J Korean Neurosurg Soc.
2019 Jan;62(1):53-60. 10.3340/jkns.2017.0287.
Clinical Efficacy of Intra-Operative Cell Salvage System in Major Spinal Deformity Surgery
- Affiliations
-
- 1Department of Neurosurgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
- 2Department of Neurosurgery, Spine Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. hyunsj@snu.ac.kr
- KMID: 2434346
- DOI: http://doi.org/10.3340/jkns.2017.0287
Abstract
OBJECTIVE
The purpose of this study was to determine the efficacy of intra-operative cell salvage system (ICS) to decrease the need for allogeneic transfusions in patients undergoing major spinal deformity surgeries.
METHODS
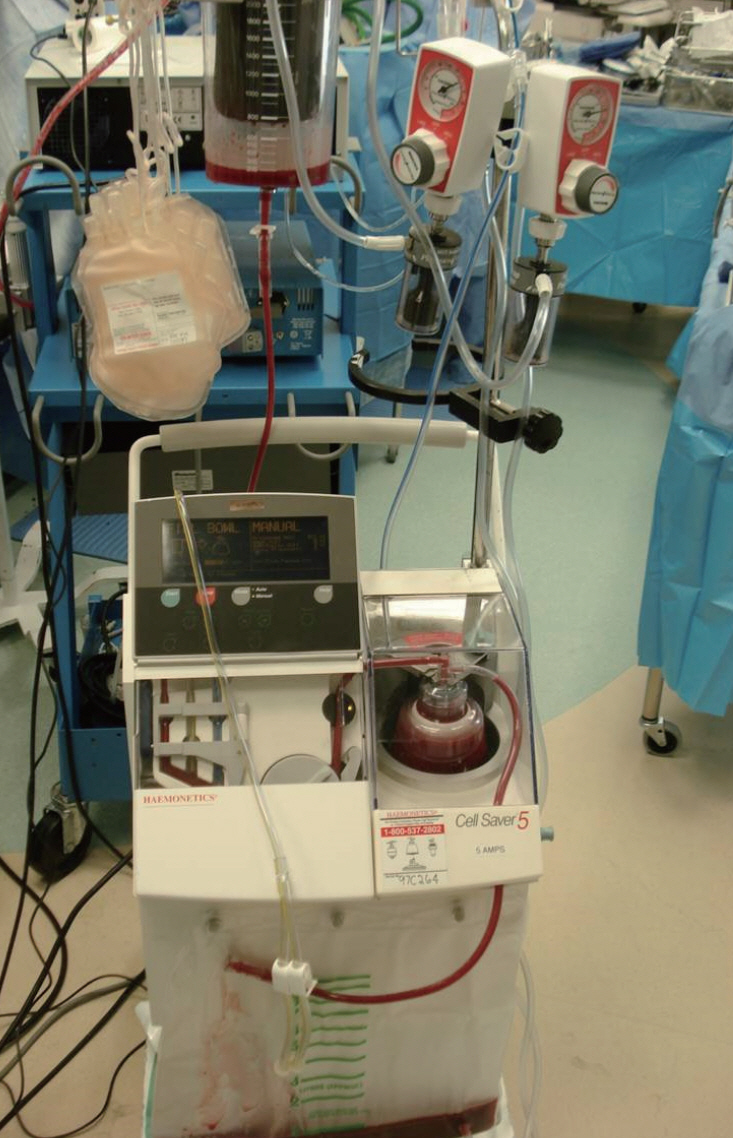
A total of 113 consecutive patients undergoing long level posterior spinal segmental instrumented fusion (≥5 levels) for spinal deformity correction were enrolled. Data including the osteotomy status, the number of fused segments, estimated blood loss, intra-operative transfusion amount by ICS (Cell Saver®, Haemonetics©, Baltimore, MA, USA) or allogeneic blood, postoperative transfusion amount, and operative time were collected and analyzed.
RESULTS
The number of patients was 81 in ICS group and 32 in non-ICS group. There were no significant differences in demographic data and comorbidities between the groups. Autotransfusion by ICS system was performed in 53 patients out of 81 in the ICS group (65.4%) and the amount of transfused blood by ICS was 226.7 mL in ICS group. The mean intra-operative allogeneic blood transfusion requirement was significantly lower in the ICS group than non-ICS group (2.0 vs. 2.9 units, p=0.033). The regression coefficient of ICS use was -1.036.
CONCLUSION
ICS use could decrease the need for intra-operative allogeneic blood transfusion. Specifically, the use of ICS may reduce about one unit amount of allogeneic transfusion in major spinal deformity surgery.
MeSH Terms
Figure
Reference
-
References
1. Ashworth A, Klein AA. Cell salvage as part of a blood conservation strategy in anaesthesia. Br J Anaesth. 105:401–416. 2010.
Article2. Berenholtz SM, Pronovost PJ, Mullany D, Garrett E, Ness PM, Dorman T, et al. Predictors of transfusion for spinal surgery in Maryland, 1997 to 2000. Transfusion. 42:183–189. 2002.
Article3. Bess RS, Lenke LG, Bridwell KH, Steger-May K, Hensley M. Wasting of preoperatively donated autologous blood in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 31:2375–2380. 2006.
Article4. Bowen RE, Gardner S, Scaduto AA, Eagan M, Beckstead J. Efficacy of intraoperative cell salvage systems in pediatric idiopathic scoliosis patients undergoing posterior spinal fusion with segmental spinal instrumentation. Spine (Phila Pa 1976). 35:246–251. 2010.
Article5. Carless PA, Henry DA, Moxey AJ, O’Connell DL, Brown T, Fergusson DA. Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. (4):CD001888. 2006.
