Anesth Pain Med.
2018 Jul;13(3):329-335. 10.17085/apm.2018.13.3.329.
Endotracheal intubation using semi-rigid optical stylet in simulated difficult airways of high grade modified Cormack and Lehane laryngeal views
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 2Department of Anesthesiology and Pain Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Anesthesiology and Pain Medicine, Kwangju Christian Hospital, Gwangju, Korea. d013084@naver.com
- KMID: 2436044
- DOI: http://doi.org/10.17085/apm.2018.13.3.329
Abstract
- BACKGROUND
Endotracheal intubation in patients with compromised cervical vertebrae and limited mouth opening is challenging, however, there are still limited options available. Among devices used for managing difficult airways, the Clarus Video System (CVS) might have considerable promise due to its semi-rigid tip. We evaluated the performance of CVS in patients with simulated difficult airways.
METHODS
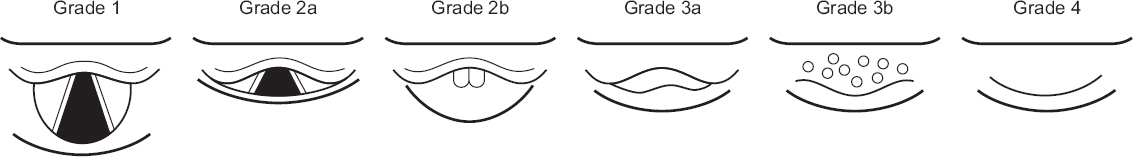
Philadelphia cervical collars were applied to 74 patients undergoing general anesthesia. The degree of simulated difficult airway was assessed by observing laryngeal view using McCoy laryngoscope; modified Cormack and Lehane grade (MCL) ≥ 3a (high-grade group, n = 38) or ≤ 2b (low-grade group, n = 36). Subsequently, patients were intubated using CVS by a blinded practitioner. We evaluated total time to intubation, intubation success rate, and conditions of intubation.
RESULTS
Intubation took significantly longer time for the high-grade group than that for the low-grade group (38.2 ± 25.9 seconds vs. 27.9 ± 6.2 seconds, time difference 10.3 seconds, 95% confidence interval: 1.4-19.2 seconds, P < 0.001). However, CVS provided similar high intubation success rates for both groups (97.4% for the high-grade and 100% for the low-grade group). During intubation, visualization of vocal cords and advancement into the glottis for the high-grade group were significantly more difficult than those for the low-grade group.
CONCLUSIONS
Although intubation took longer for patients with higher MCL laryngeal view grade, CVS provided high intubation success rate for patients with severely restricted neck motion and mouth opening regardless of its MCL laryngeal view grade.
MeSH Terms
Figure
Reference
-
1. Mihai R, Blair E, Kay H, Cook TM. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia. 2008; 63:745–60. DOI: 10.1111/j.1365-2044.2008.05489.x. PMID: 18582261.2. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology. 2013; 118:251–70. DOI: 10.1097/ALN.0b013e31827773b2.3. Dalal PG, Dalal GB, Pott L, Bezinover D, Prozesky J, Bosseau Murray W. Learning curves of novice anesthesiology residents performing simulated fibreoptic upper airway endoscopy. Can J Anaesth. 2011; 58:802–9. DOI: 10.1007/s12630-011-9542-2. PMID: 21710368.4. Uchida T, Hikawa Y, Saito Y, Yasuda K. The McCoy levering laryngoscope in patients with limited neck extension. Can J Anaesth. 1997; 44:674–6. DOI: 10.1007/BF03015455. PMID: 9187791.5. Cook TM. A new practical classification of laryngeal view. Anaesthesia. 2000; 55:274–9. DOI: 10.1046/j.1365-2044.2000.01270.x. PMID: 10671848.6. Bein B, Worthmann F, Scholz J, Brinkmann F, Tonner PH, Steinfath M, et al. A comparison of the intubating laryngeal mask airway and the Bonfils intubation fibrescope in patients with predicted difficult airways. Anaesthesia. 