Investig Clin Urol.
2019 Jan;60(1):35-39. 10.4111/icu.2019.60.1.35.
Evaluation of pain and catheter-related bladder discomfort relative to balloon volumes of indwelling urinary catheters: A prospective study
- Affiliations
-
- 1Department of Urology, Bicêtre Hospital, Le Kremlin-Bicêtre, France. zugail2@hotmail.com
- 2Department of Surgery, Faculty of Medicine in Rabigh, King Abdulaziz University, Jeddah, Saudi Arabia.
- KMID: 2434623
- DOI: http://doi.org/10.4111/icu.2019.60.1.35
Abstract
- PURPOSE
To evaluate patients' tolerance to indwelling urinary catheters (IUCs) before and after reducing their balloon volumes. IUCs are a source of discomfort or pain.
MATERIALS AND METHODS
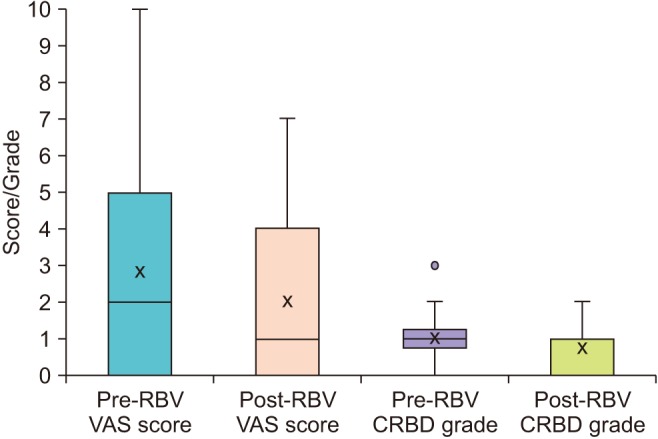
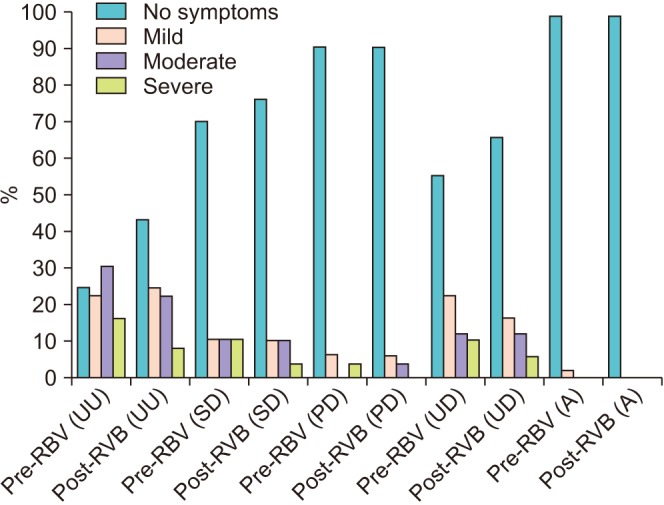
All consecutive patients hospitalized in our department with IUCs were included during the study period with some exclusion. Each patient was his/her own control before and two hours after reduction of the balloon volume (RBV) by half using two types of assessments, a visual analog scale for pain and a catheter-related bladder discomfort (CRBD) symptom questionnaire.
RESULTS
Forty-nine patients were included in our study that completed the assessments. The mean scores for pain before and after RBVs were 2.80 and 2.02, respectively. The difference was significant (p < 0.05). The mean grades of the CRBD before and after RBVs were 1.02 and 0.75, respectively. The difference was significant (p < 0.05).
CONCLUSIONS
A 50% RBV has shown a significant amelioration in tolerating the catheter.
MeSH Terms
Figure
Cited by 1 articles
-
The Novel Method to Reduce Catheter-Related Bladder Discomfort after Transurethral Prostate Surgery
Yu Seob Shin, A Ram Doo, Hyun Jun Park
World J Mens Health. 2020;38(1):137-138. doi: 10.5534/wjmh.190069.
