol Neurotol. 2014; Apr. 35(4):719–24.11. Subhash HM, Nguyen-Huynh A, Wang RK, Jacques SL, Choudhury N, Nuttall AL. Feasibility of spectral-domain phase-sensitive optical coherence tomography for middle ear vibrometry. J Biomed Opt. 2012; Jun. 17(6):060505.
Article12. Burkhardt A, Kirsten L, Bornitz M, Zahnert T, Koch E. Investigation of the human tympanic membrane oscillation ex vivo by Doppler optical coherence tomography. J Biophotonics. 2014; Jun. 7(6):434–41.13. Zhang K, Kang JU. Real-time 4D signal processing and visualization using graphics processing unit on a regular nonlinear-k Fourier-domain OCT system. Opt Express. 2010; May. 18(11):11772–84.
Article14. Jeong H, Cho NH, Jung U, Lee C, Kim JY, Kim J. Ultra-fast displaying Spectral Domain Optical Doppler Tomography system using a Graphics Processing Unit. Sensors (Basel). 2012; 12(6):6920–9.
Article15. American National Standards Institute. American national standard for safe use of lasers: standard Z1361-2007. Orlando (FL): Laser Institute of America;2007.16. Cho NH, Jung U, Kim S, Jung W, Oh J, Kang HW, et al. High speed SD-OCT system using GPU accelerated mode for in vivo human eye imaging. J Opt Soc Korea. 2013; Feb. 17(1):68–72.
Article17. Cho NH, Park K, Wijesinghe RE, Shin YS, Jung W, Kim J. Development of real-time dual-display handheld and bench-top hybrid-mode SD-OCTs. Sensors (Basel). 2014; Jan. 14(2):2171–81.18. Yang V, Gordon M, Qi B, Pekar J, Lo S, Seng-Yue E, et al. High speed, wide velocity dynamic range Doppler optical coherence tomography (Part I): system design, signal processing, and performance. Opt Express. 2003; Apr. 11(7):794–809.
Article19. Makita S, Fabritius T, Yasuno Y. Quantitative retinal-blood flow measurement with three-dimensional vessel geometry determination using ultrahigh-resolution Doppler optical coherence angiography. Opt Lett. 2008; Apr. 33(8):836–8.
Article20. Ahn YC, Jung W, Chen Z. Quantification of a three-dimensional velocity vector using spectral-domain Doppler optical coherence tomography. Opt Lett. 2007; Jun. 32(11):1587–9.
Article21. Ravicz ME, Rosowski JJ, Merchant SN. Mechanisms of hearing loss resulting from middle-ear fluid. Hear Res. 2004; Sep. 195(1-2):103–30.
Article22. Gan RZ, Dai C, Wood MW. Laser interferometry measurements of middle ear fluid and pressure effects on sound transmission. J Acoust Soc Am. 2006; Dec. 120(6):3799–810.
Article23. Nakajima HH, Pisano DV, Roosli C, Hamade MA, Merchant GR, Mahfoud L, et al. Comparison of ear-canal reflectance and umbo velocity in patients with conductive hearing loss: a preliminary study. Ear Hear. 2012; Jan-Feb. 33(1):35–43.
Article24. Rosowski JJ, Nakajima HH, Merchant SN. Clinical utility of laser-Doppler vibrometer measurements in live normal and pathologic human ears. Ear Hear. 2008; Jan. 29(1):3–19.
Article25. Arechvo I, Lasurashvili N, Bornitz M, Kevanishvili Z, Zahnert T. Laser Doppler vibrometry of the middle ear in humans: derivation dependence, variability, and bilateral differences. Medicina (Kaunas). 2009; 45(11):878–86.
Article26. Goode RL. Middle ear transmission disorders by laser-Doppler vibrometry. Acta Otolaryngol. 1994; Nov. 114(6):679–81.27. Stasche N, Foth HJ, Hormann K, Baker A, Huthoff C. Middle ear transmission disorders: tympanic membrane vibration analysis by laser-Doppler-vibrometry. Acta Otolaryngol. 1994; Jan. 114(1):59–63.28. Niehorster DC, Cheng JC, Li L. Optimal combination of form and motion cues in human heading perception. J Vis. 2010; Sep. 10(11):20.29. Cheng JT, Hamade M, Merchant SN, Rosowski JJ, Harrington E, Furlong C. Wave motion on the surface of the human tympanic membrane: holographic measurement and modeling analysis. J Acoust Soc Am. 2013; Feb. 133(2):918–37.
Article30. Guan X, Li W, Gan RZ. Comparison of eardrum mobility in acute otitis media and otitis media with effusion models. Otol Neurotol. 2013; Sep. 34(7):1316–20.
Article31. Zhang X, Guan X, Nakmali D, Palan V, Pineda M, Gan RZ. Experimental and modeling study of human tympanic membrane motion in the presence of middle ear liquid. J Assoc Res Otolaryngol. 2014; Dec. 15(6):867–81.
Article32. Dai C, Gan RZ. Change of middle ear transfer function in otitis media with effusion model of guinea pigs. Hear Res. 2008; Sep. 243(1-2):78–86.
Article33. Carr JA, Valdez TA, Bruns OT, Bawendi MG. Using the shortwave infrared to image middle ear pathologies. Proc Natl Acad Sci U S A. 2016; Sep. 113(36):9989–94.
Article34. Monroy GL, Pande P, Shelton RL, Nolan RM, Spillman DR Jr, Porter RG, et al. Non-invasive optical assessment of viscosity of middle ear effusions in otitis media. J Biophotonics. 2017; Mar. 10(3):394–403.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extratympanic Observation of Middle and Inner Ear Structures in Rodents Using Optical Coherence Tomography
- Availability of Optical Coherence Tomography in Diagnosis and Classification of Choroidal Neovascularization
- In-vivo Optical Measurement of Neural Activity in the Brain
- Optical Imaging and Its Clinical Application in Otorhinolaryngology
- Early caries detection using optical coherence tomography: a review of the literature