2004; 59:668–74. DOI: 10.1111/j.1365-2044.2004.03778.x. PMID: 15200542.7. Kim JK, Kim JA, Kim CS, Ahn HJ, Yang MK, Choi SJ. Comparison of tracheal intubation with the airway scope or clarus video system in patients with cervical collars. Anaesthesia. 2011; 66:694–8. DOI: 10.1111/j.1365-2044.2011.06762.x. PMID: 21564045.8. Cheng WC, Lan CH, Lai HY. The clarus video system (trachway) intubating stylet for awake intubation. Anaesthesia. 2011; 66:1178–80. DOI: 10.1111/j.1365-2044.2011.06948.x. PMID: 22070595.9. Gaszynski T, Gaszynska E. The clarus video system stylet for awake intubation in a very difficult urgent intubation. Anaesthesiol Intensive Ther. 2013; 45:153–4. DOI: 10.5603/AIT.2013.0032. PMID: 24092512.10. Komatsu R, Kamata K, Sessler DI, Ozaki M. A comparison of the airway scope and McCoy laryngoscope in patients with simulated restricted neck mobility. Anaesthesia. 2010; 65:564–8. DOI: 10.1111/j.1365-2044.2010.06334.x. PMID: 20412151.11. Goutcher CM, Lochhead V. Reduction in mouth opening with semi-rigid cervical collars. Br J Anaesth. 2005; 95:344–8. DOI: 10.1093/bja/aei190. PMID: 16006487.12. Pott LM, Murray WB. Review of video laryngoscopy and rigid fiberoptic laryngoscopy. Curr Opin Anaesthesiol. 2008; 21:750–8. DOI: 10.1097/ACO.0b013e3283184227. PMID: 18997526.13. Komatsu R, Kamata K, Hoshi I, Sessler DI, Ozaki M. Airway scope and gum elastic bougie with Macintosh laryngoscope for tracheal intubation in patients with simulated restricted neck mobility. Br J Anaesth. 2008; 101:863–9. DOI: 10.1093/bja/aen288. PMID: 18835885.14. Halligan M, Charters P. A clinical evaluation of the Bonfils intubation fibrescope. Anaesthesia. 2003; 58:1087–91. DOI: 10.1046/j.1365-2044.2003.03407.x. PMID: 14616594.15. Costa F, Mattei A, Massimiliano C, Cataldo R, Agrò FE. The clarus video system as a useful diagnostic tool. Anaesthesia. 2011; 66:135–6. DOI: 10.1111/j.1365-2044.2010.06590.x. PMID: 21254990.16. Seo H, Lee G, Ha SI, Song JG. An awake double lumen endotracheal tube intubation using the clarus video system in a patient with an epiglottic cyst: a case report. Korean J Anesthesiol. 2014; 66:157–9. DOI: 10.4097/kjae.2014.66.2.157. PMID: 24624275. PMCID: PMC3948444.17. Liem EB, Bjoraker DG, Gravenstein D. New options for airway management: intubating fibreoptic stylets. Br J Anaesth. 2003; 91:408–18. DOI: 10.1093/bja/aeg011. PMID: 12925482.18. Lee AR, Yang S, Shin YH, Kim JA, Chung IS, Cho HS, et al. A comparison of the BURP and conventional and modified jaw thrust manoeuvres for orotracheal intubation using the clarus video system. Anaesthesia. 2013; 68:931–7. DOI: 10.1111/anae.12282. PMID: 23841798.19. Thong SY, Wong TG. Clinical uses of the Bonfils retromolar intubation fiberscope: a review. Anesth Analg. 2012; 115:855–66. DOI: 10.1213/ANE.0b013e318265bae2. PMID: 22956530.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cervical Subcutaneous Emphysema Occured by Unexpected Difficult Endotracheal Intubation: A case report
- Comparison between GlideRite® rigid stylet and Parker Flex-It™ stylet to facilitate GlideScope intubation in simulated difficult intubation: a randomized controlled study
- Is the Laryngeal Lift a Useful Maneuver Improving the Laryngoscopic View for Endotracheal Intubation?
- The Clinical Effectiveness of the Bonfils Intubation Fibrescope in Difficult Tracheal Intubation
- Encountering unexpected difficult airway: relationship with the intubation difficulty scale