Reference
-
1. Diokno AC, Lapides J. Oxybutynin: a new drug with analgesic and anticholinergic properties. J Urol. 1972; 108:307–309. PMID: 5047425.2. Yarker YE, Goa KL, Fitton A. Oxybutynin. A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic use in detrusor instability. Drugs Aging. 1995; 6:243–262. PMID: 7620236.3. Clmett D, Jarvis B. Tolterodine: a review of its use in the treatment of overactive bladder. Drugs Aging. 2001; 18:277–304. PMID: 11341475.4. Ergenoglu P, Akin S, Yalcin Cok O, Eker E, Kuzgunbay B, Turunc T, et al. Effect of intraoperative paracetamol on catheter-related bladder discomfort: a prospective, randomized, double-blind study. Curr Ther Res Clin Exp. 2012; 73:186–194. PMID: 24653520.
Article5. Agarwal A, Yadav G, Gupta D, Singh PK, Singh U. Evaluation of intra-operative tramadol for prevention of catheter-related bladder discomfort: a prospective, randomized, double-blind study. Br J Anaesth. 2008; 101:506–510. PMID: 18653496.
Article6. Agarwal A, Gupta D, Kumar M, Dhiraaj S, Tandon M, Singh PK. Ketamine for treatment of catheter related bladder discomfort: a prospective, randomized, placebo controlled and double blind study. Br J Anaesth. 2006; 96:587–589. PMID: 16531445.
Article7. Agarwal A, Dhiraaj S, Pawar S, Kapoor R, Gupta D, Singh PK. An evaluation of the efficacy of gabapentin for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled, double blind study. Anesth Analg. 2007; 105:1454–1457. PMID: 17959982.8. Agarwal A, Raza M, Singhal V, Dhiraaj S, Kapoor R, Srivastava A, et al. The efficacy of tolterodine for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Anesth Analg. 2005; 101:1065–1067. PMID: 16192522.
Article9. Tauzin-Fin P, Stecken L, Sztark F. Catheter-related bladder discomfort in post-anaesthesia care unit. Ann Fr Anesth Reanim. 2012; 31:605–608. PMID: 22749555.10. Tauzin-Fin P, Sesay M, Svartz L, Krol-Houdek MC, Maurette P. Sublingual oxybutynin reduces postoperative pain related to indwelling bladder catheter after radical retropubic prostatectomy. Br J Anaesth. 2007; 99:572–575. PMID: 17681969.11. Bai Y, Wang X, Li X, Pu C, Yuan H, Tang Y, et al. Management of catheter-related bladder discomfort in patients who underwent elective surgery. J Endourol. 2015; 29:640–649. PMID: 25335575.
Article12. Agarwal A, Dhiraaj S, Singhal V, Kapoor R, Tandon M. Comparison of efficacy of oxybutynin and tolterodine for prevention of catheter related bladder discomfort: a prospective, randomized, placebocontrolled, double-blind study. Br J Anaesth. 2006; 96:377–380. PMID: 16415311.
Article13. Caulfield MP, Birdsall NJ. International Union of Pharmacology. XVII. Classification of muscarinic acetylcholine receptors. Pharmacol Rev. 1998; 50:279–290. PMID: 9647869.14. Yamanishi T, Chapple CR, Chess-Williams R. Which muscarinic receptor is important in the bladder? World J Urol. 2001; 19:299–306. PMID: 11760777.
Article15. Binhas M, Motamed C, Hawajri N, Yiou R, Marty J. Predictors of catheter-related bladder discomfort in the post-anaesthesia care unit. Ann Fr Anesth Reanim. 2011; 30:122–125. PMID: 21277735.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Bladder Perforation in a Patient with a Long-Term Intraurethral Catheter
- Bladder Management after Total Hip Arthroplasty under Spinal Anesthesia
- Clinical Evaluation of Sterile Intermittent Catheterization in Spinal Cord Injury Patients on Indwelling Catheter Drainage
- Effectiveness of Topical Ofloxacin Ointment for Genitourinary Post-Operative Patients with Urinary Catheterization
- Removal of non-deflatable retained Foley catheter in the bladder by percutaneous puncture of catheter balloon