Healthc Inform Res.
2018 Oct;24(4):346-358. 10.4258/hir.2018.24.4.346.
Bayesian Network Model to Evaluate the Effectiveness of Continuous Positive Airway Pressure Treatment of Sleep Apnea
- Affiliations
-
- 1Department of Public Health and Clinical Nutrition, University of Eastern Finland, Kuopio, Finland. olli-pekka.ryynanen@uef.fi
- 2General Practice & Primary Health Care Unit, Kuopio University Hospital, Kuopio, Finland.
- 3Department of Applied Physics, University of Eastern Finland, Kuopio, Finland.
- 4Department of Clinical Neurophysiology, Kuopio University Hospital, Kuopio, Finland.
- 5Department of Communications and Networking, School of Electrical Engineering, Aalto University, Espoo, Finland.
- 6Institute of Clinical Medicine, Faculty of Health Sciences, University of Eastern Finland, Kuopio, Finland.
- KMID: 2434550
- DOI: http://doi.org/10.4258/hir.2018.24.4.346
Abstract
OBJECTIVES
The association between obstructive sleep apnea (OSA) and mortality or serious cardiovascular events over a long period of time is not clearly understood. The aim of this observational study was to estimate the clinical effectiveness of continuous positive airway pressure (CPAP) treatment on an outcome variable combining mortality, acute myocardial infarction (AMI), and cerebrovascular insult (CVI) during a follow-up period of 15.5 years (186 ± 58 months).
METHODS
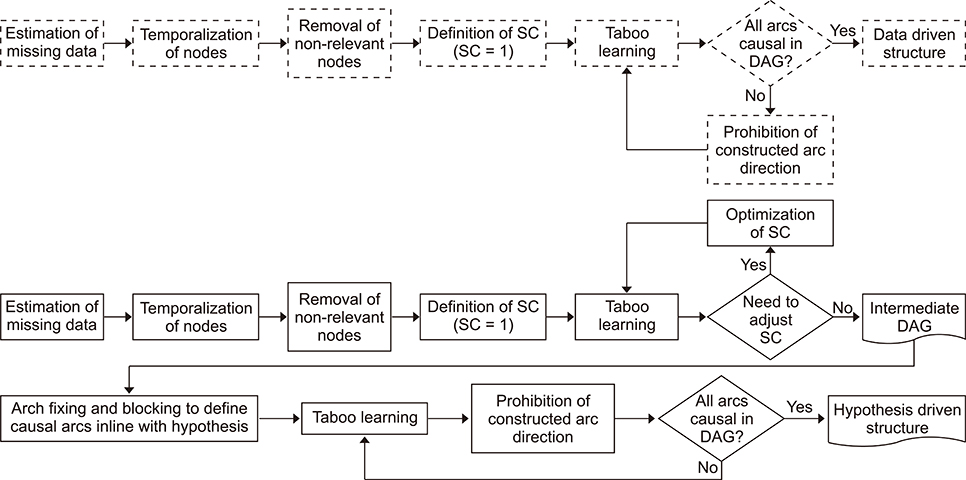
The data set consisted of 978 patients with an apnea-hypopnea index (AHI) ≥5.0. One-third had used CPAP treatment. For the first time, a data-driven causal Bayesian network (DDBN) and a hypothesis-driven causal Bayesian network (HDBN) were used to investigate the effectiveness of CPAP.
RESULTS
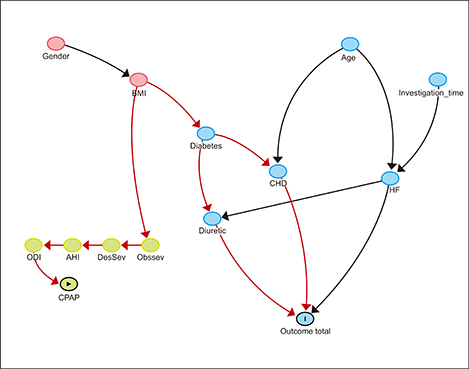
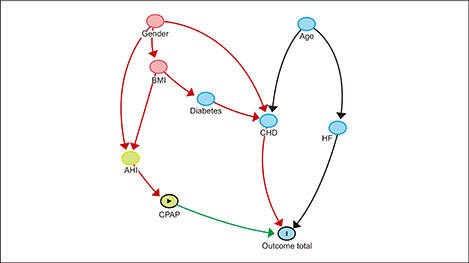
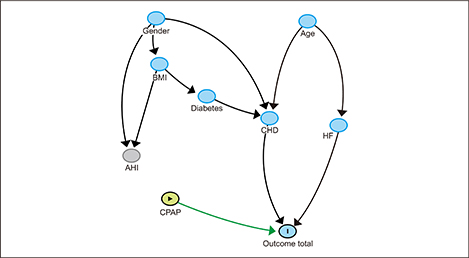
In the DDBN, coronary heart disease (CHD), congestive heart failure (CHF), and diuretic use were directly associated with the outcome variable. Sleep apnea parameters and CPAP treatment had no direct association with the outcome variable. In the HDBN, CPAP treatment showed an average improvement of 5.3 percentage points in the outcome. The greatest improvement was seen in patients aged ≤55 years. The effect of CPAP treatment was weaker in older patients (>55 years) and in patients with CHD. In CHF patients, CPAP treatment was associated with an increased risk of mortality, AMI, or CVI.