Article6. Cole JW, Murray DJ, Snider RJ, Bassett GS, Bridwell KH, Lenke LG. Aprotinin reduces blood loss during spinal surgery in children. Spine (Phila Pa 1976). 28:2482–2485. 2003.
Article7. Domen RE. Adverse reactions associated with autologous blood transfusion : evaluation and incidence at a large academic hospital. Transfusion. 38:296–300. 1998.
Article8. Fong J, Gurewitsch ED, Kang HJ, Kump L, Mack PF. An analysis of transfusion practice and the role of intraoperative red blood cell salvage during cesarean delivery. Anesth Analg. 104:666–672. 2007.
Article9. Gause PR, Siska PA, Westrick ER, Zavatsky J, Irrgang JJ, Kang JD. Efficacy of intraoperative cell saver in decreasing postoperative blood transfusions in instrumented posterior lumbar fusion patients. Spine (Phila Pa 1976). 33:571–575. 2008.
Article10. Gill JB, Chin Y, Levin A, Feng D. The use of antifibrinolytic agents in spine surgery. a meta-analysis. J Bone Joint Surg Am. 90:2399–2407. 2008.11. Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ. Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine. 14:126–132. 2017.
Article12. Kelly PD, Parker SL, Mendenhall SK, Bible JE, Sivasubramaniam P, Shau DN, et al. Cost-effectiveness of cell saver in short-segment lumbar laminectomy and fusion (≤3 levels). Spine (Phila Pa 1976). 40:E978–E985. 2015.
Article13. Keverline JP, Sanders JO. Hematuria associated with low-volume cell saver in pediatric orthopaedics. J Pediatr Orthop. 18:594–597. 1998.
Article14. Kwon JW, Hyun SJ, Han SH, Kim KJ, Jahng TA. Pyogenic vertebral osteomyelitis: clinical features, diagnosis, and treatment. Korean J Spine. 14:27–34. 2017.
Article15. Lee BH, Hyun SJ, Park JH, Kim KJ. Single stage posterior approach for total resection of presacral giant schwannoma : a technical case report. Korean J Spine. 14:89–92. 2017.
Article16. Lennon RL, Hosking MP, Gray JR, Klassen RA, Popovsky MA, Warner MA. The effects of intraoperative blood salvage and induced hypotension on transfusion requirements during spinal surgical procedures. Mayo Clin Proc. 62:1090–1094. 1987.
Article17. Liang J, Shen J, Chua S, Fan Y, Zhai J, Feng B, et al. Does intraoperative cell salvage system effectively decrease the need for allogeneic transfusions in scoliotic patients undergoing posterior spinal fusion? a prospective randomized study. Eur Spine J. 24:270–275. 2015.
Article18. Murray DJ, Gress K, Weinstein SL. Coagulopathy after reinfusion of autologous scavenged red blood cells. Anesth Analg. 75:125–129. 1992.
Article19. Neilipovitz DT. Tranexamic acid for major spinal surgery. Eur Spine J. 13 Suppl 1:S62–S65. 2004.
Article20. Nuttall GA, Horlocker TT, Santrach PJ, Oliver WC Jr, Dekutoski MB, Bryant S. Predictors of blood transfusions in spinal instrumentation and fusion surgery. Spine (Phila Pa 1976). 25:596–601. 2000.
Article21. Ovadia D, Luger E, Bickels J, Menachem A, Dekel S. Efficacy of closed wound drainage after total joint arthroplasty. a prospective randomized study. J Arthroplasty. 12:317–321. 1997.22. Paravicini D, Schmitz-Huebner U, Stinnesbeck B. Heparin elimination in intraoperative autotransfusion with the haemonetics cell saver. Infusionsther Klin Ernahr. 10:19–21. 1983.
Article23. Park YS, Hyun SJ, Kim KJ, Jahng TA. Multiple intradural disc herniations masquerading as intradural extramedullary tumors: a case report and review of the literature. Korean J Spine. 13:30–32. 2016.
Article24. Park MJ, Roberts CP, Hay D. Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 86-A:1146–1152. 2004.25. Serrick CJ, Scholz M, Melo A, Singh O, Noel D. Quality of red blood cells using autotransfusion devices: a comparative analysis. J Extra Corpor Technol. 35:28–34. 2003.26. Sharp WV, Stark M, Donovan DL. Modern autotransfusion. experience with a washed red cell processing technique. Am J Surg. 142:522–524. 1981.27. Sistino JJ, Owitz D, Mongero LB. Heparin washout in the pediatric cell saver bowl. J Extra Corpor Technol. 24:94–96. 1992.28. Urban MK, Beckman J, Gordon M, Urquhart B, Boachie-Adjei O. The efficacy of antifibrinolytics in the reduction of blood loss during complex adult reconstructive spine surgery. Spine (Phila Pa 1976). 26:1152–1156. 2001.
Article29. Vorweg M, Muckel G, Knüttgen D, Schindler A, Doehn M. Heparin-induced coagulation disturbance from mechanical autotransfusion. Anaesthesist. 47:979–981. 1998.30. Waters JH, Dyga RM, Waters JF, Yazer MH. The volume of returned red blood cells in a large blood salvage program: where does it all go? Transfusion. 51:2126–2132. 2011.
Article31. Weiss JM, Skaggs D, Tanner J, Tolo V. Cell saver: is it beneficial in scoliosis surgery? J Child Orthop. 1:221–227. 2007.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Blood Salvage and Transfusion During Spinal Surgery
- Role of Intraoperative Red Cell Salvage and Autologus Transfusion in Metastatic Spine Surgery: A Pilot Study and Review of Literature
- Effectiveness and Safety of Tranexamic Acid in Spinal Deformity Surgery
- Perioperative Blood Management: Pros and Cons of ANH and Cell Salvage
- Surgical Correction of Adult Spinal Deformity