CONCLUSIONS
The effectiveness of CPAP is modest in younger patients. Long-term effectiveness is limited in older patients and in patients with heart disease (CHD or CHF).
Keyword
MeSH Terms
Figure
Reference
-
1. Kronholm E, Sallinen M, Suutama T, Sulkava R, Era P, Partonen T. Self-reported sleep duration and cognitive functioning in the general population. J Sleep Res. 2009; 18(4):436–446.
Article2. Muraja-Murro A, Eskola K, Kolari T, Tiihonen P, Hukkanen T, Tuomilehto H, et al. Mortality in middle-aged men with obstructive sleep apnea in Finland. Sleep Breath. 2013; 17(3):1047–1053.
Article3. Rich J, Raviv A, Raviv N, Brietzke SE. All-cause mortality and obstructive sleep apnea severity revisited. Otolaryngol Head Neck Surg. 2012; 147(3):583–587.
Article4. Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005; 353(19):2034–2041.
Article5. Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981; 1(8225):862–865.
Article6. Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006; (1):CD001106.
Article7. Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013; 169(3):207–214.
Article8. Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR. Bayesian methods in health technology assessment: a review. Health Technol Assess. 2000; 4(38):1–130.
Article9. Sheingold SH. Can Bayesian methods make data and analyses more relevant to decision makers? A perspective from Medicare. Int J Technol Assess Health Care. 2001; 17(1):114–122.
Article10. Allmark P. Bayes and health care research. Med Health Care Philos. 2004; 7(3):321–332.
Article11. Woertman W, van der Wilt GJ. Estimating the effectiveness of HPV vaccination in the open population: a Bayesian approach. Value Health. 2013; 16(4):604–609.
Article12. Pearl J. Causality. 2nd ed. Cambridge: Cambridge University Press;2009.13. American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999; 22(5):667–689.14. Kulkas A, Tiihonen P, Eskola K, Julkunen P, Mervaala E, Toyras J. Novel parameters for evaluating severity of sleep disordered breathing and for supporting diagnosis of sleep apnea-hypopnea syndrome. J Med Eng Technol. 2013; 37(2):135–143.
Article15. Kulkas A, Tiihonen P, Julkunen P, Mervaala E, Toyras J. Novel parameters indicate significant differences in severity of obstructive sleep apnea with patients having similar apnea-hypopnea index. Med Biol Eng Comput. 2013; 51(6):697–708.
Article16. Leppanen T, Toyras J, Muraja-Murro A, Kupari S, Tiihonen P, Mervaala E, Kulkas A. length of individual apnea events is increased by supine position and modulated by severity of obstructive sleep apnea. Sleep Disord. 2016; 2016:9645347.17. Muraja-Murro A, Kulkas A, Hiltunen M, Kupari S, Hukkanen T, Tiihonen P, et al. Adjustment of apneahypopnea index with severity of obstruction events enhances detection of sleep apnea patients with the highest risk of severe health consequences. Sleep Breath. 2014; 18(3):641–647.
Article18. Leppanen T, Sarkka M, Kulkas A, Muraja-Murro A, Kupari S, Anttonen M, et al. RemLogic plug-in enables clinical application of apnea-hypopnea index adjusted for severity of individual obstruction events. J Med Eng Technol. 2016; 40(3):119–126.
Article19. Muraja-Murro A, Kulkas A, Hiltunen M, Kupari S, Hukkanen T, Tiihonen P, et al. The severity of individual obstruction events is related to increased mortality rate in severe obstructive sleep apnea. J Sleep Res. 2013; 22(6):663–669.
Article20. BayesiaLab [Internet]. Franklin (TN): Bayesia USA;c2018. cited at 2017 Jul 14. Available from: http://www.bayesialab.com/.21. Kjaerulff UB, Madsen AL. Bayesian networks and influence diagrams. New York (NY): Springer-Verlag;2008.22. Bai X. Tabu search enhanced Markov blanket classifier for high dimensional data sets. Pittsburg (PA): Carnegie Mellon University;2005.23. Grunwald PD. The minimum description length principle. Cambridge (MA): MIT Press;2007.24. Kekolahti P, Karikoski J, Riikonen A. The effect of an individual's age on the perceived importance and usage intensity of communications services: a Bayesian network analysis. Inf Syst Front. 2015; 17(6):1313–1333.
Article25. Kekolahti P, Kilkki K, Hammainen H, Riikonen A. Features as predictors of phone popularity: an analysis of trends and structural breaks. Telematics Inform. 2016; 33(4):973–989.
Article26. Kasza J, Solomon P. Comparing score-based methods for estimating Bayesian networks using the Kullback-Leibler divergence. Commun Stat Theory Methods. 2015; 44(1):135–152.
Article27. Shamilov A, Asan Z, Giriftinoglu C. Estimation by MinxEnt principle. In : Proceedings of the 9th WSEAS International Conference on Applied Mathematics (WSEAS); 2006 May 27-29; Istanbul, Turkey. p. 436–440.28. Friedman N. The Bayesian structural EM algorithm. In : Proceedings of the 14th Conference on Uncertainty in Artificial Intelligence; 1998 Jul 24-26; Madison, WI. p. 129–138.29. Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011; 22(5):745.30. Pearl J, Mackenzie D. The ladder of causation. The book of why: the new science of cause and effect. New York (NY): Basic Books;2018. p. 23–52.31. Kendzerska T, Gershon AS, Hawker G, Leung RS, Tomlinson G. Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: a decade-long historical cohort study. PLoS Med. 2014; 11(2):e1001599.
Article32. Marshall NS, Wong KK, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the Busselton Health Study cohort. J Clin Sleep Med. 2014; 10(4):355–362.
Article33. Meinow B, Kareholt I, Parker MG, Thorslund M. The effect of the duration of follow-up in mortality analysis: the temporal pattern of different predictors. J Gerontol B Psychol Sci Soc Sci. 2004; 59(3):S181–S189.
Article34. Jennum P, Tonnesen P, Ibsen R, Kjellberg J. All-cause mortality from obstructive sleep apnea in male and female patients with and without continuous positive airway pressure treatment: a registry study with 10 years of follow-up. Nat Sci Sleep. 2015; 7:43–50.
Article35. Kasai T, Narui K, Dohi T, Yanagisawa N, Ishiwata S, Ohno M, et al. Prognosis of patients with heart failure and obstructive sleep apnea treated with continuous positive airway pressure. Chest. 2008; 133(3):690–696.
Article36. Gottlieb DJ, Yenokyan G, Newman AB, O'Connor GT, Punjabi NM, Quan SF, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010; 122(4):352–360.
Article37. Cowie MR, Woehrle H, Wegscheider K, Angermann C, d'Ortho MP, Erdmann E, et al. Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med. 2015; 373(12):1095–1105.
Article38. Yogasundaram H, Oudit GY. Increased mortality associated with adaptive servo-ventilation therapy in heart failure patients with central sleep apnea in the halted SERVE-HF Trial. Can J Cardiol. 2015; 31(9):1202–1203.
Article39. Woehrle H, Cowie MR, Eulenburg C, Suling A, Angermann C, d'Ortho MP, et al. Adaptive servo ventilation for central sleep apnoea in heart failure: SERVE-HF on-treatment analysis. Eur Respir J. 2017; 50(2):1601692.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Massive REM Rebound on Continuous Positive Airway Pressure in Obstructive Sleep Apnea
- The Role of Endothelin-1 in Obstructive Sleep Apnea Syndrome and Pulmonary Hypertension
- CPAP Treatment in Pediatric Obstructive Sleep Apnea
- Treatment of Obstructive Sleep Apnea with Positive Pressure Ventilation
- Obstructive Sleep Apnea of Achondroplasia Treated With Continuous Positive Airway Pressure